Open Access | Commentary
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
New insights into the pain symptoms of chronic prostatitis/ chronic pelvic pain syndrome (CP/CPPS): the role of musculoskeletal ultrasound
* Corresponding author: Yifeng Shen
Mailing address: Department of Andrology, Chengdu University of Traditional Chinese Medicine Affiliated Reproductive and Maternity Hospital, Chengdu, 610000, China.
Email: shen.yifeng@foxmail.com
Received: 08 December 2025 / Accepted: 11 December 2025 / Published: 30 December 2025
DOI: 10.31491/UTJ.2025.12.049
Abstract
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) represents a prevalent and highly debilitating urological disorder that significantly impairs the quality of life of male patients. Conventional monomodal pharmacological interventions have demonstrated limited efficacy, primarily due to the intricate and not fully elucidated etiology of the disease. This article focuses on the pivotal discoveries derived from musculoskeletal ultrasound - guided examinations in CP/CPPS patients. Our findings indicate that inflammatory edema within the suprapubic muscles is the principal etiological factor for lower abdominal pain, while inflammatory edema and calcification in the perineal pelvic floor muscles are responsible for perineal pain. These revelations have precipitated a paradigm shift towards a multimodal treatment approach, with the overarching goal of enhancing clinical outcomes and improving the quality of life of patients.
Keywords
Prostatitis, CP/CPPS, musculoskeletal ultrasound
Introduction
Prostatitis is a multifaceted urological condition that encompasses infectious prostatitis, asymptomatic prostatitis, and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Among these subtypes, CP/CPPS is the most prevalent, accounting for approximately 90-95% of all prostatitis cases. This syndrome is characterized by a cluster of distressing symptoms, including persistent pelvic pain, urinary dysfunction, and sexual symptoms, all of which severely compromise the quality of life of male patients. By definition, CP/CPPS involves pelvic pain or discomfort that persists for at least 3 months, often accompanied by urinary symptoms such as increased urinary frequency [1]. A comprehensive understanding of the full spectrum of its pain symptoms is of paramount importance. In this context, musculoskeletal ultrasound emerges as a potent diagnostic tool that offers novel and invaluable insights, which will be explored in the subsequent sections.
Musculoskeletal ultrasound examinations: a new perspective
In our research endeavors, we employed musculoskeletal ultrasound examinations to gain a more profound understanding of the pain symptoms in CP/CPPS patients. Musculoskeletal ultrasound is a non - invasive imaging modality capable of providing real-time, high-resolution images of soft tissues, including muscles, tendons, and ligaments. By utilizing this technique, we were able to directly visualize the anatomical structures and pathological alterations in the relevant muscle groups associated with CP/CPPS related pain.
Detailed findings in the muscles of the pubic region
Visualization of inflammatory edema link to lower abdominal pain
Under the guidance of musculoskeletal ultrasound, we clearly observed inflammatory edema in the muscles of the pubic region in CP/CPPS patients. The Pyramidal muscles and rectus abdominis, situated in the lower abdominal region just superior to the pubic bone, play a crucial role in supporting the pelvic organs and maintaining lower abdominal stability. In patients with CP/CPPS, ultrasound images revealed increased fluid accumulation within these muscles, resulting in a swollen and hypoechoic appearance. The hypoechoic areas indicated the presence of excess fluid, which is a characteristic sign of inflammation (Figure 1).
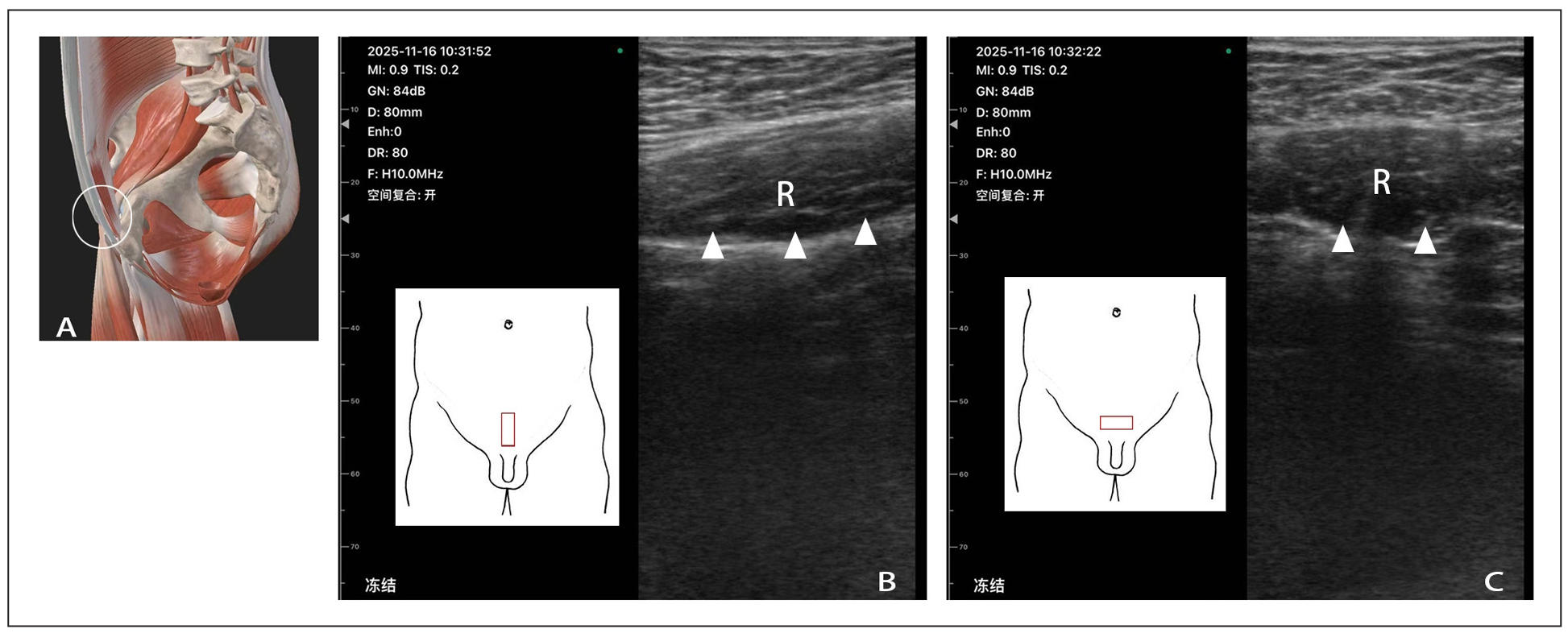
Figure 1. Musculoskeletal ultrasound scan in the muscles of the pubic region. (A) schematic diagram of anatomical structure; (B) abdominal longitudinal probe scanning; (C) abdominal transverse probe scanning; R: rectus abdominis; the white triangle refers to the area of inflammation and edema. The white circle represents the anatomical structure of the ultrasound scanning area. The red square represents the placement position of the probe
This inflammatory edema in the suprapubic muscles is directly correlated with the lower abdominal pain and discomfort frequently reported by patients. The increased fluid within the muscles exerts pressure on the surrounding nerves and tissues, stimulating the pain receptors. Consequently, patients experience a dull, aching, or sometimes sharp pain in the lower abdomen. We observed that this phenomenon is prevalent in the vast majority of patients who complain of lower abdominal pain. We speculate that prolonged sitting, during which the abdomen folds and compresses at the pubic bone, may be a contributing factor, and this compression can occur regardless of the patient's body weight. It can be alleviated through local muscle relaxation or rectus abdominis muscle stretching exercises. In the past, this pain was often misattributed to factors related to the prostate gland itself, such as prostatic inflammation or congestion. However, our musculoskeletal ultrasound findings have unveiled that suprapubic muscle pathology is an important and frequently overlooked cause of lower abdominal pain in CP/CPPS patients.
In depth analysis of perineal pelvic floor muscles
Identification of inflammatory edema and calcification association with perineal pain
The pelvic floor muscles in the perineal region of CP/CPPS patients also exhibited significant pathological changes under musculoskeletal ultrasound examination. In addition to inflammatory edema, which was similar to that observed in the muscles of the pubic region, we also detected calcification in some patients. The inflammatory edema in the perineal pelvic floor muscles presented as swollen and hypoechoic areas, while the calcification appeared as bright, echogenic foci within the muscle tissue. These echogenic foci represented the deposition of calcium salts, which can occur as a result of chronic inflammation and tissue damage (Figure 2).
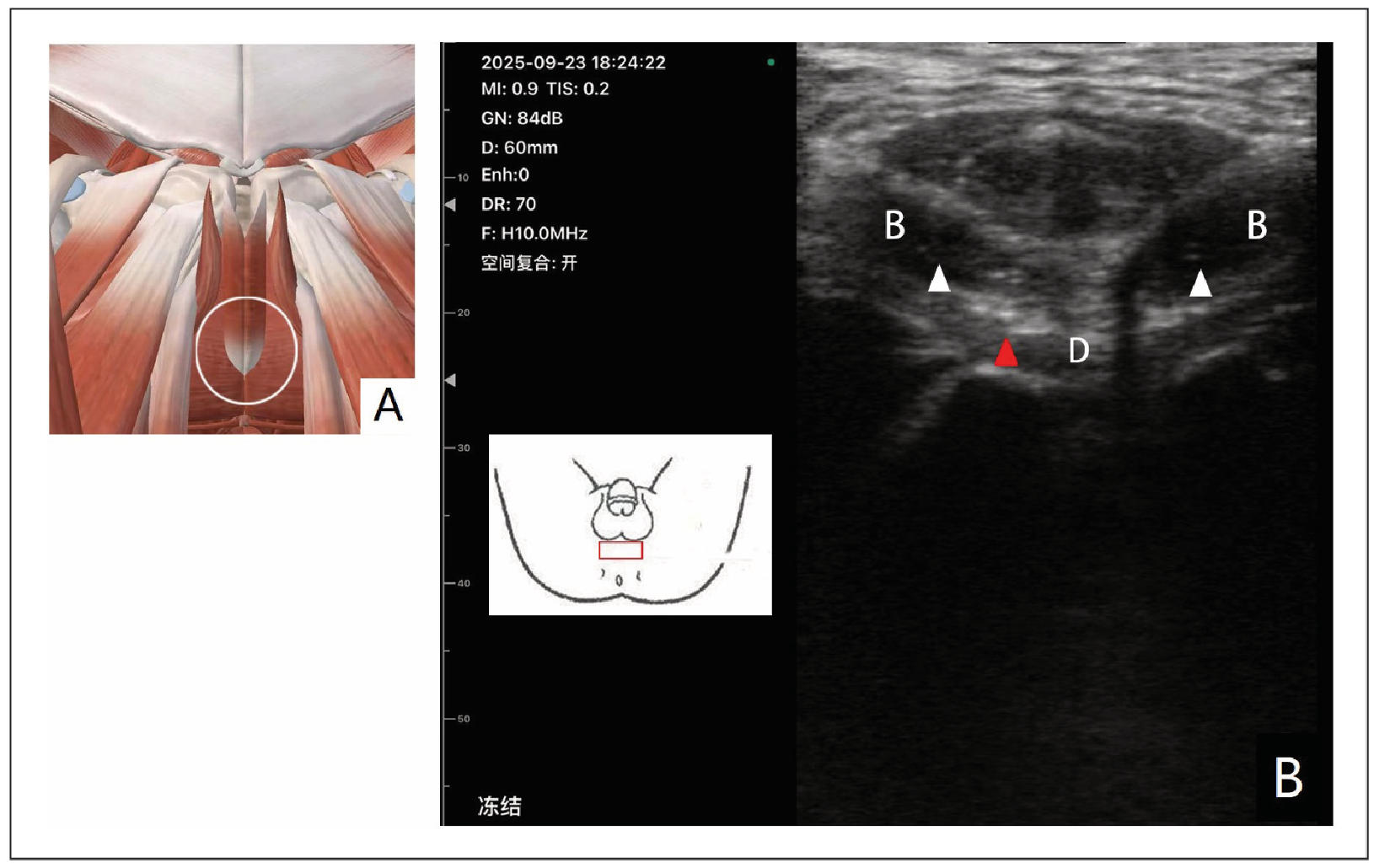
Figure 2. Musculoskeletal ultrasound scan in the perineal area (A) schematic diagram of anatomical structure; (B) ultrasound image of perineal muscle; the white triangle refers to the area of inflammation and edema. The white circle represents the anatomical structure of the ultrasound scanning area. The red square represents the placement position of the probe; the red triangle refers to the calcified area. B, Bulbospongiosus; D, Deep transverse perineal
The perineum is a highly sensitive area, and any pathological changes in the pelvic floor muscles in this region can cause severe perineal pain. The inflammatory edema can directly irritate the pain receptors in the perineal skin and underlying tissues, leading to a burning, stinging, or throbbing pain. The calcification, on the other hand, can cause mechanical irritation and compression of the surrounding nerves and blood vessels, further exacerbating the pain. This perineal pain is a common and distressing symptom for CP/CPPS patients, and its direct link to muscle pathology, as revealed by musculoskeletal ultrasound, was previously overlooked. At the same time, some patients complain of numbness or burning symptoms in the perineum due to prolonged sitting, which is closely related to the compression of the perineal nerve at the ischial tuberosity. It is necessary to release this nerve compression point.
Musculoskeletal ultrasound: a revolutionary force in cp/cpps understanding and treatment
The etiology of chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) is highly intricate and remains incompletely understood, which has long been a significant barrier to the effectiveness of monomodal therapy. In the past, limited knowledge of pain mechanisms in CP/CPPS patients led to the widespread use of single-drug therapies. These well-studied pharmacological options included antibiotics, alpha -blockers, anti-inflammatory and immunomodulatory agents, phytotherapies, phosphodiesterase inhibitors, hormonal agents, neuromodulatory agents, and antidepressants. However, due to the multi-factorial nature of CP/CPPS, these single-drug methods consistently failed to deliver satisfactory clinical results as they were unable to comprehensively address the disease.
Musculoskeletal ultrasound has emerged as a gamechanger, completely revolutionizing our understanding and treatment of CP/CPPS pain. It offers direct and clear visualization of the muscle pathology associated with CP/CPPS, challenging and updating our traditional view of prostatitis pain. Traditionally, prostatitis pain was mainly thought to be caused by prostate-related factors such as inflammation or congestion within the gland itself. However, musculoskeletal ultrasound-guided findings have uncovered that muscle pathology, such as inflammatory edema in the muscles of the pubic region and the perineal pelvic floor muscles, along with calcification in the latter, plays a crucial role in causing lower abdominal and perineal pain. This empirical research evidence has shifted our focus from solely the prostate to the surrounding muscular structures. As a result, there has been a significant shift from monomodal to multimodal treatment strategies. Alongside existing pharmacological therapies, non-pharmacological approaches are gaining increasing prominence. Well studied non-pharmacological methods include pelvic floor physical therapy, myofascial trigger point release, acupuncture and electroacupuncture, electrocorporeal shockwave therapy, and local thermotherapy [2]. With musculoskeletal ultrasound, we can now perform ultrasound guided pain treatment techniques for CP/CPPS, enabling more precise identification of treatment targets. These non-pharmacological therapies can directly act on the muscle pathology identified by musculoskeletal ultrasound, reducing muscle tension, alleviating inflammation,and improving muscle function. By integrating pharmacological and non - pharmacological therapies, a more comprehensive and effective treatment plan can be formulated for CP/CPPS patients, which is expected to significantly improve their clinical symptoms and quality of life.
Conclusions
The utilization of musculoskeletal ultrasound-guided examinations has provided us with novel and direct evidence regarding the pain symptoms of CP/CPPS patients. Inflammatory edema in the suprapubic muscles and inflammatory edema and calcification in the perineal pelvic floor muscles are important etiological factors for lower abdominal and perineal pain, respectively. These findings have challenged the traditional view of CP/CPPS treatment and underscore the necessity for a multimodal approach. By integrating different treatment modalities, we can better address the complex pathological changes in CP/CPPS patients and improve their overall well-being. Further research is warranted to optimize the multimodal treatment strategies and enhance the long term prognosis of CP/CPPS patients.
Declarations
Availability of data and materials
Not applicable.
Financial support and sponsorship
Financial support and sponsorship: Youth Project of National Natural Science Foundation of China (82405413); Joint Innovation Fund of Chengdu Municipal Health Commission and University Committee (WXLH202403298, WXLH2024031656).
Conflicts of interest
Not applicable.
Ethical Approval and Informed consent
Not applicable.
Consent for publication
Not applicable.
References
1. Borgert B, Wallen E, & Pham M. Prostatitis: a review. JAMA, 2025, 334(11): 1003-1013. [Crossref]
2. Pirola G, Verdacchi T, Rosadi S, Annino F, & De Angelis M. Chronic prostatitis: current treatment options. Res Rep Urol, 2019, 11: 165-174. [Crossref]