Open Access | Case Report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Retrograde intra renal surgery (RIRS): the most minimally invasive stone surgery, its safety and efficacy in patient with sickle cell anemia. A case report and review of literature for the optimal peri-operative management in sickle cell patients
* Corresponding author: Ravi Jineshkumar Jain
Mailing address: Department of Urology and Renal Transplantation, GCS Medical College and Research Centre, Asarwa, Ahmedabad, India.
Email: imshahiduro@gmail.com
This article belongs to the Special Issue: Nightmare and complex cases in Urology
Received: 14 March 2024 / Revised: 07 April 2024 / Accepted: 16 April 2024 / Published: 27 June 2024
DOI: 10.31491/UTJ.2024.06.021
Abstract
Sickle cell anemia (SCA) is a genetic hematologic disorder characterized by repeated hemolytic and vasoocclusive episodes. Surgical procedures in such patients carry the risk of bleeding and coagulation problems. Kidney stone is a common health problem in India. Optimal management depends on various stone-related factors (stone burden, location, hardness, degree of hydronephrosis) and patient-related factors. Kidney stone surgery in patients with bleeding disorders can be challenging. Extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy are minimally invasive procedures. However, they carry a risk of bleeding and are relatively contraindicated in patients with bleeding disorders. Retrograde intra renal surgery (RIRS) is the most minimally invasive modality for upper tract calculi due to the lowest risk of bleeding. Since there is no puncture of the kidney, it is relatively safe in patients with bleeding disorders, cardiac patients on antiplatelet therapy, recurrent stone formers, solitary kidneys, and stones in anatomically abnormal kidneys. Our patient presented with a 13 × 12 mm upper ureteral calculus with hydronephrosis. He was diagnosed with SCA during pre-operative work up. We achieved complete stone clearance with RIRS. No postoperative complications such as bleeding, urosepsis, sickling crisis, renal infarction, etc. were observed. The patient was discharged within 48 hours and is doing well. To date, there is no reported case of RIRS for renal stone management in patients with SCA. We aim to report this case and review the literature for the ideal perioperative management of SCA patients.
Keywords
Sickle cell disease, sickle cell anemia, retrograde intra renal surgery, kidney stone, percutaneous lithotomy, extra corporeal shock wave lithotripsy
Introduction
Sickle cell disease (SCD) is the most common genetically inherited hematologic disorder. Sickle cell anemia (SCA) represents
the most severe form of SCD due to its renal manifestations. It is characterized by the mutant sickle β-globin resulting from the
replacement of valine for glutamic acid at the sixth amino acid position. Sickle cell hemoglobin (HbS) polymerizes when the
concentration of its deoxygenated form (deoxyHbS) is exceeded, leading to vaso-occlusive crisis and repeated hemolytic episodes
[1]. Sickling of red blood cells (RBCs) can lead to clumping and early destruction of RBCs.
Sickle cell nephropathy can cause myriad of complications such as hematuria, proteinuria, renal papillary necrosis, renal tubular
disorder, acute and chronic renal injury, sickle cell glomerulopathy, renal medullary carcinoma, etc.
[2, 3].
Kidney stones are a common urological problem worldwide, especially in India. Various modalities are available for optimal management
of upper tract calculi such as extra corporeal shock wave lithotripsy (ESWL), percutaneous nephrolithotomy (PCNL), mini PCNL
(MPCNL) and retrograde intra renal surgery (RIRS). The kidneys receive almost 25% of cardiac output (1.1 L/min). Therefore, any
puncture of the kidney may carry the risk of bleeding requiring major blood transfusion (0-20%, mean 7%)
[4]. Unlike PCNL and ESWL, RIRS is a completely endoscopic procedure that does not require
an incision in the body or a puncture of the kidney. During the procedure, a flexible ureteroscope is passed directly from the
urethra to the pelvicalyceal system (PCS) in the kidney. Following this, the stone in the kidney is fragmented or dusted with the
help of laser. A double J stent (DJ stent) is deployed at the end of procedure which is removed after 2-4 weeks. The available
literature shows that RIRS has the lowest risk of bleeding compared to MPCNL
[5-8]. Bleeding, dehydration, hypoxia,
etc. can trigger sickling crisis and must be avoided in SCA patients
[9-11]. RIRS is considered the safest modality
for patients with bleeding disorders, patients on antiplatelet therapy, solitary kidney, anatomically abnormal kidney, and recurrent
stone formers [5-7]. Most complications of RIRS
are of lower Clavien grade and major complications are rare [12]. To date, RIRS for stone
management in SCA patients has not been reported in the literature.
Case report
A 45-year-old man presented with 2 months of right flank pain, hematuria, and dysuria. On examination, he was found to have a 15 × 13 mm impacted hard upper ureteral stone (Hounsfield value 1400 HU) just distal to the pelviureteric junction (PUJ). His blood investigations revealed anemia with a hemoglobin (Hb) of 7 g/dL. Rest investigations were normal. Urine culture was sterile. A hematologist's opinion was obtained and he was diagnosed with SCA based on hemoglobin electrophoresis (Figure 1). Under the expert guidance of the hematologist, the patient was transfused with 1 unit of packed cell volume (PCV) and the patient was pre-stented. Two weeks later, his preoperative Hb was 9 g/dL and he was scheduled for RIRS. During RIRS, it was extremely difficult to reach the upper ureteral stone despite pre-stenting. A semi-rigid ureteroscope (6.5/8 Fr) followed by a disposable digital ureteroscope (7.5 Fr) was passed to the level of the upper ureteral stone using two gliding wires (Figure 2A). A thulium fiber laser (IPGTM 35 watt) was used. The upper ureteral stone was first fragmented using laser settings of 0.8-1.0 joules and a frequency of 10-15 hertz. The stone was fragmented from the center to the periphery, safeguarding the ureteral mucosa. Gentle hand-held irrigation with a 100 cm extension tube was used. Once the stone was dis-impacted, it was pushed into the PCS. The ureteral access sheath (10/12 Fr, 35 cm) was then deployed to the upper ureter. A limited-use digital disposable ureteroscope (SeeshenTM) was used for RIRS. The stone was completely dusted into fine golden dust (Figure 2B). Intra renal laser settings were 1.0-1.2 joules and 30-35 hertz for dusting. Finally, popcorn settings of 0.05-0.1 joules and 200 hertz were used. Complete on-table stone clearance was observed. Post-procedure contrast study in the form of retrograde pyelography was normal. A DJ stent (5 Fr/26 cm) was routinely placed. Total ureteroscopy time was 40 minutes. No complications in the form of sepsis or bleeding were noted. The stent was removed after 2 weeks.
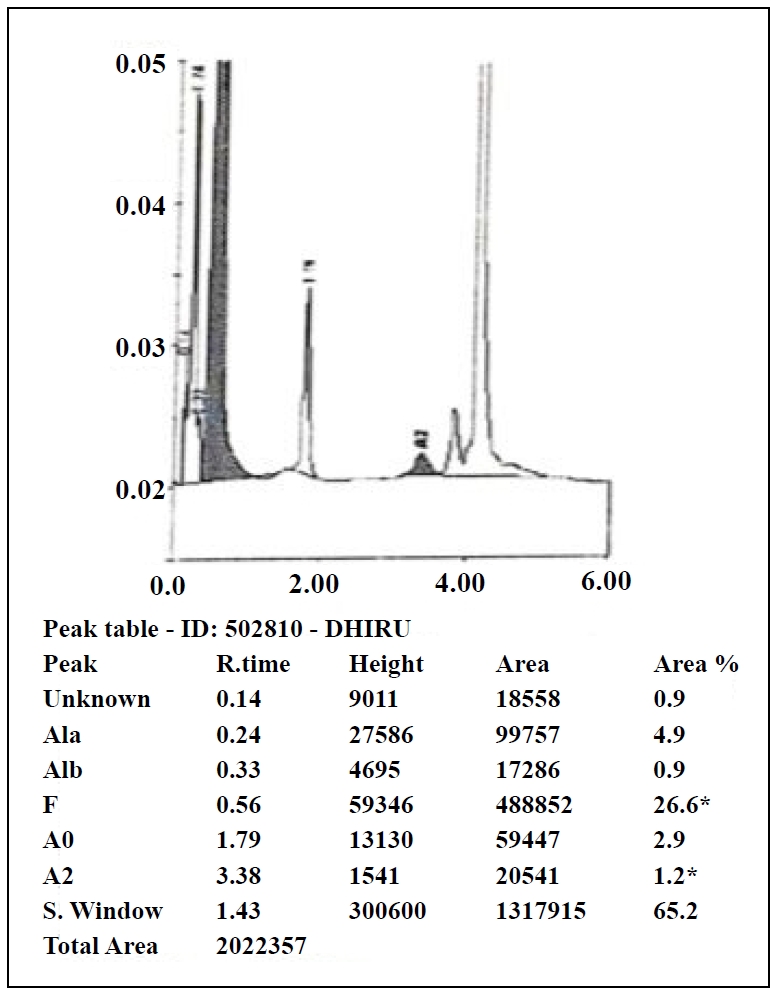
Figure 1. Hemoglobin Electrophoresis showing positive sickling test.
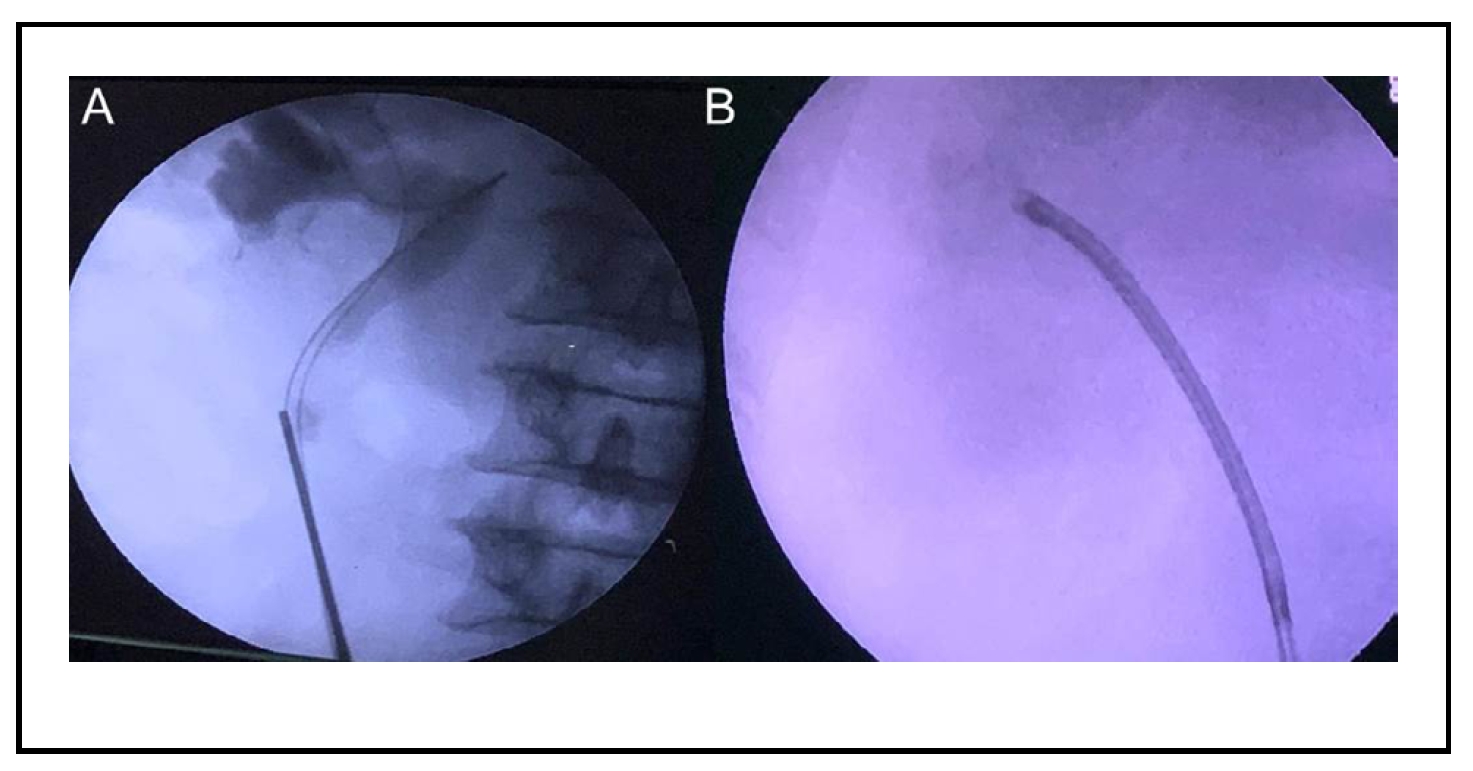
Figure 2. (A) Semi-rigid ureteroscope negotiated up to the level of the upper ureteral stone with difficulty with double gliding wire. (B) Complete stone clearance with RIRS.
Discussion
Normal adult Hb, hemoglobin A (HbA), is composed of two α and two β globin chains (αβ) located on chromosomes 16 and 11. HbS
results from the substitution of valine for glutamic acid at position 6 of the β globin chain
[1]. The resulting HbS polymerizes in response to stress, dehydration, hypothermia,
hypovolemia, acidosis, etc. and causes sickling of RBC and early destruction. SCD is characterized by recurrent
vaso-occlusion [2, 13].
Surgery in SCA patients can be challenging due to the high risk of complications. SCA patients are at high risk for perioperative
mortality, acute chest syndrome, congestive heart failure, sepsis, etc. [9].
Surgical management of SCA patients requires multidisciplinary team management involving urologist, hematologist, pathologist and
nursing staff. Preoperative anemia is crucial for any surgery. There are various schools of thought regarding preoperative blood
transfusion in SCA patients undergoing surgery. The Cooperative Study of SCD conducted the largest cohort study of surgery in SCD
patients. They concluded a beneficial effect of preoperative transfusion in Hb SC patients for all surgical procedures
[9, 10]. However, few studies refute the role of
preoperative transfusion. It is important to avoid the triggering factors of sickle cell crisis such as dehydration, hypoxia,
hypovolemia, hypothermia, stress, infection, vascular stasis and increased blood viscosity
[9-11].
Renal stone disease is a common urological problem worldwide. Mini PCNL and RIRS are currently the mainstay of management of upper
tract calculi. According to the European Association of Urology (EAU) guidelines, RIRS is the first-line modality for non-lower
pole renal stones up to 20 mm [12]. RIRS scores over MPCNL in terms of safety due to a
lower risk of bleeding, pain and hospital stay. The risk of bleeding requiring blood transfusion after PCNL can be up to 20%
(mean 7%), while it is negligible with RIRS [4-8,
14]. RIRS is equally effective for stone clearance of 1.5-2 cm upper tract calculi. Newer
lasers such as the thulium fiber laser (TFL) are proving to be a game changer for RIRS. With the TFL laser, there has been a
significant improvement in stone clearance, decreased operative time, and larger stone loads can be successfully treated with
RIRS [15]. Therefore, RIRS is the modality of choice in high-risk patients, such as
those with bleeding disorders, with excellent outcomes and minimal morbidity.
Conclusions
RIRS is a safe, effective, and minimally invasive modality for upper tract calculi management. It is the procedure of choice in patients with hematological disorders such as SCA. Appropriate perioperative management of these patients is required to prevent major complications.
Declarations
Financial support and sponsorship
None.
Conflict of interest statement
No conflict of interest.
Ethical approval and informed consent
The patient has provided an informed consent for publication of images and information in this study.
References
1. Hebbel RP. Beyond hemoglobin polymerization: the red blood cell membrane and sickle disease pathophysiology. Blood, 1991, 77(2): 214-237.
2. Kassim AA, & DeBaun MR. Sickle cell disease, vasculopathy, and therapeutics. Annu Rev Med, 2013, 64: 451-466. [Crossref]
3. Aeddula NR, Bardhan M, & Baradhi KM: Sickle Cell Nephropathy. In: StatPearls. 2024, edn. StatPearls Publishing.
4. Zumrutbas AE, Toktas C, Baser A, & Tuncay OL. Percutaneous nephrolithotomy in rare bleeding disorders: a case report and review of the literature. J Endourol Case Rep, 2016, 2(1): 198-203. [Crossref]
5. Akgül M, Cakir H, Çinar Ö, Özman O, Başataç C, SIDDIKOĞLU D, et al. The efficacy and safety of retrograde intrarenal surgery: a multi-center experience of the RIRSearch group study. J Urol Sur, 2023, 10(2): 119- 128. [Crossref]
6. Jiao B, Luo Z, Xu X, Zhang M, & Zhang G. Minimally invasive percutaneous nephrolithotomy versus retrograde intrarenal surgery in surgical management of upper urinary stones - a systematic review with meta-analysis. Int J Surg, 2019, 71: 1-11. [Crossref]
7. Lai D, Chen M, He Y, Li X, & Wan S. Safety and efficacy of retrograde intrarenal surgery for the treatment of renal stone in solitary kidney patients. Ren Fail, 2018, 40(1): 390-394. [Crossref]
8. Kallidonis P, Panagopoulos V, Kyriazis I, & Liatsikos E. Complications of percutaneous nephrolithotomy: classification, management, and prevention. Curr Opin Urol, 2016, 26(1): 88-94. [Crossref]
9. Vichinsky EP, Neumayr LD, Haberkern C, Earles AN, Eckman J, Koshy M, et al. The perioperative complication rate of orthopedic surgery in sickle cell disease: report of the national sickle cell surgery study group. Am J Hematol, 1999, 62(3): 129-138. [Crossref]
10. Koshy M, Weiner SJ, Miller ST, Sleeper LA, Vichinsky E, Brown AK, et al. Surgery and anesthesia in sickle cell disease. Cooperative Study of Sickle Cell Diseases. Blood, 1995, 86(10): 3676-3684.
11. Adjepong KO, Otegbeye F, & Adjepong YA. Perioperative management of sickle cell disease. Mediterr J hematol I, 2018, 10(1): e2018032. [Crossref]
12. Bladder MI, & Challacombe B. The 38 th Annual EAU Congress. 2023.
13. Aeddula NR, Bardhan M, & Baradhi KM. Sickle cell nephropathy. 2018.
14. Parikh KP, Jain RJ, & Kandarp AP. Is retrograde intrarenal surgery the game changer in the management of upper tract calculi? A single-center single-surgeon experience of 131 cases. Urol Ann, 2018, 10(1): 29-34. [Crossref]
15. Traxer O, & Corrales M. Managing urolithiasis with thulium fiber laser: updated real-life results-a systematic review. J Clin Med, 2021, 10(15): 3390. [Crossref]