Open Access | Research
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
An original instrument for diagnosing inflammation of the paraurethral glands in women
Mailing address: Military Medical Academy S. M. Kirov, 6, Academician Lebedev str, Saint-Petersburg, 194044, Russia.
Email: iglovikov@yandex.ru
Received: 31 March 2025 / Revised: 30 April 2025 / Accepted: 21 May 2025 / Published: 25 June 2025
DOI: 10.31491/UTJ.2025.06.037
Abstract
Purpose: The aim of this study was to enhance examination
outcomes for patients with chronic skeneitis through the clinical evaluation
of a specialized retractor designed for the instrumental assessment of the
urethra and skene’s glands.
Materials and Methods: This prospective study involved 55
female participants aged 19 to 38 years, all diagnosed with skeneitis.
The examinations were conducted from 2020 to 2024, and the mean duration
of the disease among the participants was 8.4 ± 3.1 years. Each participant
underwent two distinct physical examinations of the urethra: the first
utilizing forceps and the second employing a novel instrument, with a
one-week interval between assessments. The diagnostic efficacy of
these examinations was evaluated based on several parameters: the
duration of the examination, the condition of the urethral mucosa
(noted for hyperemia and/or infiltration), and the number of
identifiable SG ducts.
Results: The use of the urethral speculum significantly
reduced examination time by 51.6% (P < 0.001) and increased the number
of identified ducts by 1.55 times (P < 0.001), indicating its high
diagnostic efficacy. Additionally, the application of this speculum
decreased pain levels by 2.3 times (P < 0.001) and significantly
reduced hematuria post-examination by 41.8% (P < 0.001), confirming
its enhanced safety profile.
Conclusion: The implementation of this original urethral
viewing speculum represents an innovative, effective, and atraumatic
method for visualizing the urinary tract in women with suspected skeneitis.
Keywords
Paraurethral ducts and glands in women, skene's glands, skineitis, chronic skineitis, recurrent cystourethritis, female urethra, original urethral speculum
Introduction
The term "skeneitis" currently refers to the nonspecific catarrhal
inflammation of the paraurethral glands in women, specifically
skene’s glands (SG), leading to symptoms such as dysuria, pain,
burning sensations, cramping in the urethra, and increased urinary
frequency [1-5].
The anatomical significance of the paraurethral ducts and glands
was established in 1880 by the American gynecologist Alexander
Johnston Chalmers Skene, who documented them in his seminal work,
"Anatomy and Pathology of Two Important Glands of the Female
Urethra." He remarked, "When I first discovered these glands,
I presumed that they were mucous follicles that were accidentally
of unusual size in the subject examined. However, after investigating
more than one hundred such glands across various subjects and consistently
finding them present and uniform in size and location, I became convinced
that they warranted a distinct place in descriptive anatomy" [6].
Skene hypothesized that the painful inflammation of the meatus in
his patient was perpetuated by infected vaginal secretions,
and although he hoped that treatment would sanitize the urethral
canal, the outcome was unsuccessful. During examination, he observed
two cavities filled with yellowish-gray material resembling unhealed
ulcers on either side of the meatus after prolonged treatment. Notably,
he found that these formations allowed for the passage of more than
half an inch (1.27 cm). Upon applying pressure to the urethra after
instrument removal, he noted the expulsion of purulent fluid from
these openings. Subsequent treatment focused on these structures,
leading to the patient’s full recovery within two months following
the correct diagnosis. Skene identified gonococcal inflammation as
a significant pathological condition affecting these anatomical structures.
According to A.G. Glukharev, skeneitis may be the primary etiology of
recurrent lower urinary tract infections (UTIs) in up to 50% of cases [5].
Clinical studies have indicated that skeneitis, along with its complications
such as cysts and diverticula of the urethra, ranks as the fifth most prevalent
cause of persistent dysuric disorders in women [7]. Despite the high prevalence
of SG inflammation, standardized guidelines for the diagnosis and treatment of
suspected cases remain lacking.
Currently, standardized diagnostic criteria for chronic skeneitis remain undefined.
However, clinical studies suggest that inflammatory signs in the affected anatomical
structures may include tenderness upon transvaginal palpation in the distal and/or
middle urethral third, as well as erythema and edema of the skene’s gland ducts
upon instrumental examination, accompanied by pain during probing. [1-3, 8, 9].
The absence of a dedicated urethral retractor and reliance on improvised surgical
instruments (such as forceps or tweezers) complicate examinations, leading to
significant patient discomfort and inadequate visualization of the urethral walls
and targeted structures [10-12]. Thus, a standardized diagnostic tool for skeneitis
is urgently needed in urological practice, both in outpatient and inpatient settings.
The aim of the study was to improve the examination outcomes for patients
with chronic skeneitis by developing and clinically evaluating a specialized
retractor for the instrumental examination of the urethra and skene's glands.
Materials and methods
This prospective study involved 55 female participants
aged 19 to 38 years, all with a preliminary diagnosis of skeneitis.
Patients were examined between 2020 and 2024, with a mean disease
duration of 8.4 ± 3.1 years. The diagnosis was based on clinical complaints,
medical history, and transvaginal palpation of the urethra, which revealed
localized pain in the distal and middle thirds, corresponding to the
location of skene’s glands (SG). A comprehensive diagnostic evaluation
was conducted to exclude other causes of dysuria.
The primary complaints reported during the initial interview
included constant or intermittent urethral pain, dysuria,
burning sensations during urination, pollakiuria, dyspareunia,
and recurrent urinary tract infections (including postcoital cystitis).
Notably, 18 (32%) respondents could not identify the cause of their
condition; 22 (40%) attributed it to the onset of sexual activity,
while 15 (27.3%) linked it to a prior episode of acute cystitis.
Additionally, 10 (18.1%) patients had previously undergone transurethral
resection of the bladder for leukoplakia 2 to 5 years prior, without
significant relief.
All participants were of reproductive age, with 8 (14.5%) abstaining
from sexual intercourse and 28 (50.9%) limiting their sexual activity.
A history of gynecological conditions was reported by 34 (61.8%) participants,
including vaginitis in 13 (23.6%), cervical erosion in 9 (16.4%), colpitis
in 7 (12.7%), uterine fibroids in 1 (1.8%), and ovarian cysts in 6 (10.9%).
Contraceptive methods employed included interrupted intercourse in 20 (36.4%),
oral contraceptives in 26 (47.2%), intrauterine devices in 2 (4%), and barrier
methods in 7 (12.7%).
Exclusion criteria included pregnancy, acute or chronic infections
of the upper and lower urinary tracts and reproductive organs at the
time of diagnosis, urethral cysts and diverticula, malignancies, benign
lesions, chronic pelvic pain syndrome, and refusal to participate in the
study. The study adhered to the principles of Helsinki Declaration.
Informed consent was obtained by all subjects when they were enrolled.
Each patient underwent two physical examinations of the urethra:
the first using standard techniques with forceps and the second with
an original instrument (Figure 1), with a one-week interval between
assessments. To ensure objectivity, 28 participants were assessed in
the aforementioned order, while the remaining 27 underwent evaluations
in reverse order.
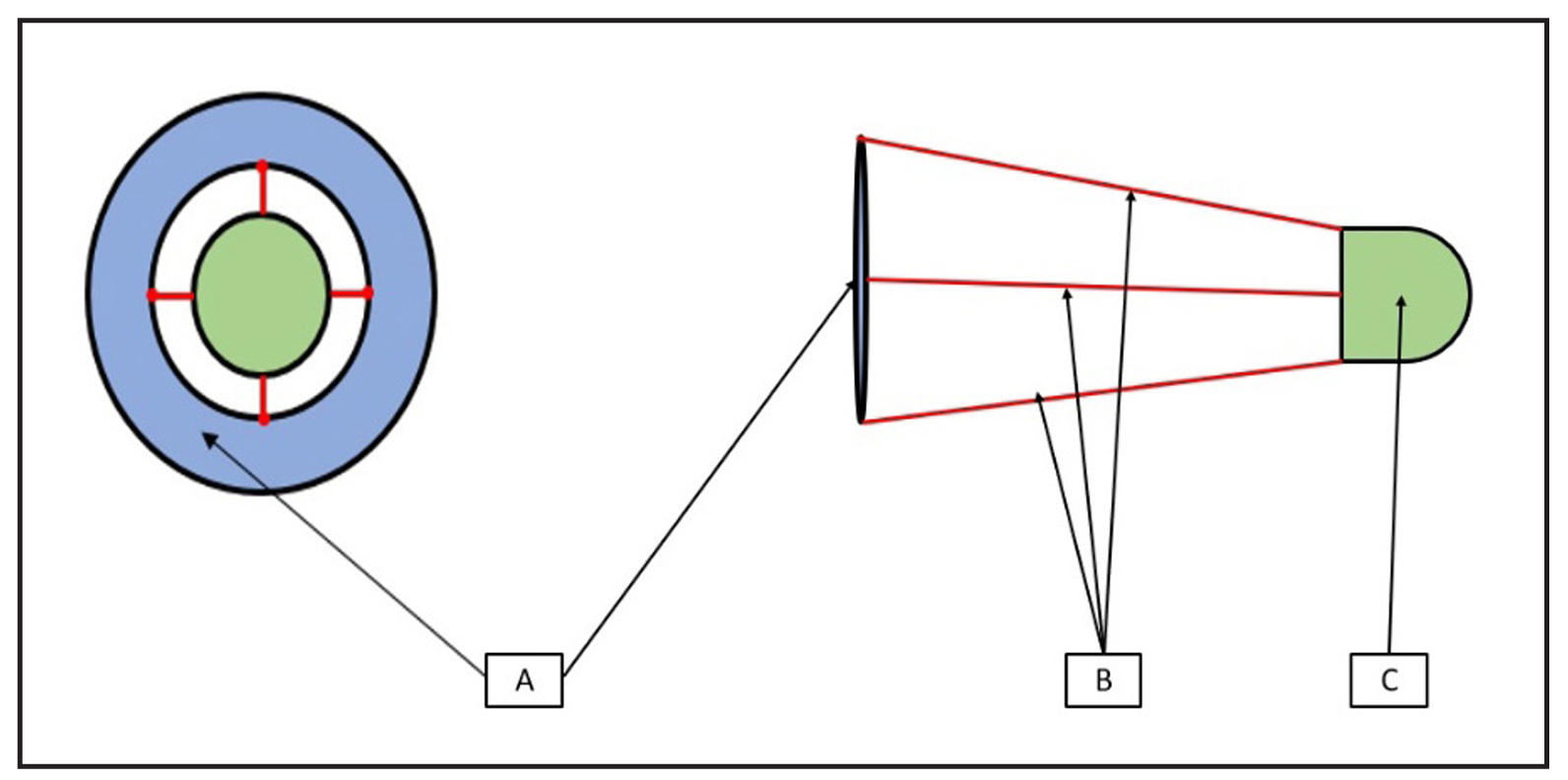
Figure 1. Schematic representation of the urethral viewing speculum (A–outer ring, B–rigidity ribs, C–obturator tip).
The examination procedure included bladder emptying, positioning
the patient in the Lloyd-Davies position, cleansing the external
genitalia, inserting the instrument into the urethra, and inspecting
the urethral mucosa.
The following parameters were evaluated:
1) Examination time (seconds);
2) Condition of the urethral mucosa (hyperemia and/or infiltration; yes/no);
3) Number of identified ducts of the SG (count);
4) Pain severity assessed using the visual analog scale (VAS; scores ranging from 0 to 10);
5) Presence of hematuria (defined as more than 10 erythrocytes per field of
view) in urinalysis collected immediately after examination (yes/no).
Parameters 1, 2, and 3 were considered indicators of diagnostic
effectiveness, while the last two parameters were associated with
examination safety. The number of identified ducts was critical
for surgical planning, as missed ducts during electrosurgical
resection of the SG are a primary factor in disease recurrence
and subsequent interventions. Hematuria was regarded as an indicator
of potential trauma to the urethral mucosa. The local status was
assessed by a single physician with over 10 years of experience
managing this pathology, who had access to the initial examination
data after completing the second procedure.
Data were statistically analyzed using STATISTICA version 10.0 and
Python programming version 3.11.6. For features exhibiting non-normal
distribution, the median (Me) and interquartile range (Q1 – Q3) were
calculated. Categorical data were presented as absolute values and
percentages. The Wilcoxon non-parametric test was employed to evaluate
the statistical significance of differences in continuous variables,
while comparisons of binary indicators were performed using the McNemar
test for chi-square (x2) analysis. Differences were considered statistically
significant at a p-value of < 0.05.
Results
To address the study's objective, an original instrument—a urethral viewing speculum—was developed (Patent for invention RU No. 2790762 C1, dated February 28, 2023). This innovative device is composed of surgical stainless steel and includes an outer ring, four rigidity ribs, and a 3 cm long obturator tip. The outer ring is designed to prevent migration of the instrument into the urethra or bladder cavity, while the rigidity ribs, positioned at the 12, 3, 6, and 9 o'clock positions, allow for internal extension of the urethra in four directions, facilitating examination of the mucosa and the orifices of the SG ducts. The speculum can be rotated during the examination to assess obscured areas and to adjust the tilt angle for visualizing the anterior wall. Its conical shape, with a gradual decrease in diameter from the outer ring to the obturator tip, minimizes discomfort during the diagnostic process. The rounded end of the obturator tip ensures safe and atraumatic insertion and removal of the instrument (Figure 1 & 2).
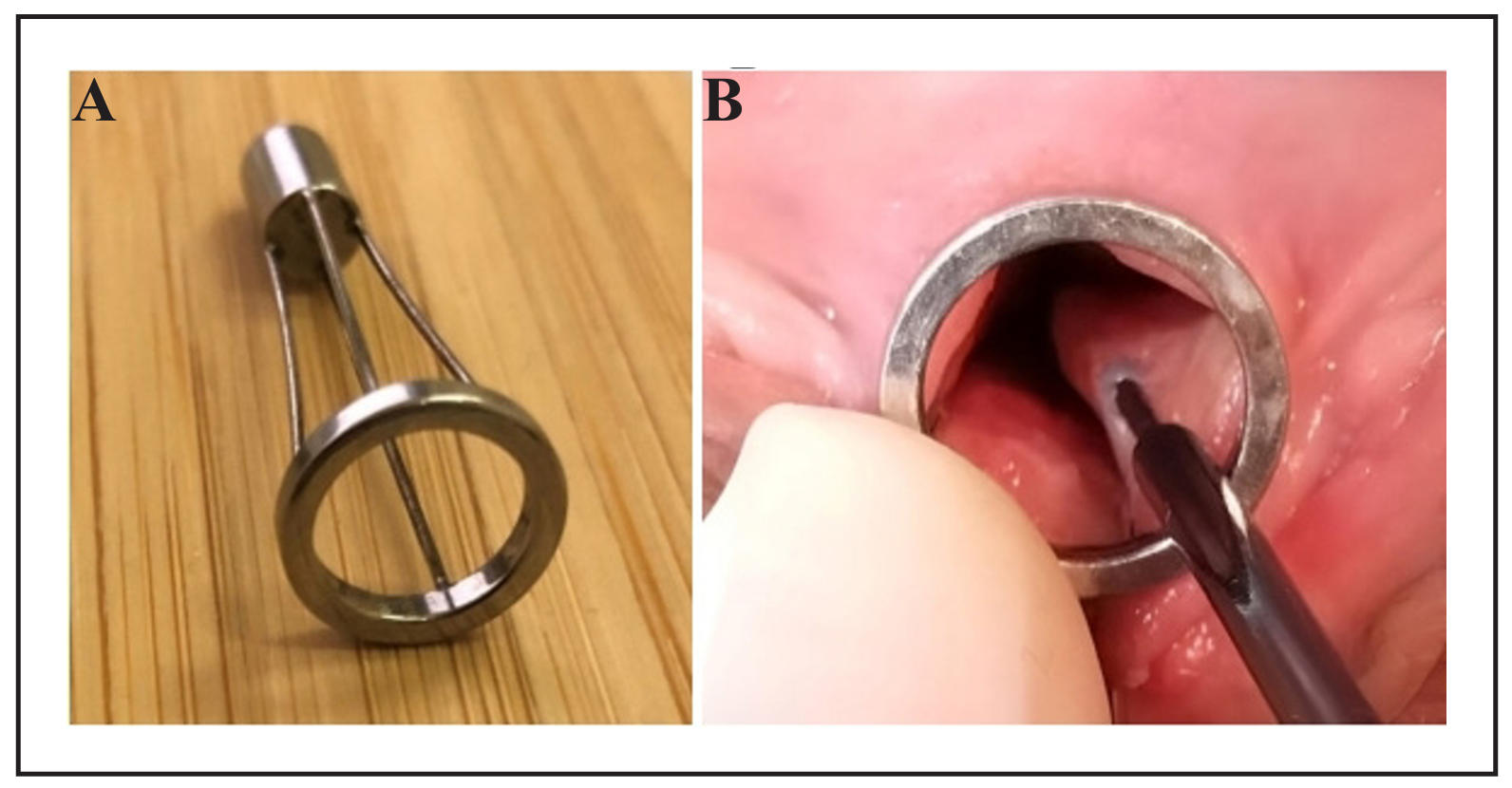
Figure 2. (A) Prototype appearance of the urethral viewing speculum; (B) Examination of the urethra using the original instrument.
The speculum is available in sizes 21, 24, and 27 Ch, allowing selection
of an appropriate size for optimal visualization, accommodating various
anatomical variations.
Using the standard method, the median examination time was 287 seconds
(Q1–Q3: 241-347), with an average of 2 identified SG ducts (Q1–Q3: 2-2).
In contrast, when utilizing the original instrument, these values improved
to a median of 139 seconds (Q1–Q3: 124-157) and 3 identified ducts (Q1–Q3: 3-4),
respectively. Inflammatory changes, such as hyperemia and/or infiltration
of the mucosa, were observed in 14 (25.5%) women with the conventional
method and in 15 (27.2%) cases using the urethral speculum. These parameters
were considered indicators of diagnostic informativeness (Table 1).
Table 1.
Diagnostic informativeness of the examination.
| Indicators | Standard method (n = 55) | Original instrument (n = 55) | P-value |
|---|---|---|---|
| Examination time (seconds), Me (Q1–Q3) | 287 [241-347] | 139 [124-157] | < 0.001 |
| Condition of the urethral mucosa (hyperemia and/or infiltration, pcs, %) | 14 (25.5%) | 15 (27.2%) | 0.318 |
| Number of identified ducts of the SG (pcs), Me (Q1–Q3) | 2 [2-2] | 3 [3-4] | < 0.001 |
Statistical analysis using the Wilcoxon signed-rank test demonstrated
significant differences in the medians of the evaluated parameters
between the two methodologies, with a high effect size (P < 0.001 for each parameter).
The time required for the examination was reduced by 51.6%, while the number of
identified ducts increased by 1.5 times. The incidence of hyperemia and/or infiltration
of the urethral mucosa was similar across both techniques (x2 = 1; P = 0.318).
Consequently, the criteria for diagnostic effectiveness—specifically,
the duration of the physical examination and the number of identified
ducts—were significantly improved with the use of the original instrument.
Safety indicators for the proposed visualization method were also favorable;
the median pain score on the visual analog scale (VAS) during examination
with forceps was 7 (Q1–Q3: 7-8), compared to a median of 3 (Q1–Q3: 3-4)
with the urethral speculum (Figure 3).
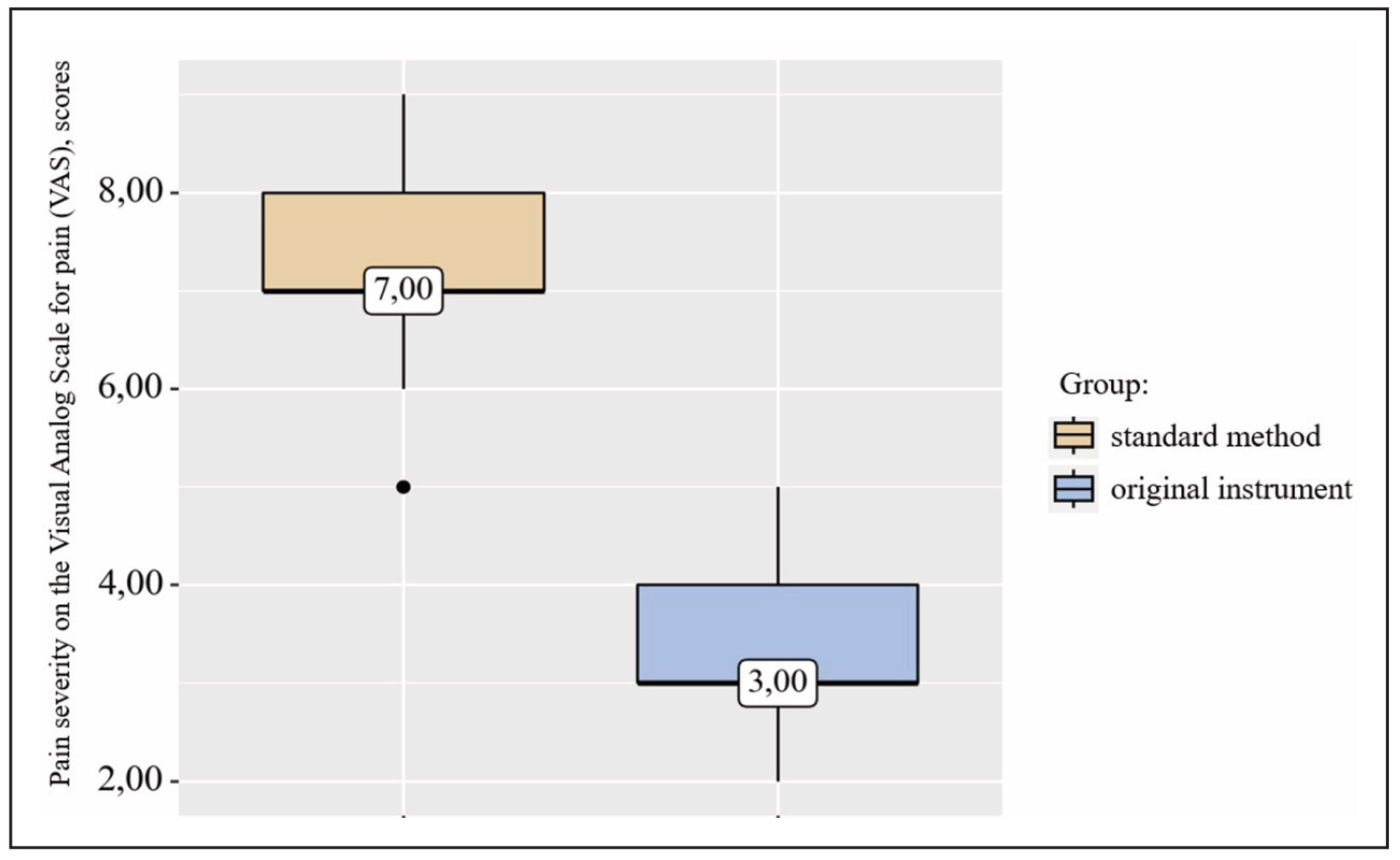
Figure 3. Diagrams illustrating the range of median VAS scores based on the method employed.
Urinalysis results indicated that 45 patients (81.8%) exhibited hematuria following examination with forceps, whereas hematuria was observed in only 11 women (20%) after examination with the original instrument (Figure 4).
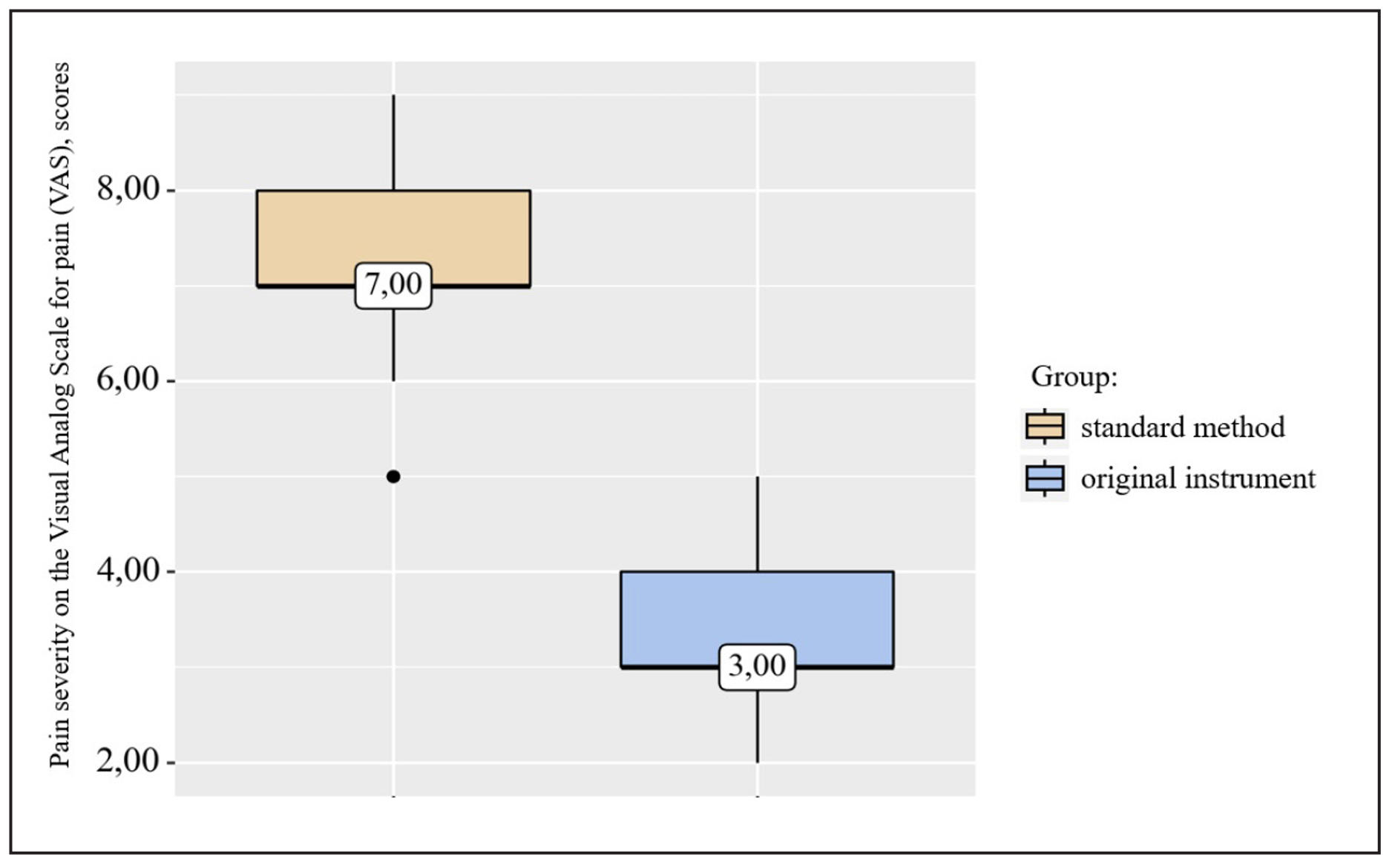
Figure 4. Frequency of hematuria detection based on the method utilized.
Statistical evaluation revealed significant differences in pain scores on the VAS (P < 0.001) and in the prevalence of hematuria at the conclusion of the study (x2 = 32; P < 0.001). The developed instrument proved effective in reducing pain associated with the examination by a factor of 2.3 and in decreasing the occurrence of hematuria post-examination by 52%.
Discussion
Palpation of the anterior vaginal wall in the region of the urethra
has been a standard diagnostic technique for skeneitis since the
early 20th century. This method facilitates the assessment of
tenderness and the exclusion of mucopurulent fluid from the
meatus [3, 4, 8, 9]. Despite its continued use, which can aid in
suspecting the diagnosis during a patient's initial visit [1, 5],
this technique has notable limitations. Primarily, it is subjective
and heavily reliant on the physician's experience. Furthermore,
its effectiveness may be compromised in anxious or emotional patients,
as well as in those with myofascial pain syndrome of the pelvic floor
muscles, where a high likelihood of false-positive results exists.
Subsequent to palpation, a visual examination of the urethra and
skene's glands is warranted. Indicators such as swelling of the paraurethral
gland orifices, hyperemia in the surrounding tissues, and significant tenderness
upon probe insertion can help confirm the suspected diagnosis. However, it is
crucial to recognize that the urethra is not always a distensible structure;
it behaves as a collapsed canal when not in the act of micturition. Thus,
separation of its walls is essential for adequate visualization of skene's
glands. Historically, various instruments have been proposed for this purpose.
For example, the skenescope developed by C. Moore, based on Kelly's endoscope,
and refined by H. Walhter, failed to meet expectations and did not have widespread
adoption [11, 13].
Current endoscopic equipment is primarily designed for the assessment
of the male urethra, resulting in limited visualization of the proximal
female urethra and rendering the distal segment virtually inaccessible.
Due to the short and wide anatomy of the female urethra, irrigating
solutions used to distend the organ often escape during examination.
Consequently, detection of purulent fluid expulsion from the orifices
of the skene's gland ducts is infrequent (Figure 5A).
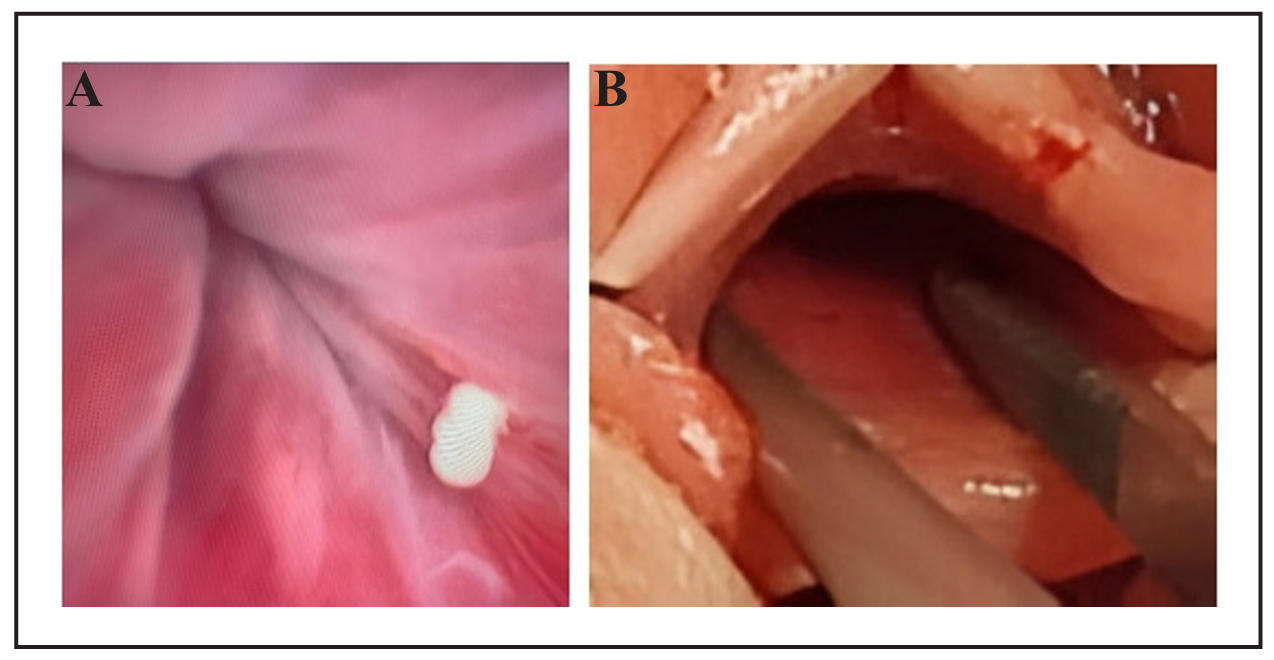
Figure 5. (A) Expulsion of purulent fluid from the orifice of the SG ducts during urethrocystoscopy in a woman with chronic skineitis. (B) Instrumental examination of the urethra using tweezers.
At present, surgical tweezers (Figure 5B) are commonly employed for
instrumental examination. However, utilizing these or similar instruments
as urethral retractors presents several challenges. The primary issue is
inadequate visualization of the urethral walls in a plane perpendicular
to the direction of stretching, which hampers thorough examination of
the distal portion, where the majority of skene's gland orifices are located.
The introduction of a specialized instrument designed specifically
for examining the female urinary tract in patients suspected of skeneitis
could significantly benefit clinicians. In our assessment, a urethral
viewing speculum may serve as a valuable tool in this regard.
Conclusions
Chronic inflammation of the paraurethral glands is a frequently
overlooked etiology of recurrent urinary tract infections. Existing
diagnostic techniques are inadequate in providing sufficient visualization
of the female urinary tract and the orifices of skene's gland ducts.
Furthermore, these methods can be complex to execute and may cause significant
discomfort to patients, complicating the examination process and diminishing
the efficacy of subsequent surgical interventions.
The urethral speculum developed in this study reduces examination time
by 51.6% and increases the identification of ducts by 1.55 times, thereby
demonstrating high diagnostic efficacy. Additionally, the application of
this speculum significantly reduces pain during examination by a factor
of 2.3 and decreases the incidence of post-examination hematuria by 41.8%,
highlighting its improved safety profile.
The introduction of this original instrument offers an innovative,
effective, rapid, and atraumatic method for visualizing the urinary
tract in women suspected of skeneitis.
Declarations
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and informed consent
Not applicable.
Consent for publication
Not applicable.
References
1. Kislitsyn P, Protoshchak V, Kukushkin A, Sinelnikov L, Galyuk D, Babkin P, et al. Inflammation of paraurethral ducts and glands in women: the problem with 350 years history. Experimental and Clinical Urology, 2023, 16(4): 143-155. [Crossref]
2. Heller D. Lesions of skene glands and periurethral region: a review. J Low Genit Tract Dis, 2015, 19(2): 170-174. [Crossref]
3. Mazhbits A. Diseases of the skeletal glands. In obstetric and gynecological urology with atlas. Leningrad, 1936: 116-124.
4. Mazhbits A. Operative urogynecology. Moscow: Medicine, 1964: 416-419.
5. Gluharev A. Inflammation of parauretral glanduli in women-scineitis. Journal of obstetrics and women's diseases, 1999, 48(2): 79-81. [Crossref]
6. Skene A. The anatomy and pathology of two important glands of the female urethra. The American Journal of Obstetrics and Diseases of Women and Children (1869-1919), 1880, 13(2): 265-275.
7. Slesarevskaya M, Ignashov Y, Kuzmin I, & Al-Shukri S. Persistent dysuria in women: etiological diagnostics and treatment. Urology reports (St.-Petersburg), 2021, 11(3): 195-204. [Crossref]
8. Eberhart C. The etiology and treatment of urethritis in female patients. J Urol, 1958, 79(2): 293-299. [Crossref]
9. Eberhart C, & Morgan J. The treatment of urethritis in female patients. II. J Urol, 1959, 81(1): 146-149. [Crossref]
10. Le Fur R. Diathermy in Urology. Bull. med, 1922, (36): 5-9.
11. Walther H. An electric skeneoscope. Journal of the American Medical Association, 1927, 88(1): 27-27. [Crossref]
12. Walther H, & Peacock C. Diathermy in urology: preliminary report. Journal of the American Medical Association, 1924, 83(15): 1142-1147. [Crossref]
13. Rieser C. A new method of treatment of inflammatory lesions of the female urethra. JAMA, 1968, 204(5): 378-384.