Open Access | Case Report
This work is licensed under a Creative
Commons Attribution-ShareAlike 4.0 International License.
Spontaneous renal pelvic rupture: a case report
* Corresponding author: Javier Pizzarello
Mailing address: Department of Urology, Hospital Aleman, Buenos Aires, Argentina.
Email: javierpizzarello@gmail.com
Received: 13 October 2023 / Revised: 01 November 2023 / Accepted: 21 November 2023 / Published: 25 December 2023
DOI: 10.31491/UTJ.2023.12.015
Abstract
Spontaneous renal pelvic rupture (SRPR) is a rare entity. Diagnosis is made by contrast-enhanced computed tomography or retrograde pyelography, and management may be active or conservative. We present the case of a 79-year-old woman who developed SRPR of the left kidney on the fifth postoperative day of a right laparoscopic nephroureterectomy with endoscopic bladder cuff resection. Active management was decided and a ureteral catheter was placed. Symptoms improved and the patient did not develop any complications during follow-up. This case report explores SRPR, a condition with traumatic and non-traumatic causes, including urethral calculi and congenital abnormalities. SRPR is the result of a sudden increase in intraluminal pressure, often exceeding 20–75 mmHg, causing tissue tearing at the weakest urinary tract point, the fornix. In this instance, the patient experienced contralateral renal pelvic rupture following nephroureterectomy with no apparent cause for elevated intrarenal pressure. We propose that bladder irritation after ureteral cuff resection induced spasms, triggering the rupture. Diagnostic challenges arise as initial symptoms mimic renal colic, later manifesting as a urinoma. Imaging techniques, such as ultrasonography and contrast-enhanced CT, aid in the diagnosis. Treatment options encompass ureteral stenting and conservative management, with the choice depending on the patient's condition. This case underscores the significance of early recognition and management of SRPR, especially following nephroureterectomy. In conclusion, SRPR is an entity that requires immediate management. It is important to evaluate if there are any features that require active treatment.
Keywords
Spontaneous renal pelvic rupture, laparoscopic nephroureterectomy, urinoma, active management, renal function impairment
Introduction
Spontaneous renal pelvic rupture (SRPR) is a rare condition characterized by urine extravasation. This entity develops when there is a sudden elevation of intraluminal pressure. The most common etiology is obstructive urolithiasis, representing almost three-quarters of SRPR cases, followed by malignant compression, ureteropelvic junction, and bladder outlet obstruction [1]. Clinical presentation varies from asymptomatic to acute abdomen, with abdominal pain, distention, nausea, and vomiting [2]. Diagnosis is made by contrast-enhanced computed tomography (CT) or retrograde pyelography to identify urinary extravasation [3]. We present a case of left renal pelvic rupture in a 79-year-old woman on the fifth postoperative day of right laparoscopic nephroureterectomy.
Case description
A 79-year-old woman with a recent incidental diagnosis of high-grade urothelial carcinoma of the right kidney
underwent laparoscopic nephroureterectomy with conventional cuff resection. The patient presented a history of hypothyroidism
and arterial hypertension. The preoperative CT scan showed no urolithiasis or evidence of obstructive pathology in her left kidney.
The surgery was performed without intraoperative complications and the patient was discharged 72 hours postoperatively with a
bladder urinary catheter. On the fifth postoperative day, she developed diffuse abdominal pain
and consulted the urology department. The pain progressively increased and developed nausea and vomiting during observation, for
which she was hospitalized for pain control and evaluation. Analgesic medication therapy was
administered. Laboratory tests showed a white blood cell count of 10.6 mil/mm3 and an elevated creatinine level of
2.42 mg/dL. Later, her urine output decreased to 200 mL in 12 hours with associated abdominal distention. The abdominal pain persisted
despite analgesic medication therapy with 100 mg of tramadol. A bedside ultrasonography
showed an empty bladder with a well-positioned bladder urinary catheter.
Therefore, a CT scan of the abdomen and pelvis was performed in the emergency department within the first 12
hours. During the CT scan, we instilled contrast through
the bladder urinary catheter and were able to identify extraluminal contrast surrounding the left renal pelvis and
proximal left ureter. The exact site of extravasation could
not be identified and no evidence of urine extravasation
was observed in the bladder (Figure 1A). No obstructive
urolithiasis or masses were noted.
Cystoscopy with pyelography confirming contrast extravasation was performed, and a retrograde ureteral stent was
placed 6 ft retrograde. The patient's symptoms improved, pain diminished, and abdominal distension resolved
within the first 24 hours, and she was discharged 48 hours later with a bladder urinary catheter. The bladder urinary
catheter was removed on the third day and the ureteral stent at three weeks postoperatively. The creatinine level
diminished to 0.7 mg/dL on the third postoperative day. The patient did not present complications for the next
eight months (Figure 1B).
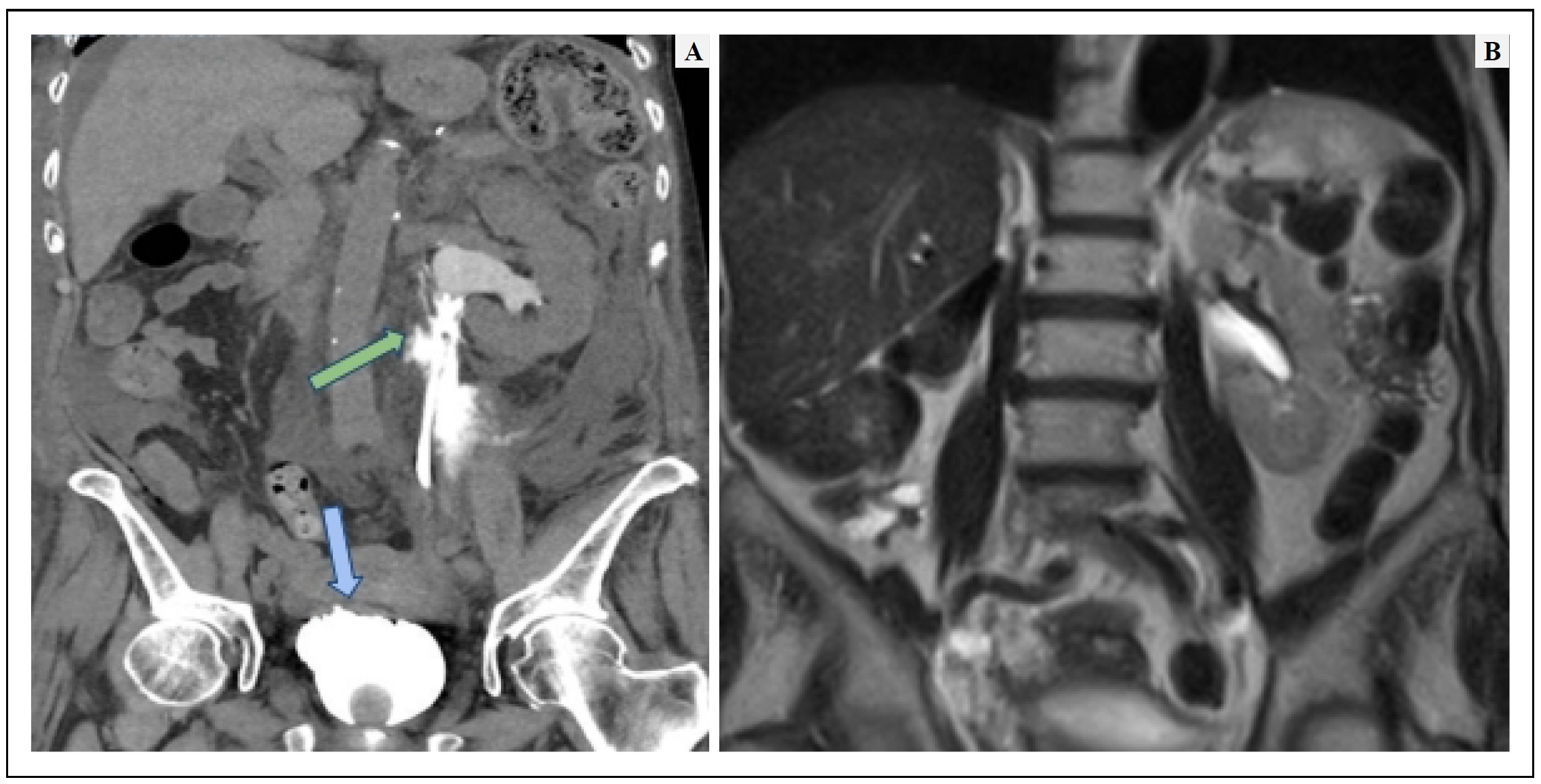
Figure 1. (A) Initial diagnostic contrast-enhanced CT of the abdomen and pelvis. The green arrow shows extraluminal contrast surrounding the left renal pelvis and the proximal left ureter. The blue arrow shows that there is no perivesical contrast, assuming that the bladder closure is not compromised. (B) Contrast-enhanced CT of the abdomen and pelvis 4 months later. No collection or urinoma is seen.
Discussion
The etiology of SRPR is divided into traumatic and nontraumatic, with ureteral calculi being the most common
(non-traumatic). Non-traumatic etiologies may include
congenital abnormalities, retroperitoneal fibrosis, urethral strictures, external compression by intra-abdominal
masses, etc [4]. SRPR is caused by a sudden elevation of
the intraluminal pressure, in this scenario the tissue cannot
adjust and ends up tearing the fornix, which is the weakest area of the urinary tract. This mechanism prevents
the kidney from suffering damage caused by sustained
elevated pressure [3]. According to You et al., the pressure
at which fornix rupture occurs ranges from 20–75 mmHg
[5].
In our case, the patient presented with contralateral renal
pelvic rupture after nephroureterectomy. No signs of compromise of the left renal unit and ureter were found during
surgery. Moreover, there were no other known causes for
the sudden elevation of intrarenal pressure leading to tissue tearing. We believe that irritation of the bladder resulting
from the resection of the ureteral cuff led to bladder
spasms. The spasms may have potentially induced a sudden surge in pressure within the kidney, resulting in the
rupture in the renal pelvis, an area where the renal parenchyma lacks support [6]. We
suspect that ureteral reflux was the cause behind the SRPR and that closure of the
bladder wall prevented any leakage. However, it remains
unclear why the rupture occurred despite using a permeable bladder urinary catheter to reduce urinary pressure.
The symptomatology of SRPR, in the beginning, is similar to renal colic, an acute pain in the lower back, but when
the fornix breaks this disappears due to the decrease in intraluminal pressure. Later, the symptoms are secondary to
the urinoma and range from asymptomatic to mimicking
an acute abdomen with peritoneal irritation and abdominal distention, nausea, and vomiting, making it difficult
to diagnose without imaging [7]. In our case, the patient
developed pain associated with abdominal distention and nausea.
Ultrasonography is a good tool for an initial approach.
It is fast, cheap, radiation free, and helps us rule out differential diagnoses such as appendicitis and renal colic. In
SRPR, hydronephrosis is absent and clear fluid collections can be identified. Also, in our case, the bladder was empty
and urine output diminished despite adequate hydration of the patient. Contrast-enhanced CT is the optimal imaging
modality to identify urinary leakage and urinoma formation. Delayed acquisition of images is essential to allow
visualization of extravasated contrast in the study. In the
present case, the patient had a Foley catheter in the bladder, therefore we instilled contrast through the urinary
catheter, where we were able to observe contrast extravasation in the upper urinary tract rather than in the bladder
due to the vesicoureteral reflux created. This allowed us to determine that the urinoma originated in the upper urinary
tract and that the bladder sutures from the bladder cuff resection were not compromised.
SRPR treatment can be active or conservative. Active treatment is made by placing a ureteral stent, which can be
performed retrograde or antegrade, in our case the ureteral stent was placed retrograde. The stent drains the urine
from the kidney to the bladder and prevents the urinoma
progression, and promotes the healing of the urothelial tissue [7]. Conservative management has great results, but it
should not be chosen when the patient with fever, leukocytosis, positive urine cultures, emesis, or renal
dysfunction [8]. In these scenarios, active treatment is mandatory, as in this case.
Conclusions
SRPR is an entity in which we must discard the differential diagnosis that requires immediate treatment. It is crucial to evaluate if there are any features that require active treatment, on the other hand, conservative management is feasible.
Declarations
Acknowledgments
None.
Financial support and sponsorship
None.
Conflict of interest statement
No conflict of interest.
Ethical approval and informed consent
The patient has provided an informed consent for publication of images and information in this study.
References
1. Yanaral F, Ozkan A, Cilesiz NC, & Nuhoglu B. Spontaneous rupture of the renal pelvis due to obstruction of pelviureteric junction by renal stone: a case report and review of the literature. Urol Ann, 2017, 9(3): 293-295. [Crossref]
2. Pampana E, Altobelli S, Morini M, Ricci A, D'Onofrio S, & Simonetti G. Spontaneous ureteral rupture diagnosis and treatment. Case Rep Radiol, 2013, 2013: 851859. [Crossref]
3. Blas L, Bonanno N, Mieggi M, Ringa M, Contreras P, & Ameri CA. Risk factors for contrast extravasation in renal colic. Arch Esp Urol, 2022, 75(3): 256-261.
4. Chen GH, Hsiao PJ, Chang YH, Chen CC, Wu HC, Yang CR, et al. Spontaneous ureteral rupture and review of the literature. Am J Emerg Med, 2014, 32(7): 772-774. [Crossref]
5. You JS, Chung YE, Lee JY, Lee HJ, Chung TN, Park YS, et al. The spontaneous rupture of the renal fornix caused by obstructive nephropathy. J Emerg Med, 2012, 43(3): 488- 489. [Crossref]
6. Prem K, Smita S, Pankaj K, & Pragya P. Surgical management of spontaneously ruptured kidney with peritonitis due to neglected renal and ureteric calculi. BMJ Case Rep, 2021, 14(6): e240910. [Crossref]
7. Al-Mujalhem AG, Aziz MS, Sultan MF, Al-Maghraby AM, & Al-Shazly MA. Spontaneous forniceal rupture: can it be treated conservatively? Urol Ann, 2017, 9(1): 41-44. [Crossref]
8. Morgan TN, Bandari J, Shahait M, & Averch T. Renal forniceal rupture: is conservative management safe? Urology, 2017, 109: 51-54. [Crossref]