Open Access | Research
This work is licensed under a Creative
Commons Attribution-ShareAlike 4.0 International License.
Evaluation of sexual function and urinary continence after bilateral intrafascial nerve-sparing laparoscopic radical prostatectomy after prostate resection for incidental prostate cancer
* Corresponding author: Francesco Greco
Mailing address: Urology Unit, Centro Salute Uomo, Bergamo, Italy.
Email: francesco_greco@ymail.com
Received: 04 March 2024 / Revised: 08 March 2024 / Accepted: 11 March 2024 / Published: 27 March 2024
DOI: 10.31491/UTJ.2024.03.016
Abstract
Objective: To evaluate the impact of nerve-sparing laparoscopic radical prostatectomy after TUR-P (nsLRPT) on surgical and functional outcomes using a validated questionnaire in patients with incidental prostate cancer.
Materials and methods: Retrospective single surgeon study including 125 consecutive patients who underwent nsLRPT for incidentally diagnosed prostate cancer. The primary outcome parameters were defined as any change in sexual function as measured by the IIEF-5 at 12 months postoperatively compared to baseline as well as changes in IIEF-5 domains and total score over time. Urinary continence and erectile function at follow-up were evaluated using the International Prostate Symptom Score (IPSS), the International Consultation of Incontinence Questionnaire-Urinary Incontinence (ICIQ-UI) short-form instrument. All patients reporting no need for pads were defined as continent. All patients with an IIEF-5 > 17 were defined as potent.
Results: The mean operative time was 153.1 ± 35.4 min with a mean intraoperative blood loss of 350.3 ± 150.4 mL and a transfusion rate of 1.6%. The mean catheterization time was 5 ± 1 days and the mean length of hospitalization was shorter after nsLRPT (6.2 ± 2.1 days). There were no major complications in either group. Positive margins were detected in only 1 patient (1.8%) with pT2c tumor. Nevertheless, all patients were alive with no evidence of tumor recurrence at a median follow-up of 48 months. At 12 months, complete continence was reported in 98.4% of patients who underwent surgery. Regarding sexual potency, 52% and 78.4% of all patients reported the ability to engage in sexual intercourse at 6 and 12 months after surgery, respectively.
Conclusion: sLRP after TUR-P performed by experienced surgeons is a safe procedure with excellent functional outcomes regarding urinary continence and sexual potency.
Keywords
Bilateral intrafascial nerve-sparing radical prostatectomy, incidental prostate cancer, laparoscopy, transurethral prostate resection, sexual function, outcomes
Introduction
The goal of radical prostatectomy (RP) by any approach is the eradication of cancer while, whenever possible, preserving pelvic organ function [1]. Actually, both laparoscopic (LRP) and robot-assisted radical prostatectomy (RARP) represents well-established alternatives to open surgery as they can reduce hospital stay and blood loss [2, 3]. Incidental prostate cancer is found in 3%-16% of transurethral resection of the prostate (TUR-P) specimens [4]. It has been reported that nerve-sparing radical prostatectomy (nsRP) after previous prostate surgery can be challenging [4-8]. A recent meta-analysis suggested that RARP is feasible but challenging after TUR-P and it significantly increases the difficulty of operation and compromises surgical, functional, and oncological outcomes [6]. Many studies on erectile dysfunction (ED) following nerve-sparing RRP have been published, revealing widely disparate potency rates (30-86%) among various groups in different studies [9]. This variation in potency rates may be due to patient selection, surgeon and hospital volume, and the proportion of nerve-sparing procedures. The aim of our study was to investigate the effect of laparoscopic bilateral nerve-sparing radical prostatectomy after TUR-P (nsLRPT) on surgical and functional outcomes in patients previously diagnosed with incidental prostate cancer.
Materials and methods
Study design
This was a retrospective, single-surgeon study of 125 consecutive patients who underwent extraperitoneal laparoscopic bilateral nerve-sparing radical prostatectomies (nsLRPT) for incidental prostate cancer diagnosed after TUR-P. All patients were informed of the procedures and provided written informed consent. Our surgical technique has been described previously [2]. Briefly, after dissection of the bladder neck (Figure 1), the periprostatic fascia including the neurovascular bundles is mobilized and dissection is performed posteriorly behind the bladder neck, and the seminal vesicles and the ductus deferens are identified and dissected. The Denonvilliers' fascia was stripped from the prostatic capsule, and the prostatic pedicles were clipped and dissected (Figure 2A & B). No coagulation or ultrasonic dissector was used during this step. Inclusion criteria were as follows: PSA < 10, Gleason ≤ 7, and only two positive cores from a minimum of 12 biopsies. Surgical and functional outcomes were compared. Postoperatively, all patients were treated with tadalafil 20 mg (on demand) and a vacuum constriction device for a consecutive period of 12 months. No patient underwent nerve-sparing LRP within the first 4 months after TUR-P to reduce periprostatic inflammation due to the first intervention. All surgical procedures were performed by one surgeon (F.G.) who had completed at least 70 nsLRPTs and at least 500 laparoscopic radical prostatectomies before the beginning of the study, thus reducing the learning curve effect. Data are expressed as mean ± standard deviation (SD), and statistical significance was accepted at P < 0.05. Statistical analysis was performed using SigmaPlot® software version 13.0 (SPSS Inc., Chicago, IL, USA) and Graphpad Prism 5 (Graphpad Software, CA, USA). Fisher's exact test was applied to evaluate statistical differences between groups in pathological stages. Changes in sexual function scores over time were analyzed by repeated measures two-way analysis of variance.

Figure 1. Dissection of the bladder neck after TUR-P.
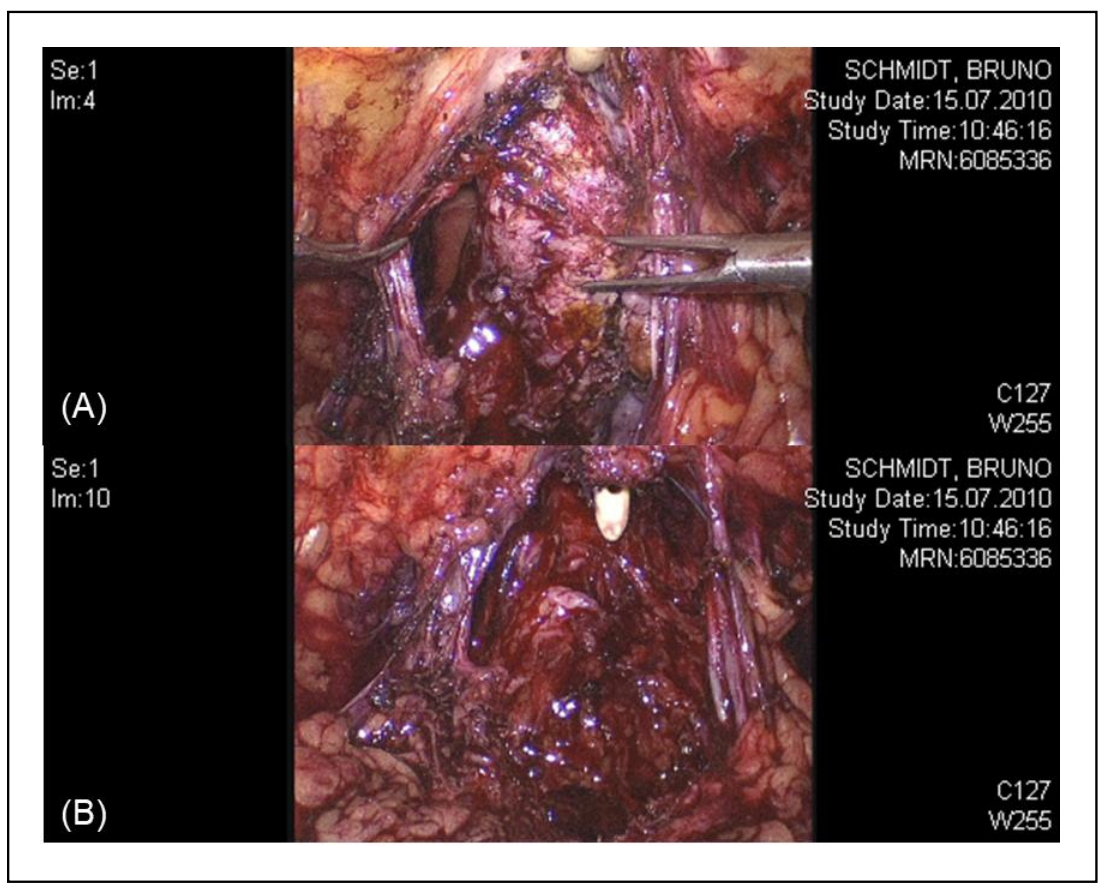
Figure 2. Dissection of the prostatic pedicles.
Main outcome measures
The primary outcome parameters were defined as any change in sexual function as measured by the IIEF-5 at 12 months
postoperatively compared to baseline, as well as changes in IIEF-5 domain and total scores over time. The IIEF-5 questionnaire has
been given to patients preoperatively and at each follow-up visit (3 months, 6 months, 1 year). All questionnaires were completed
independently. The secondary outcome measure of the study was to evaluate the efficacy and clinical performance of nsLRPT in
patients with incidental prostate cancer.
Preoperatively, all patients were evaluated with a general medical history, sexual history, physical examination, 24-hour pad
count (number of sanitary pads used in 24 hours), video urodynamics, and cystoscopy. Urinary continence and erectile function at
follow-up were evaluated using the International Prostate Symptom Score (IPSS), the International Consultation of Incontinence
Questionnaire-Urinary Incontinence (ICIQ-UI) short-form instrument. All patients reporting no need for pads were defined as
continent. All patients with an IIEF-5 > 17 were defined as potent.
Results
Preoperative demographic data are shown in Table 1. Patients were generally young (56.8 ± 6.7 years) with a mean preoperative prostate specific antigen of 3.2 ± 1.4 ng/mL. The mean preoperative IIEF-5 was 22.5 ± 2.3 and the mean preoperative IPSS was 10.6 ± 4.2.
Table 1
Preoperative data.
| Items | nsLRPT (n = 125) |
|---|---|
| Mean age (years) | 56.8 ± 6.7 (48–73) |
| Body mass Index (kg/m2) | 27.7 ± 3.8 (24.2–30.4) |
| PSA level before TUR-P (ng/mL) | 3.2 ± 1.4 (2.1–5.3) |
| Clinical stage: patients (%) | |
| T1a | 51 (40.8%) |
| T1b | 74 (59.2%) |
| Preoperative Gleason score: patients (%) | |
| 5-6 | 92 (73.6%) |
| 7 | 33 (26.4%) |
| 8-10 | 0 |
| mean IIEF-5 | 22.5 ± 2.3 (18–25) |
| mean IPSS | 10.6 ± 4.2 (3–16) |
| mean ICIQ-SF | 0.2 ± 0.4 |
Perioperative data are summarized in Table 2. The mean operative time was 153.1 ± 35.4 min with a mean intraoperative blood loss of 350.3 ± 150.4 mL and a transfusion rate of 1.6%. The mean catheterization time was 5 ± 1 days and the mean hospital stay was shorter after nsLRPT (6.2 ± 2.1 days).
Table 2
Intra and postoperative data.
| Items | nsLRPT (n = 125) |
|---|---|
| Mean operation time (min) | 153.1 ± 35.4 (120–190) |
| Mean estimated blood loss (mL) | 350.3 ± 150.4 |
| Blood transfusion (%) | 1.6 |
| Mean catheterization time (day) | 5 ± 1 (4–6) |
| Mean hospital stays (day) | 6.2 ± 2.1 (3–8) |
| Mean prostate weight (g) | 21.1 ± 4.3 (14–26) |
| Mean Gleason score | 6.35 ± 0.63 |
| Tumor stage (patients) | |
| T0 | 0 |
| T2a | 43 |
| T2b | 28 |
| T2c | 54 |
| T3a/b | 0 |
| Positive surgical margins (pT2c, %) | 1.8 |
| Tumor recurrence at 4 years (patients) | 0 |
Each patient underwent cystography on postoperative day 4 to evaluate the urethral anastomosis for leakage. There were no major complications in either group. Only in one patient who had previously undergone extraperitoneal laparoscopic hernia repair with mesh placement, a lesion of the bladder occurred during developing the preperitoneal space by the balloon. Nevertheless, the bladder was repaired laparoscopically with a two-layer suture line (Figure 3A & B).
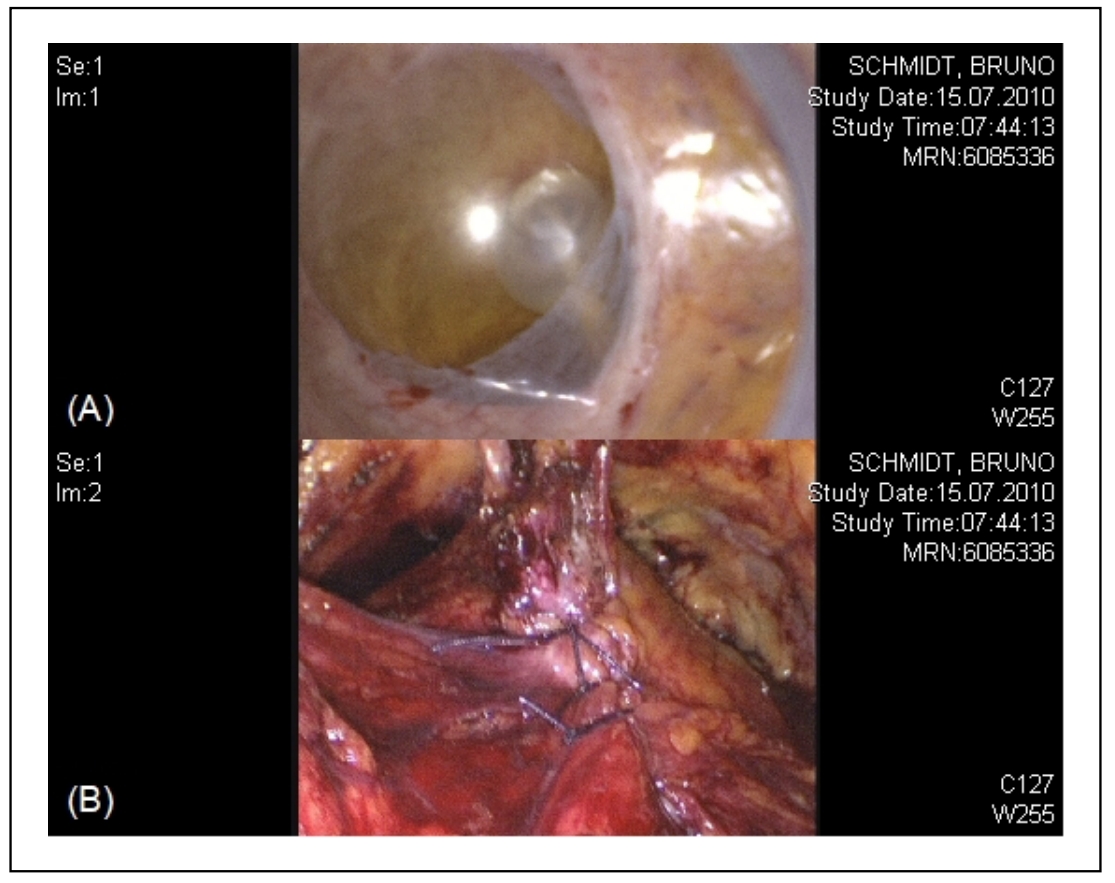
Figure 3. Lesion of the bladder and its repair with a two-layer suture line.
Moreover, two patients (1.6%) required postoperative blood transfusions (Clavien grade 2). The mean Gleason score was 6.35 ±
0.63, and no patient showed absence of prostate cancer at definitive pathologic examination (pT0). Positive margins were detected
in only 1 patient (1.8%) with pT2c tumor. Nevertheless, all patients were alive with no evidence of tumor recurrence at a median
followup of 48 months.
The early return to continence at 4 weeks after the operation was achieved by only 54 (43.2%) patients with the nsLRPT
(Table 3). At 6 months postoperatively, 110 patients (88%) were continent, 13 (10.4%)
experienced a minimal stress incontinence (1-2 pads per day), and 2 (1.6%) experienced a moderate stress incontinence (2-4 pads
per day). At 12 months, complete continence was reported in 98.4% of patients who underwent surgery. Regarding sexual potency,
52.0% and 78.4% of all patients reported the ability to engage in sexual intercourse at 6 and 12 months after surgery,
respectively. The use of phosphodiesterase type 5 (PED5) inhibitors must be considered when interpreting potency results
(on demand tadalafil 20 mg).
Table 3
Postoperative functional outcomes.
| Items | nsLRPT (n = 125) |
|---|---|
| Complete urinary continence: % (patients) | |
| 4 weeks after surgery | 43.2 (54) |
| 6 months after surgery | 88 (110) |
| 12 months after surgery | 98.4 (123) |
| Potency at 6 months after surgery: % (patients) | 52 (65) |
| Potency at 12 months after surgery: % (patients) | 78.4 (98) |
Discussion
In recent years, mini-invasive RP has been suggested as a safe and effective treatment for prostate cancer in specialized
centers [10-16]. Nevertheless, a Cochrane
review comparing either RARP or LRP vs. open RP, which included two RCTs, found no significant differences between the
comparisons for oncological, urinary, and sexual function outcomes, although RARP and LRP both resulted in statistically
significant improvements in duration of hospital stay and blood transfusion rates compared with open RP
[17]. Therefore, one surgical approach cannot be recommended over the other and is mostly
based on surgeon preference and experience.
Performed by any of the surgical approaches, previous TUR-P may impose technical difficulties for the surgical teams, especially
during dissection of the bladder neck. Moreover, previous infections of the prostate and seminal vesicles and perforation of the
prostate capsule during TUR-P with extravasation of irrigation fluid might result in peri-prostatic fibrosis and distortion of the
surgical plains, making dissection difficult. With better visualization of the anatomy and a relatively bloodless field, LRPT has
the potential to provide good functional outcomes with equal oncologic effectiveness [18].
Although Jaffe et al. [19] reported that patients with a history of
transurethral prostate resection who undergo laparoscopic radical prostatectomy have worse outcomes with respect to operative time,
length of stay, positive margin rate and overall complication rate, other reports indicated that radical prostatectomy may be
performed safely with an acceptable morbidity rate following TUR-P, although postoperative urinary incontinence and erectile
dysfunction are more frequent as compared to primary cases [20-23].
Colombo et al. [7] reported on 109 patients who underwent RRP for prostate
cancer, after surgical intervention for BPH. In 88 of these 109 patients the previous intervention was TUR-P. Patients were matched
in pairs according to PSA level, age, and clinical stage. The peri- and post-operative morbidity was moderately increased in
comparing with naïve patients, but functional results were assessed in only 48.8% of patients. In that study, complete urinary
control was achieved in 86%, and adequate erectile function in 12% at 1 year follow-up after RRP.
Performing nerve-sparing radical prostatectomy in patients who previously had surgery for urinary obstruction can present some
unexpected difficulties, requiring better surgical skills [6,
8]. In 2008, Suardi et al. [8] reported
their experience with 15 consecutive patients who underwent nsRRPT after holmium laser enucleation of the prostate (HoLEP) and
after TUR-P, with encouraging results. All operations were successfully performed without major complications. It has been
postulated that nsLRPT resulted in a higher rate of positive margins. For an objective evaluation of the positive margin rate,
three aspects have to be considered. The first is the technique of histopathologic examination, because pathologic evaluation of
the prostate can influence the detection of positive margins. The second aspect is the stratification of positive margin rates
according to pathologic stage. The third aspect is case selection (with or without adjuvant therapy)
[15]. In many reports in the literature [7,
8, 20-23],
there was no significant difference in the rate of positive margins associated with open or laparoscopic RP after TUR-P, as also
found in our study (2.7% and 5.2% in the laparoscopic and open groups, respectively).
The quality of life is strongly affected by urinary incontinence. It has been shown that the incidence of postoperative
incontinence depends on the experience of the urologist, patient age (increased frequency after 70 years), and the operative
technique (i.e., nerve-sparing or not) [24,
25]. Laparoscopic surgery may offer an improved identification of anatomic landmarks
such as striated muscles and neurovascular bundles, resulting in less damage to the striated sphincter. Moreover Stolzenburg
et al. [14] proved better results on early continence by preserving the
puboprostatic ligament during nsLRP. The main question associated with a RP after TUR-P is represented by its safety concerning the
postoperative continence and potency rates. Again, the study group of the University Vita-Salute San Raffaele, Milan
[8] reported an interesting continence rate in all patients who underwent nsRRPT after
HoLEP and TUR-P. At 6 months after the procedure, 93.3% of all patients were continent and 53.3% of patients after HoLEP and 40% of
patients after TUR-P reported satisfactory sexual intercourse with the use of PED5 inhibitors.
In our study, all procedures were performed without major complications. An earlier return to continence was observed in 43.8% of
patients. Nevertheless, complete continence was reported at 12 months in 98.4% of patients who underwent surgery. Regarding sexual
potency, the outcomes resulted to be promising, with 52% and 78.4% of all patients reporting the ability to engage in sexual
intercourse at 6 and 12 months after surgery, respectively. However, these results should be evaluated considering the use of PED5
inhibitors and vacuum constriction device for a consecutive period of 12 months. Although our results can be interpreted as
promising, nsLRPT remains a challenging procedure that requires extensive surgical experience and should be performed in
high-volume centers. Future prospective studies comparing mini-invasive RP after TUR-P with alternative therapies including HIFU
or radiotherapy are needed to identify the best treatment for incidental prostate cancer after TUR-P.
Conclusions
nsLRPT represents a feasible mini-invasive approach to the treatment of prostate cancer also for patients with prior prostate resection. Given the technical difficulties associated with this procedure, LRPT should be performed by experienced surgeons in high-volume centers, in order to improve postoperative oncologic and functional outcomes with regard to urinary continence and sexual potency.
Declarations
Financial support and sponsorship
None.
Conflicts of interest
Francesco Greco is a member of the editorial board of Uro-Technology. The authors declare that they have no conflicts and were not involved in the journal's review or decision regarding this manuscript.
Ethical statement
This study was approved by the Institute Research Medical Ethics Committee of Centro Salute Uomo. All patients were informed of the procedures and provided written informed consent.
References
1. Adolfsson J. Watchful waiting and active surveillance: the current position. BJU Int, 2008, 102(1): 10-14. [Crossref]
2. Greco F, Wagner S, Hoda MR, Kawan F, Inferrera A, Lupo A, et al. Laparoscopic vs open retropubic intrafascial nerve-sparing radical prostatectomy: surgical and functional outcomes in 300 patients. BJU Int, 2010, 106(4): 543-547. [Crossref]
3. Yaxley JW, Coughlin GD, Chambers SK, Occhipinti S, Samaratunga H, Zajdlewicz L, et al. Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study. Lancet, 2016, 388(10049): 1057- 1066. [Crossref]
4. Rassweiler J, Teber D, Kuntz R, & Hofmann R. Complications of transurethral resection of the prostate (TURP)--incidence, management, and prevention. Eur Urol, 2006, 50(5): 969-980. [Crossref]
5. Rossignol G, Leandri P, Ramon J, & Gautier JR. Radical prostatectomy in the management of stage A carcinoma of the prostate. Eur Urol, 1992, 21(4): 269-273. [Crossref]
6. Gu L, Li Y, Li X, & Liu W. Does previous transurethral resection of the prostate negatively influence subsequent robotic-assisted radical prostatectomy in men diagnosed with prostate cancer? A systematic review and metaanalysis. J Robot Surg, 2023, 17(4): 1299-1307. [Crossref]
7. Colombo R, Naspro R, Salonia A, Montorsi F, Raber M, Suardi N, et al. Radical prostatectomy after previous prostate surgery: clinical and functional outcomes. J Urol, 2006, 176(6 Pt 1): 2459-2463. [Crossref]
8. Suardi N, Scattoni V, Briganti A, Salonia A, Naspro R, Gallina A, et al. Nerve-sparing radical retropubic prostatectomy in patients previously submitted to holmium laser enucleation of the prostate for bladder outlet obstruction due to benign prostatic enlargement. Eur Urol, 2008, 53(6): 1180-1185. [Crossref]
9. Albersen M, Joniau S, & Poppel HV. The use of IIEF-5 for reporting erectile dysfunction following nerve-sparing radical retropubic prostatectomy. The Open Prostate Cancer Journal, 2009, 2(1): 1-9. [Crossref]
10. Artibani W, Grosso G, Novara G, Pecoraro G, Sidoti O, Sarti A, et al. Is laparoscopic radical prostatectomy better than traditional retropubic radical prostatectomy? An analysis of peri-operative morbidity in two contemporary series in Italy. Eur Urol, 2003, 44(4): 401-406. [Crossref]
11. Guazzoni G, Cestari A, Naspro R, Riva M, Centemero A, Zanoni M, et al. Intra- and peri-operative outcomes comparing radical retropubic and laparoscopic radical prostatectomy: results from a prospective, randomised, single-surgeon study. Eur Urol, 2006, 50(1): 98-104. [Crossref]
12. Jurczok A, Zacharias M, Wagner S, Hamza A, & Fornara P. Prospective non-randomized evaluation of four mediators of the systemic response after extraperitoneal laparoscopic and open retropubic radical prostatectomy. BJU Int, 2007, 99(6): 1461-1466. [Crossref]
13. Rassweiler J, Stolzenburg J, Sulser T, Deger S, Zumbé J, Hofmockel G, et al. Laparoscopic radical prostatectomy- -the experience of the German laparoscopic working group. Eur Urol, 2006, 49(1): 113-119. [Crossref]
14. Stolzenburg JU, Liatsikos EN, Rabenalt R, Do M, Sakelaropoulos G, Horn LC, et al. Nerve sparing endoscopic extraperitoneal radical prostatectomy--effect of puboprostatic ligament preservation on early continence and positive margins. Eur Urol, 2006, 49(1): 103-112. [Crossref]
15. Lein M, Stibane I, Mansour R, Hege C, Roigas J, Wille A, et al. Complications, urinary continence, and oncologic outcome of 1000 laparoscopic transperitoneal radical prostatectomies-experience at the Charité Hospital Berlin, Campus Mitte. Eur Urol, 2006, 50(6): 1278-1283. [Crossref]
16. Galli S, Simonato A, Bozzola A, Gregori A, Lissiani A, Scaburri A, et al. Oncologic outcome and continence recovery after laparoscopic radical prostatectomy: 3 years' follow-up in a “second generation center”. Eur Urol, 2006, 49(5): 859-865. [Crossref]
17. Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, & Frydenberg M. Laparoscopic and robotic-assisted versus open radical prostatectomy for the treatment of localised prostate cancer. Cochrane Database Syst Rev, 2017, 9(9): Cd009625. [Crossref]
18. Katz R, Borkowski T, Hoznek A, Salomon L, Gettman MT, & Abbou CC. Laparoscopic radical prostatectomy in patients following transurethral resection of the prostate. Urol Int, 2006, 77(3): 216-221. [Crossref]
19. Jaffe J, Stakhovsky O, Cathelineau X, Barret E, Vallancien G, & Rozet F. Surgical outcomes for men undergoing laparoscopic radical prostatectomy after transurethral resection of the prostate. J Urol, 2007, 178(2): 483-487. [Crossref]
20. Yazici S, Inci K, Yuksel S, Bilen CY, & Ozen H. Radical prostatectomy after previous prostate surgery: effects on surgical difficulty and pathologic outcomes. Urology, 2009, 73(4): 856-859. [Crossref]
21. Teber D, Cresswell J, Ates M, Erdogru T, Hruza M, Gözen AS, et al. Laparoscopic radical prostatectomy in clinical T1a and T1b prostate cancer: oncologic and functional outcomes--a matched-pair analysis. Urology, 2009, 73(3): 577-581. [Crossref]
22. Menard J, de la Taille A, Hoznek A, Allory Y, Vordos D, Yiou R, et al. Laparoscopic radical prostatectomy after transurethral resection of the prostate: surgical and functional outcomes. Urology, 2008, 72(3): 593-597. [Crossref]
23. Palisaar JR, Wenske S, Sommerer F, Hinkel A, & Noldus J. Open radical retropubic prostatectomy gives favourable surgical and functional outcomes after transurethral resection of the prostate. BJU Int, 2009, 104(5): 611-615. [Crossref]
24. Salomon L, Sèbe P, De la Taille A, Vordos D, Hoznek A, Yiou R, et al. Open versus laparoscopic radical prostatectomy: part I. BJU Int, 2004, 94(2): 238-243. [Crossref]
25. Salomon L, Sèbe P, De La Taille A, Vordos D, Hoznek A, Yiou R, et al. Open versus laparoscopic radical prostatectomy: Part II. BJU Int, 2004, 94(2): 244-250. [Crossref]