Open Access | Review
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Flexible and navigable ureteral access sheath (FANS-UAS): a narrative literature review
Abstract
Since the first description in 1974 of the ureteral access sheaths (UAS), its use during retrograde intrarenal surgery (RIRS) has showed multiple benefits. In addition, due to minimizing intra renal pressure (IRP), it could decrease the incidence of infectious complications after ureteroscopy, that have an overall incidence of 10% after RIRS. Nonetheless, there is still discordant data about the role of UAS in decreasing the risk of UTI and sepsis, and the use of UAS may cause lesions to the ureter by direct trauma during sheath insertion or affecting blood flow during its usage. During the last 10 years, suction access sheaths for mini-PCNL and RIRS have sparked interest among endourologists as they may achieve higher stone-free rates (SFR) and lower complication rates. In this paper, we perform a narrative review, covering the current evidence regarding flexible and navigable ureteral access sheath for RIRS.
Keywords
Ureteroscopy, suction, UAS, RIRS, stone
Introduction
Since the first description in 1974 of the ureteral access sheaths (UAS) [1],
its use during retrograde intrarenal surgery (RIRS) has showed multiple benefits,
such as facilitating multiple entries into the kidney during the procedure and
achieving better vision due to improved irrigation and outflow, washing out
small stone particles created during lithotripsy, a feature that may improve
stone clearance [2]. In addition, due to minimizing intra renal pressure
(IRP), it could decrease the incidence of infectious complications after
ureteroscopy [3]. Urinary tract infections (UTI) and sepsis still represent
a major issue, with an overall incidence of 10% after RIRS [4]. Nonetheless,
there is still discordant data about the role of UAS in decreasing the risk
of UTI and sepsis [5], and the use of UAS may cause lesions to the ureter
by direct trauma during sheath insertion or affecting blood flow during
its usage [6, 7].
The study of IRP has been more frequently debated, since a prolonged
increase in IRP can lead to complications, especially related to pyelorenal
backflow, leading to potential severe complications [8]. During the last 10
years, suction access sheaths for mini-PCNL and RIRS have sparked interest
among endourologists as they may achieve higher stone-free rates (SFR) and
lower complication rates [9-12]. In this paper, we perform a narrative review,
covering the current evidence regarding flexible and navigable ureteral
access sheath for RIRS.
Evidence acquisition
We performed a comprehensive English literature research for
original and review articles through December 2024 and January 2025,
using Pubmed and Embase databases, as well as a comprehensive review
of The American Urological Association (AUA) guidelines and European
Association of Urology (EAU) Guidelines. We searched for the following
terms: "ureteral access sheath", "flexible navigable ureteral access
sheath", "flexible navigable suction ureteral access sheath".
and "(("Ureteral Access Sheath" OR "ureteral access sheath" OR "UAS")
AND ("Aspiration" OR "Suction") AND ("Retrograde Intrarenal Surgery"
OR "RIRS" OR "Flexible Ureteroscopy") AND ("Kidney Calculi"[Mesh]
OR "renal stones" OR "nephrolithiasis" OR "urolithiasis")).
The combination of terms found 794 related articles; articles
that were not in English, case reports, editorials, duplicated
papers and papers without available abstract were not considered
for this review. After the initial screening, 43 full-text studies
were left for evaluating eligibility. Finally, 21 papers were
considered eligible and included in this review (Figure 1).
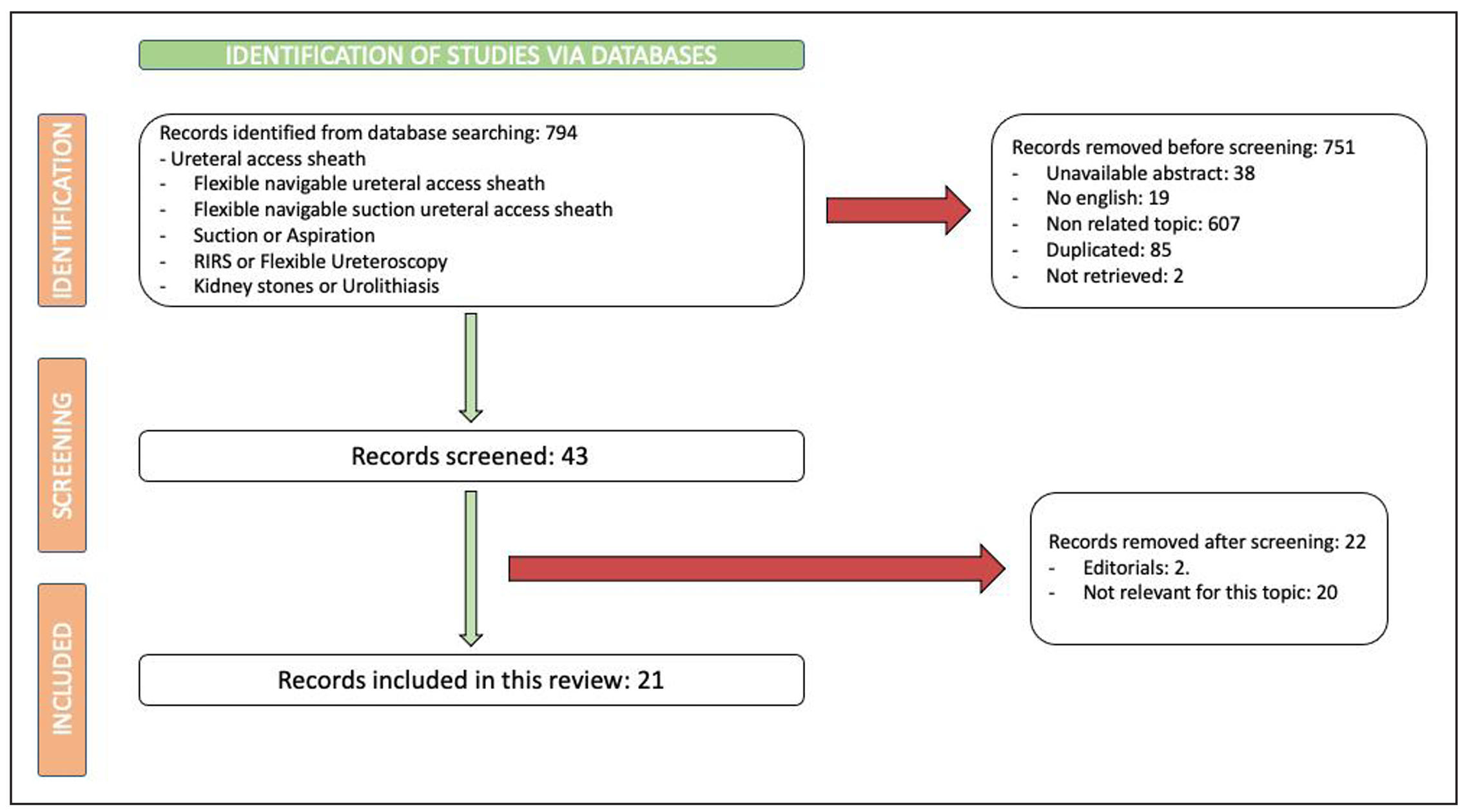
Figure 1. Overview of the study selection process.
Evidence synthesis and discussion
Current guidelines recommendations
The European Association of Urology (EAU) accepts the use of UAS as part of routine practice in RIRS, being safe and useful for large and multiple renal stones, or if a long procedural time is expected [13, 14]. The American Urological Association (AUA) guidelines also discusses their positive role, but there is no specific recommendation for patient selection for UAS selection [14, 15]. Currently, there is insufficient evidence to create consensus on suction access sheaths. The European Association of Urology (EAU) guidelines do not mention ureteral FANS, but they remark that there is some evidence regarding suction access sheaths for mini-PCNL in order to reduce IRP and increase SFR [13, 16]. The American Urological Association (AUA) does not mention any recommendations regarding these devices [15].
FANS-UAS stone-free rate
Of the 21 studies analyzed, 20 reported stone-free rate (SFR) in their results (Table 1), defining it as the sum of SFR-A (no residual fragments) and SFR-B (one residual fragment smaller than 2 mm) within the first 30 days. Additionally, SFR-A is also referred to as the Zero-Fragment Rate (ZFR). Two studies in the pediatric population reported a high SFR with FANS-UAS [17, 18]. Seven studies [17, 19-24] compared the performance of FANS-UAS with conventional UAS (CUAS), finding that the initial and final SFR was statistically higher for FANS-UAS. However, the final SFR showed no statistically significant differences in pediatric population [17]. In the adult population, the overall SFR with FANS-UAS was greater than 90%. Two studies [25, 26] stratified their results based on the caliber of the ureteral access sheath. Kwok et al. [25] reported a significantly higher ZFR in the smaller-diameter group (67.5% vs. 52.9%, P = 0.02), but they were not able to find statistically significant differences between smaller and larger diameters for SFR (SFR smaller group: 95.9%; SFR larger group: 95.3%; P > 0.99). In contrast, Gauhar et al. [26] reported better outcomes with larger sheath diameters (SFR 10 Ch: 68.8%; SFR 12 Ch: 94.7%; P < 0.01). However, although Castellani et al. [27] subdivided their cohort into 2 groups according to the source of energy source used for lithotripsy (Thulium-fiber laser (TFL) and Pulsed-Thulium:YAG Laser), the group with the higher stone-free rate (Pulsed-Thulium:YAG laser) also had a greater proportion of cases treated with smaller caliber sheaths (10-12 Ch) than the other group (TFL 12.5%; Pulsed-Thulium:YAG Laser 98.4%, P < 0.001).
Table 1
Characteristics of the studies describing stone-free rates (SFR) among their results.
| Author | Study design | Population | Number of patients (n) | UAS/FURS size | Basketing only for stone removal | SFR | Reintervention rate / ESWL for residual fragments | Year of publication |
| Turedi et al. [17] | Double-arm, retrospective | Pediatrics | 46 (23 patients/arm) |
CUAS 9,5/11,5 Ch 10/12 Ch 11/13 Ch FANS/UAS 10/12 Ch-26 cm ClearPetra Wellead 7,5 Ch Scope |
CUAS: 73.9% FANS/UAS: 30.4% P = 0.003 |
Initial: CUAS: 65.2% FANS/UAS: 91.3% P = 0.03 Final: CUAS: 87% FANS/UAS: 95.7% P = 0.29 |
CUAS: 26.1% - RIRS 17.4% - miniPCNL 4.35% - ESWL: 4.35% FANS/UAS: 8.7% - RIRS 8.7% P = NR | 2025 |
| Gauhar et al. [18] | Multicentric, prospective | Pediatrics | 50 |
10/12 Ch 11/13 Ch 40-46 cm ClearPetra Wellead |
0% | 100 % | 0% | 2024 |
| Gonçalves et al. [19] | Systematic review and meta-analysis | Adults | 2255 |
T-UAS 12/14 Ch 11/13 Ch S-UAS 10/12 Ch 11/13 Ch 12/14 Ch |
NR |
Day 1 T-UAS: 7.2-75.68% S-UAS: 76.3-88.73% Day 30: T-UAS: 70-93.4% S-UAS: 86.7-95.2% |
NR | 2025 |
| Rico et al. [20] | Double-arm, retrospective | Adults | 96 |
FANS/UAS 10/12 Ch CUAS 10/12 Ch Uscope 7.5 Ch PUSEN |
Only in CUAS, percentage NR |
4th-week CT-scan: FANS/UAS: 93.7% CUAS: 75% P < 0.001 |
NR | 2025 |
| Cacciatore et al. [21] | Randomized Controlled Trial | Adults | 132 |
FANS/UAS 10–12 Ch/46 cm or 10-12Ch/50 cm Clear-Petra® Wellead, or NP-UAS® Innovex CUAS 10/12 Fr Dual Lumen UAS (Rocamed Bi-Flex®) 35-45 cm |
NR |
FANS-UAS: 95% CUAS: 67% P= 0.005 |
FANS-UAS: 5% CUAS: 23% P = 0.02 |
2025 |
| Uslu et al. [22] | Multicentric, prospective | Adults | 88 |
NTBS ClearPetra Wellead Diameter NR SAS 9.5/11.5 Scope NR |
NR |
NTBS: 81.4% SAS: 73.3% P = 0.259 |
NR | 2024 |
| Geavlete et al. [23] | 3 arms, single center, prospective | Adults | 105 |
CUAS 10/12 Ch FANS 10/12 Ch DISS + FANS 10/12 Ch ClearPetra or YigaoMed PUSEN 7.5 Ch |
NR |
CUAS: 17.14% FANS: 11.42% DISS + FANS: 2.85% P = NR |
NR | 2024 |
| Chen et al. [24] | Double-arm, retrospective | Adults | 238 |
TFS-UAS 12-14 Ch 38-45 cm T-UAS 12-14 Ch 38-45 cm |
NR |
Day 1: TFS-UAS: 87.2% T-UAS: 73.45% Day 30: TFS-UAS: 95.2% T-UAS: 85.84% P < 0.05 |
NR | 2024 |
| Giulioni et al. [34] | Systematic review | Adults and exvivo models (porcine) | 2028 |
FANS-UAS Intelligent pressure-control system Negative pressure induced by a ureteral catheter DISS Irrigation and suctioning platform |
NR | 64.3% (At 3-weeks) to 100% (at 1 month) | NR | 2024 |
| Gauhar et al. [35] | Multicentric, prospective | Adults | 394 |
10/12 Ch 11/13 Ch 12/14 Ch ClearPetra Wellead Innovex Elephant Other Scope NR |
NR | 97.2% | RIRS 2.79% | 2024 |
| Gauhar et al. [28] | Multicentric, prospective | Adults | 142 |
ClearPetra Wellead Innovex Elephant ZSR Biomedical Technology < 8 Ch Scope (48.1%) < 8 Ch Scope (51.9%) |
0% | 96.5% | RIRS 2.8% | 2024 |
| Kwok et al. [25] | Multicentric, prospective | Adults | 295 |
ClearPetra Innovex Elephant Seplou Group A: 10/12 Ch Group B: 11/13 or 12/14 Ch Scope 7,5 Ch or > 8 Ch |
Group A: 0% Group B: 0% |
Group A: 95.9% Group B 95.3% P > 0.99 |
Group A: 10.6% Group B 2.3% P = 0.08 ESWL or RIRS not specified |
2024 |
| Gauhar et al. [26] | Multicentric, retrospective | Adults | 31 |
Elephant Group 1: 10 Ch Group 2: 12 Ch Scope NR |
NR |
Group A: 68.8% Group B 94.7% P < 0.01 |
NR | 2023 |
| Shrestha et al. [29] | Multicentric, prospective | Adults | 394 |
ClearPetra Innovex Elephant Others 10/12 Ch 11/13 Ch 12/14 Ch Scope: < 8 Ch or >8 Ch |
Group 1. Non-lower pole: 13.1% Group 2. Lower pole: 13.5% P > 0.99 |
Group 1. Non-lower pole: 96.6% Group 2. Lower pole: 98.4% P = 0.6 |
Group 1. Non-lower pole: 3.36% - RIRS: 3.36% - ESWL: 0% Group 2. Lower pole: 1.59% - RIRS: 1.59 - ESWL: 0% P = NR |
2024 |
| Bai et al. [30] | Multicentric, retrospective | Adults | 231 |
Elephant 12/14 Ch Uscope 9.2 Ch PUSEN |
0% |
Immediate SFR 90.48% Long-term SFR 95.67% |
3.46% RIRS: 3.46% ESWL: 0% |
2024 |
| Geavlete et al. [36] | Review | Adults | NR |
ClearPetra Elephant 10/12 Ch 11/13 Ch 12/14 Ch Scope: Flex-X2 Storz Uscope 9.2 Ch PUSEN Scivita Medical 8.4 Ch. |
NR |
SFR Day-1 Range: 57.1-100% SFR Day-30 Range: 66.7-100% SFR Day-90 Range: 68.8-100% |
NR | 2024 |
| Castellani et al. [27] | Multicentric, prospective | Adults | 179 |
ClearPetra Innovex Elephant 10/12 Ch 11/13 Ch 12/14 Ch Scope NR |
Group 1. Thulium-fiber laser (TFL): 4.7% Group 2. Pulsed-Thulium:YAG Laser: 10.9% P = 0.32 |
Group 1. Thulium-fiber laser (TFL): 93.7% Group 2. Pulsed-Thulium:YAG Laser: 85.9% P = 0.04 |
Group 1. Thulium-fiber laser (TFL): 3.1% RIRS: 3.46% ESWL: 0% Group 2. Pulsed-Thulium:YAG Laser: 17.2% P = 0.02 |
2025 |
| Fong et al. [31] | Multicentric, prospective | Adults | 310 |
ClearPetra Innovex Yigaomed Seplou 10/12 Ch 11/13 Ch 12/14 Ch Scope NR |
4.5% | 95.1% |
4.2% RIRS: 3.88% ESWL: 0.32% |
2025 |
| Gauhar et al. [37] | Multicentric, prospective | Adults | 192 |
ClearPetra Innovex Elephant Seplou 10/12 Ch 11/13 Ch 12/14 Ch Scope NR |
NR |
Group 1. HPHL: 99% Group 2. TFL: 95.9% P > 0.99 |
Group 1. HPHL: 1% Technique NR Group 2. TFL: 1% Technique NR P > 0.99 |
2025 |
| Lim et al. [38] | Multicentric, prospective | Adults | 562 |
10/12 Ch 11/13 Ch 12/14 Ch Scope NR |
NR |
Group 1: 91.3% Group 2: 98.3% P = 0.001 |
Group 1: 6.8% - RIRS: 5.3% - ESWL: 1.5% Group 2: 1.2% - RIRS: 0.8% - ESWL: 0.4% P = 0.003 |
2025 |
Note: UAS: ureteral access sheath. FURS: flexible ureteroscope. SFR: stone-free rate. CUAS: conventional ureteral access sheath. T-UAS: traditional UAS. S-UAS: suction UAS. FANS-UAS: flexible and navigable suction ureteral access sheath. NTBS: nobel tip-bendable suction-assisted ureteral access sheath. SAS: standard ureteral access sheath. DISS: direct in-scope suction. TFS-UAS: tip-flexible suctioning ureteral access sheath. RIRS: retrograde intrarenal surgery. ESWL: extracorporeal shock wave lithotripsy. PCNL: percutaneous nephrolithotomy. NR: not reported. TFL: thulium fiber laser. HPHL: high-power holmium laser. Significant P values are in bold font.
Intraoperative IRP and perioperative complications
There were only two papers that described intraoperative IRP measurements
during surgery among their results. Chen et al. [8] described and stratified
IRP during RIRS with FANS-RIRS according to different variables. IRP was
measured using LithoVue Elite™ ureteroscope (Boston Scientific Corp.,
Marlborough, MA, USA) with pressure sensing capability. The IRP remained below
40 mmHg in 76.2% of the total time in all procedures, but the overall amount
of procedure time spent at pressures between 60-80 mmHg and > 80 mmHg was
3.6% and 1.8% respectively. Median IRP was 29.0 mmHg for the 11/13 Ch diameter
and 14.0 mmHg for the 12/14 Ch diameter (P = 0.008). Pre-stenting also significantly
decreased IRPs (pre-stented 14.5 mmHg; non-prestented patients 29.0 mmHg (P < 0.001)).
Other variables significantly associated with lower IRP were the use of preoperative
alpha-blocker and having a prior endourological intervention (any ipsilateral URS or
ureteral stenting within the last 5 years). Bai et al. [30] measured IRP in 30 patients
with a computed numerical control system based on sheath-side fiber optic pressure
sensor monitoring, where the fiber optic pressure sensor enters the renal pelvis
through a side channel to monitor renal pelvis pressure. During lithotripsy,
pressure variated across calyxes and upper ureter, with statistically significant
differences (Upper calyx 19.82 ± 0.57; Middle calyx 18.07 ± 0.85; Lower
calyx 20.32 ± 0.72; Upper ureter 21.59 ± 1.14; P < 0.001). All values are below
the cut-off value of 35–40 mmHg when the pyelotubular back-flow usually occurs [39-41],
hence increasing the risk of infectious complications and postoperative pain.
All papers describe an overall complication rate lesser than 20% with the use of
FANS (Table 2), including intra and postoperative ones. Most of the complications
are Clavien-Dindo grades 1 or 2. The infectious complication rate was rather low.
Regarding urosepsis, defined as sepsis (life-threatening organ dysfunction caused
by a dysregulated host response to infection) caused by a urogenital tract infection,
has an incidence between 0.1 and 4.3% after ureteroscopy [4]. All but one of the
papers cited in this article had 0% rate of urosepsis. Giulioni et al. [34] analyzed
different suction modalities (via Access Sheath, via Scope and via catheter),
with an overall low complication rate for all of them.
Table 2
Overall complication rates and postoperative pain.
| Author | Clavien-Dindo (C-D) grade complications | Postoperative pain |
| Chen et al. [8] |
Grade 1-2: 0% Grade 3-4: 4% UTI: 4% (all grade 3) |
NR |
| Turedi et al. [17] |
CUAS - Grade 1-2: 17.4% - Grade 3-4: 8.7% - UTI: 8.7% (all grade 2) FANS-UAS - Grade 1-2: 13% - Grade 3-4: 0% - UTI: 4.35% (all grade 2) P = 0.30 |
NR |
| Gauhar et al. [18] |
Grade 1-2: 16% UTI: 8% (all grade 2) |
2.18 [1.34 SD] |
| Gonçalves et al. [19] |
T-UAS - Fever: 5.3-18.92% S-UAS - Fever: 0.8-9.5% |
NR |
| Rico et al. [20] |
FANS-UAS - Grade < 2: 4.2% CUAS - Grade < 2: 6.3% P = 0.64 |
NR |
| Cacciatore et al. [21] |
FANS-UAS: 10% CUAS: 25% P = 0.02 |
FANS-UAS: 16% CUAS: 33% P = 0.02 |
| Uslu et al. [22] |
NTBS: 9.3% SAS: 26.6% P = 0.032 |
NR |
| Geavlete et al. [23] |
CUAS: 14.29% FANS: 14.29% DISS + FANS: 5.71% P = NR |
NR |
| Chen et al. [24] |
TFS-UAS - Grade 1-2: 1.6% T-UAS - Grade 1-2: 14.16% P < 0.001 |
NR |
| Gauhar et al. [35] |
Grade 1-2: 13.8% UTI: 3.3% (all grade 2) |
1 1-2 IR |
| Gauhar et al. [28] |
Grade 1-2: 26.6% UTI: 7% (all grade 1) |
2 1-2 IR |
| Kwok et al. [25] |
Group A - Grade 1-2: 4% - Grade 3-4: 0% - UTI: 0.8% Group B - Grade 1-2: 12.46% - Grade 3-4: 0% - UTI: 4.9% P > 0.05 |
Group A 1 1-2 IR Group B 2 1-2 IR P = 0.58 |
| Gauhar et al. [26] |
Group 1 - Grade 1: 6.3% - UTI: 0% Group 2 - Grade 1: 5.3% - Grade 2: 5.3% - UTI: 0% P > 0.05 |
NR |
| Shrestha et al. [29] |
Group 1 - Grade 1-2: 4.2% - Grade 3-4: 0% - UTI: 2% Group 2 - Grade 1-2: 11.3% - Grade 3-4: 0% - UTI: 5,7% P > 0.1 |
Group 1: 1 1-2 IR Group 2: 2 1-2 IR P = 0.04 |
| Bai et al. [30] |
Grade 1-2: 0.86% Grade 3-4: 0% UTI: 0.86% |
1: 12.99% 2: 37.23% 3: 44.59% 4: 0.43% 5: 4.76% |
| Castellani et al. |
Group 1 - Grade 1-2: 4.7% - Grade 3-4: 0% - UTI: 4.7% (all grade 2). Group 2: 0% P = 0.24 |
Group 1: 1 1-2 IR Group 2: 2 1-1.25 IR P = 0.06 |
| Fong et al. [31] |
Grade 1-2: 6.7% Grade 3-4: 0% |
1 [1-2] |
| Gauhar et al. [37] |
Group 1 - Grade 1-2: 5.4 % - Grade 3-4: 0% - UTI: 3.4% (all grade 1). Group 2: 0% - Grade 1-2: 10% - Grade 3-4: 0% - UTI: 3.8% (all grade 1). P > 0.99 |
Group 1: 2 1-3 IR Group 2: 2 1-2 IR P = 0.61 |
| Lim et al. [38] |
Group 1 - Grade 1-2: 5.9% - Grade 3-4: 0% Group 2 - Grade 1-2: 7.3% - Grade 3-4: 0% P > 0.5 |
Group 1: 1 1-2 IR Group 2: 2 1-2 IR P = 0.06 |
Note: UAS: ureteral access sheath. CUAS: conventional ureteral access sheath. FANS-UAS: flexible and navigable suction ureteral access sheath. T-UAS: traditional UAS. S-UAS: suction UAS. NTBS: nobel tip-bendable suction-assisted ureteral access sheath. SAS: standard ureteral access sheath. DISS: direct in-scope suction. UTI: urinary tract infection. NR: not reported. Significant P values are in bold font.
Postoperative pain was measured at day 1 after surgery using a 10-point visual analogue score (1-4: mild pain; 5-8: moderate pain; 9-10: severe pain). Eleven papers describe postoperative pain [18, 21, 25, 27-31, 35, 37, 38], reporting low rates of discomfort after surgery.
Surgical times (ST)
We only considered for this section those papers that compared ST according to different features, such as UAS diameter, stone location, suction. energy used for lithotripsy and anesthesiology ventilation modality during surgery (Table 3), including thirteen articles. ST were measured in minutes and divided into three categories: Operative time, ureteroscopy time and laser time.
Table 3
Comparative surgical time.
| Author | Comparison | Operative time (minutes) | Ureteroscopy time (minutes) | Laser time (minutes) |
| Turedi et al. [17] | Suction vs. non-suction UAS |
CUAS: 67.9 ± 21.0 FANS-UAS: 50.4 ± 21.1 P < 0.01 |
NR | NR |
| Gonçalves et al. [19] | Suction vs. non-suction UAS |
T-UAS (range): 39.03-101.2 S-UAS: 40.9-80 P = NR |
NR | NR |
| Rico et al. [20] | Suction vs. non-suction UAS |
FANS-UAS: 33.5 26.3-44.5 IR CUAS: 57.5 40-65 IR P < 0.001 |
NR |
FANS-UAS: 17.5 12.5-23 IR CUAS: 21.5 18-24.6 IR P = 0.04 |
| Cacciatore et al. [21] | Suction vs. non-suction UAS |
CUAS: 61.36 46.63-125.35 IR FANS-UAS: 55.25 43.63-118.35 IR P = 0.028 |
NR |
CUAS: 11.96 5.64-23.7 IR FANS-UAS: 11.85 5.14-23.88 IR P = 0.56 |
| Uslu et al. [22] | Suction vs. non-suction UAS |
NTBS: 55 48-65 IR SAS: 62 59-72 IR P = 0.016 |
NR | NR |
| Geavlete et al. [23] | Non-suction vs. suction UAS vs. suction UAS + DISS |
CUAS: 50.28 30-90 IR FANS: 53 35-80 IR DISS + FANS: 52.5 30-75 IR P = NR |
NR | NR |
| Chen et al. [24] | Suction vs. non-suction UAS |
TFS-UAS: 101.17 ± 25.64 T-UAS: 86.23 ± 20.35 P < 0.001 |
NR | NR |
| Kwok et al. [25] |
Sheath diameter A: Smaller Sheath (10/12 Ch) vs. B: Larger Sheath (11/13 or 12/14 Ch) |
Group A: 50 37.5-73.5 IR Group B: 45 32-55 IR P < 0.01 |
Group A: 35 25-58 IR Group B: 31.5 23-41 IR P = 0.02 |
Group A: 17 12-28 IR Group B: 17 11-25 IR P = 0.34 |
| Gauhar et al. [26] |
Sheath diameter Group 1: 10 Ch vs. Group 2: 12 Ch |
Group 1: 63 52-74.5 p25-75 Group 2: 76 63-85.25 p25-75 P = 0.09 |
NR | NR |
| Shrestha et al. [29] |
Stone location Group 1: Non-lower pole Group 2: Lower pole |
Group 1: 49 38-67 IR Group 2: 50 36-71 IR P = 0.8 |
Group 1: 35 26-55 IR Group 2: 35 24-54 IR P = 0.6 |
Group 1: 19 12-28 IR Group 2: 17 11-28 IR P = 0.3 |
| Castellani et al. [27] |
Energy: Group 1. Thulium-fiber laser (TFL) Group 2. Pulsed-Thulium:YAG |
Group 1: 45 29.9-55 IR Group 2: 40 35-45 IR P = 0.09 |
Group 1: 30 22-39 IR Group 2: 28 25-33 IR P = 0.14 |
Group 1: 15.5 10-23 IR Group 2: 13 10-15 IR P = 0.02 |
| Gauhar et al. [37] |
Energy: Group 1. High-Power Holmium Laser (HPHL) Group 2. Thulium-fiber laser (TFL) |
Group 1: 45 38-59 IR Group 2: 47 33-65 IR P = 0.70 |
Group 1: 33 26-40 IR Group 2: 35 23-49 IR P = 0.78 |
Group 1: 18 11-26 IR Group 2: 16 11-24 IR P = 0.96 |
| Lim et al. [38] |
Anesthesiology ventilation modality Mechanical vs. Gated ventilation |
Mechanical: 45 36-60 IR Gated: 49 39-60 IR P = 0.24 |
Mechanical: 31 24-45 IR Gated: 35 25-45 IR P = 0.33 |
Mechanical: 16 11-25 IR Gated: 15 10-22 IR P = 0.02 |
Note: UAS: ureteral access sheath. CUAS: conventional ureteral access sheath. FANS-UAS: flexible and navigable suction ureteral access sheath. T-UAS: traditional UAS. S-UAS: suction UAS. NTBS: nobel tip-bendable suction-assisted ureteral access sheath. SAS: standard ureteral access sheath. DISS: direct in-scope suction. TFL: thulium fiber laser. HPHL: high-power holmium laser. Significant P values are in bold font.
Turedi et al. [17] , Rico et al. [20] and Kwok et al. [25] found a statistically significant difference in operative time (OT) in favor of the suction UAS and the larger UAS. Regarding ureteroscopy time, only Kwok et al. [25] were able to describe a statistically significant difference for larger UAS. Finally, Castellani et al. [27] and Lim et al. [38] described statistically significant shorter laser times for Pulsed Thulium:YAG laser and Gated ventilation. The rest of the papers did not find differences in ST. In addition, Giulioni et al. [34] described shorter operative times in the different analyzed suction modalities.
Intraoperative ergonomy
Nine papers evaluated subjectively different ergonomics [18, 23, 25, 26, 28, 29, 31, 37, 38] (Table 4). Except for Gauhar et al. [22] that did not use a numeric-scale, and Geavlete et al. [23] that used an ascending scale from 0 to 10, from worst to best, the rest of the articles used a Likert-scale between 1 (excellent) and 5 (difficult) to assess either subjective maneuverability, visibility, manipulation of the sheath and ease of suction. Overall results were between excellent or very good in all sections. Kwok et al. [25] found statistically significant differences in visibility and ease of suction depending on the diameter (better visibility with larger sheaths and easier suction with smaller sheaths). In addition, Gauhar et al. [37] described significant differences in visibility and manipulation depending on the source of energy (results were better in the TFL group compared to the HPHL group).
Table 4.
Subjective data regarding ergonomics.
| Author | Subjective maneuverability | Visibility | Manipulation | Ease of suction |
|---|---|---|---|---|
| Gauhar et al. [18] | NR |
Likert-scale 1.02 0.32 SD |
Likert-scale 1.24 0.52 SD |
Likert-scale 1.16 0.47 SD |
| Geavlete et al. [23] | NR |
CUAS: 6/10 FANS: 8/10 FANS + DISS: 9/10 |
NR | NR |
| Gauhar et al. [28] | NR |
Likert-scale 2 1-3 IR |
Likert-scale 2 2-3 IR |
Likert-scale 2 1-3 IR |
| Kwok et al. [25] | NR |
Likert-scale Group A 1.41 0.76 IR Group B 2.68 1.53 IR P < 0.01 |
Likert-scale Group A 1.99 0.75 IR Group B 2.15 0.82 IR P = 0.09 |
Likert-scale Group A 1.64 0.82 IR Group B 1.85 0.71 IR P = 0.02 |
| Gauhar et al. [26] |
Group A Excellent 37.5% Very good 56.3% Good 6.3% Group B Excellent 52.6% Very good 36.8% Good 10.6% P = 0.57 |
Group A Excellent 68.8% Very good 31.3% Group B Excellent 84.2% Very good 15.8% P = 0.15 |
Group A Excellent 31.3% Very good 56.3% Good 12.5% Group B Excellent 44.4% Very good 44.4% Good 11.2% P = 0.73 |
NR |
| Shrestha et al. [29] | NR |
Likert-scale Group 1: 1 1-3 IR Group 2: 1 1-3 IR P = 0.7 |
Likert-scale Group 1: 2 2-2 IR Group 2: 2 1-3 IR P = 0.2 |
Likert-scale Group 1: 2 1-2 IR Group 2: 2 1-2 IR P = 0.3 |
| Fong et al. [31] | NR |
Likert-scale 1 1-1 IR |
Likert-scale 2 2-2 IR |
Likert-scale 2 1-2 IR |
| Gauhar et al. [37] | NR |
Likert-scale Group 1: 3 1-4 IR Group 2: 1 1-2 IR P < 0.01 |
Likert-scale Group 1: 2 2-3 IR Group 2: 1 1-2 IR P < 0.01 |
Likert-scale Group 1: 2 1-2 IR Group 2: 2 1-2 IR P = 0.11 |
| Lim et al. [38] |
Likert-scale Group 1: 2 1-2 IR Group 2: 2 2 IR P = 0.24 |
Likert-scale Group 1: 1 1-3 IR Group 2: 1 1-2 IR P < 0.01 |
NR |
Likert-scale Group 1: 2 1-2 IR Group 2: 2 1-2 IR P = 0.48 |
Note: NR: not reported. SD: standard deviation. IR: interquartile range. FANS-UAS: flexible and navigable suction ureteral access sheath. DISS: direct in-scope suction. Significant P values are in bold font.
Study limitations
Our study has some limitations. The nature of its design (narrative review) is not exempt from bias. The included stud¬ies differ significantly in terms of study design and methodologies, patient demo¬graphics, and outcome measures. For instance, many of the studies did not compare FANS-UAS against CUAS. Many of these studies were performed by high-volume experienced centers/surgeons, being difficult to extrapolate these results to less experienced centers.
Conclusions
Current evidence on the safety profile and stone-free rates (SFR) of suction ureteral access sheaths (UAS) demonstrates superior outcomes compared to standard UAS, supporting their recommendation and adoption in routine clinical practice.
Declarations
Authors contributions
“Conceptualization”, L.E.O.P.; methodology, L.E.O.P.; J.G.R.; validation, L.E.O.P.; J.G.R.; formal analysis, L.E.O.P., E.J.G.R.; investigation, L.E.O.P., E.J.G.R., A.S.P., G.F.J.B.H.; data curation, L.E.O.P.,; writing—original draft preparation, L.E.O.P., E.J.G.R., A.S.P., G.F.J.B.H.; writing—review and editing, L.E.O.P., E.J.G.R., A.S.P., G.F.J.B.H.; supervision, L.E.O.P., A.S.P., E.J.G.R., M.A.R.L., A.S.P., G.F.J.B.H., A.S.B., L.I.V., P.M.D., I.G.R., J.G.R., S.A.G., J.M.S.; All authors have read and agreed to the published version of the manuscript.
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and informed consent
Not applicable.
Consent for publication
Not applicable.
References
1. Takayasu H, & Aso Y. Recent development for pyeloureteroscopy: guide tube method for its introduction into the ureter. J Urol, 1974, 112(2): 176-178. [Crossref]
2. Santa Cruz J, Danilovic A, Vicentini F, Brito A, Batagello C, Marchini G, et al. Ureteral access sheath. Does it improve the results of flexible ureteroscopy? A narrative review. Int Braz J Urol, 2024, 50(3): 346-358. [Crossref]
3. Yuen S, Zhong W, Chan Y, Castellani D, Bhojani N, Agarwal M, et al. Current utility, instruments, and future directions for intra-renal pressure management during ureteroscopy: scoping review by global research in intra-renal pressure collaborative group initiative. Ther Adv Urol, 2025, 17: 17562872251314809. [Crossref]
4. De Coninck V, Keller E, Somani B, Giusti G, Proietti S, Rodriguez-Socarras M, et al. Complications of ureteroscopy: a complete overview. World J Urol, 2020, 38(9): 2147-2166. [Crossref]
5. Villa L, Dioni P, Candela L, Ventimiglia E, De Angelis M, Corsini C, et al. Understanding the role of ureteral access sheath in preventing post-operative infectious complications in stone patients treated with ureteroscopy and Ho:Yag laser lithotripsy: results from a tertiary care referral center. J Clin Med, 2023, 12(4): 1457-1467. [Crossref]
6. Wright A, Williams K, Somani B, & Rukin N. Intrarenal pressure and irrigation flow with commonly used ureteric access sheaths and instruments. Cent European J Urol, 2015, 68(4): 434-438. [Crossref]
7. Alhefnawy M, Abdelrahman M, Abo-Elnasr H, & Eldib H. Ureteral access sheath or percutaneous nephrostomy during flexible ureteroscopy: which is better? Urolithiasis, 2025, 53(1): 18-28. [Crossref]
8. Chen K, Koo K, Zhong T, Ren R, Wong V, Almousa S, et al. Real time monitoring of intrarenal pressures while using the flexible and navigable suction ureteral access sheath. World J Urol, 2025, 43(1): 76-86. [Crossref]
9. Zeng G, Wan S, Zhao Z, Zhu J, Tuerxun A, Song C, et al. Super-mini percutaneous nephrolithotomy (SMP): a new concept in technique and instrumentation. BJU Int, 2016, 117(4): 655-661. [Crossref]
10. Kankaria S, Gali K, Chawla A, Bhaskara S, Hegde P, Somani B, et al. Super-mini PCNL (SMP) with suction versus standard PCNL for the management of renal calculi of 1.5 cm-3 cm: a randomized controlled study from a university teaching hospital. World J Urol, 2024, 42(1): 257-267. [Crossref]
11. Quhal F, Zeng G, & Seitz C. Current evidence for suction in endourological procedures: comprehensive review of literature. Curr Opin Urol, 2023, 33(2): 77-83. [Crossref]
12. Liang H, Liang L, Lin Y, Yu Y, Xu X, Liang Z, et al. Application of tip-bendable ureteral access sheath in flexible ureteroscopic lithotripsy: an initial experience of 224 cases. BMC Urol, 2023, 23(1): 175-185. [Crossref]
13. EAU Guidelines. Edn. presented at the EAU Annual Congress Paris 2024. ISBN 978-94-92671-23-3.
14. Yuen S, Traxer O, Wroclawski M, Gadzhiev N, Chai C, Lim E, et al. Scoping review of experimental and clinical evidence and its influence on development of the suction ureteral access sheath. Diagnostics, 2024, 14(10): 1034-1044. [Crossref]
15. Assimos D, Krambeck A, Miller N, Monga M, Murad M, Nelson C, et al. Surgical management of stones: American urological association/endourological society guideline, part I. J Urol, 2016, 196(4): 1153-1160. [Crossref]
16. Tzelves L, & Skolarikos A. Suction use during endourological procedures. Curr Urol Rep, 2020, 21(11): 46-56. [Crossref]
17. Turedi B, & Sezer A. Comparison of flexible and navigable suction ureteral access sheath with conventional ureteral access sheath for pediatric retrograde intrarenal surgery: a single-center propensity-matched analysis. Urolithiasis, 2024, 53(1): 17-27. [Crossref]
18. Gauhar V, Madarriaga Y, Somani B, Joshi R, Tanidir Y, Castellani D, et al. Is flexible and navigable suction ureteral access sheath (FANS-UAS) the next best development for retrograde intrarenal surgery in children? Results of a prospective multicentre study. World J Urol, 2024, 42(1): 627-637. [Crossref]
19. Gonçalves F, Porto B, Terada B, Spilborghs J, Passerotti C, Sardenberg R, et al. Enhanced stone-free rates with suctioning ureteral access sheath vs. traditional sheath in retrograde intrarenal surgery: a systematic review and meta-analysis. BMC Urol, 2025, 25(1): 86-99. [Crossref]
20. Rico L, Diaz-Zorita V, Blas L, Ramos L, Sabeh P, & Contreras P. Is the ablation stone efficacy and efficiency better with a flexible and navigable suction ureteric access sheath? World J Urol, 2025, 43(1): 219-225. [Crossref]
21. Cacciatore L, Minore A, Bonanno L, Contessa P, Esperto F, Iannello A, et al. Is flexible navigable suction ureteral access sheath (FANS) safer and more efficient than conventional sheaths? Italian multicentric experience. World J Urol, 2025, 43(1): 153-163. [Crossref]
22. Uslu M, Yildirim Ü, Ezer M, Arslan Ö, Yaşar H, & Sarica K. Comparison of tip-bendable aspiration-assisted and standard access sheaths in the treatment of lower calyceal stones. Rev Assoc Med Bras (1992), 2024, 70(12): e20241033. [Crossref]
23. Geavlete P, Mareș C, Mulțescu R, Georgescu D, Ene C, Iordache V, et al. Small diameter (7.5 Fr) single-use flexible ureteroscopy with direct in-scope suction (DISSTM) in conjunction with aspiration-assisted flexible access sheath: a new hype for real stone-free? J Clin Med, 2024, 13(23): 7191-7204. [Crossref]
24. Chen H, Xiao J, Ge J, & Liu T. Clinical efficacy analysis of tip‑flexible suctioning ureteral access sheath combined with disposable flexible ureteroscope to treat 2-4 cm renal stones. Int Urol Nephrol, 2024, 56(10): 3193-3199. [Crossref]
25. Kwok J, Somani B, Sarica K, Yuen S, Zawadzki M, Castellani D, et al. Multicenter outcome analysis of different sheath sizes for flexible and navigable suction ureteral access sheath (FANS) ureteroscopy: an EAU endourology collaboration with the global FANS study group. Urolithiasis, 2024, 52(1): 162-172. [Crossref]
26. Gauhar V, Traxer O, Castellani D, Ragoori D, Heng C, Chew B, et al. A feasibility study on clinical utility, efficacy and limitations of 2 types of flexible and navigable suction ureteral access sheaths in retrograde intrarenal surgery for renal stones. Urology, 2023, 178: 173-179. [Crossref]
27. Castellani D, Fong K, Traxer O, Malkhasyan V, Gadzhiev N, Ragoori D, et al. Propensity score matched analysis of thulium fiber vs. pulsed Thulium:Yttrium aluminum garnet laser lithotripsy in flexible ureteroscopy for kidney stone disease using a flexible and navigable suction ureteral access sheath: results from a prospective, multicenter study of the eau section of endourology. Urology, 2025, 199: 47-53. [Crossref]
28. Gauhar V, Traxer O, Castellani D, Fong K, Bin Hamri S, Gökce M, et al. Operative outcomes 24 hours after retrograde intrarenal surgery for solitary renal calculi using a flexible and navigable suction ureteral access sheath. A prospective global multicenter study by the European Association of Urology Section on Urolithiasis. Minerva urology and nephrology, 2024, 76(5): 625-634. [Crossref]
29. Shrestha A, Traxer O, Seitz C, Corrales M, Castellani D, Chew B, et al. Assessing flexible ureteroscopy outcomes for lower Pole versus non lower pole stones using the flexible and navigable suction ureteric access sheath: a prospective multicenter study by EAU Endourology and PEARLS group. World J Urol, 2024, 43(1): 41-51. [Crossref]
30. Bai J, Shangguan T, Zou G, Liu L, Xue X, Lin J, et al. Efficacy and intrarenal pressure analysis of flexible and navigable suction ureteral access sheaths with flexible ureteroscopy in modified surgical positions for 2-6 cm upper urinary tract stones: a multicenter retrospective study. Front Med, 2024, 11: 1501464. [Crossref]
31. Fong K, Yuen S, Somani B, Malkhasyan V, Tanidir Y, Persaud S, et al. Assessment of outcomes and anatomical changes in the upper urinary tract following flexible ureteroscopy with a flexible and navigable suction ureteral access sheath: 3-month results from a multicenter study. Urology, 2025, 199: 35-41. [Crossref]
32. Aboumarzouk O, Monga M, Kata S, Traxer O, & Somani B. Flexible ureteroscopy and laser lithotripsy for stones > 2 cm: a systematic review and meta-analysis. J Endourol, 2012, 26(10): 1257-1263. [Crossref]
33. Geraghty R, Abourmarzouk O, Rai B, Biyani C, Rukin N, & Somani B. Evidence for ureterorenoscopy and laser fragmentation (URSL) for large renal stones in the modern era. Curr Urol Rep, 2015, 16(8): 54-64. [Crossref]
34. Giulioni C, Castellani D, Traxer O, Gadzhiev N, Pirola G, Tanidir Y, et al. Experimental and clinical applications and outcomes of using different forms of suction in retrograde intrarenal surgery. Results from a systematic review. Actas Urol Esp (Engl Ed), 2024, 48(1): 57-70. [Crossref]
35. Gauhar V, Traxer O, Castellani D, Sietz C, Chew B, Fong K, et al. Could use of a flexible and navigable suction ureteral access sheath be a potential game-changer in retrograde intrarenal surgery? Outcomes at 30 days from a large, prospective, multicenter, real-world study by the european association of urology urolithiasis section. Eur Urol Focus, 2024, 10(6): 975-982. [Crossref]
36. Geavlete P, Multescu R, Mares C, Buzescu B, Iordache V, & Geavlete B. Retrograde intrarenal surgery for lithiasis using suctioning devices: a shift in paradigm? J Clin Med, 2024, 13(9): 2493-2506. [Crossref]
37. Gauhar V, Traxer O, Fong K, Sietz C, Chew B, Bin Hamri S, et al. Comparing thulium fiber versus high-power holmium laser lithotripsy combined with the flexible and navigable suction access sheath in flexible ureteroscopy for kidney stone disease: a propensity score matched analysis by the global FANS collaborative group. J Endourol, 2025, 39(1): 42-49. [Crossref]
38. Lim E, Somani B, Gokce M, Heng C, Satapathy A, Robles J, et al. General anaesthesia with gated or controlled mechanical ventilation and its influence on peri and post operative outcomes of retrograde intra renal surgery when using flexible and navigable suction access sheath, an EAU-endourology and global FANS collaborative study group: a prospective study. World J Urol, 2025, 43(1): 110-120. [Crossref]
39. Tokas T, Herrmann T, Skolarikos A, & Nagele U. Pressure matters: intrarenal pressures during normal and pathological conditions, and impact of increased values to renal physiology. World J Urol, 2019, 37(1): 125-131. [Crossref]
40. Han Z, Wang B, Liu X, Jing T, Yue W, Wang Y, et al. Intrarenal pressure study using 7.5 French flexible ureteroscope with or without ureteral access sheath in an ex-vivo porcine kidney model. World J Urol, 2023, 41(11): 3129-3134. [Crossref]
41. Tang Q, Liang P, Ding Y, Zhou X, & Tao R. Comparative efficacy between retrograde intrarenal surgery with vacuum-assisted ureteral access sheath and minimally invasive percutaneous nephrolithotomy for 1-2 cm infectious upper ureteral stones: a prospective, randomized controlled study. Front Surg, 2023, 10: 1200717. [Crossref]