Open Access | Case Report
This work is licensed under a Creative
Commons Attribution-ShareAlike 4.0 International License.
Robotic-assisted transvesical excision of recurrent bladder leiomyoma with intraoperative ultrasound guidance
* Corresponding author: Ayman Ali
Mailing address: Portsmouth Hospitals NHS Trust, Portsmouth,
United Kingdom; PO6 3LY.
Email: dr.aymansaad@hotmail.com
Received: 18 April 2023 / Revised: 28 June 2023 / Accepted: 11 July 2023 / Published: 26 September 2023
DOI: 10.31491/UTJ.2023.09.011
Abstract
Leiomyoma of the urinary bladder is uncommon benign tumor with a wide range of clinical presentations. Surgical excision remains the definitive treatment of leiomyoma with excellent outcomes. Seldom literatures reported the use of robotic-assisted surgical techniques for its excision. A 51-year-old woman presented with frequent episodes of visible hematuria in consistence with lower urinary tract symptoms. The initial diagnosis was a urinary tract infection. However, symptoms did not resolve even with the proper antibiotics. After further investigations a soft tissue density mass measuring 20 × 23 × 20 mm within the left posterior wall of the urinary bladder extending towards the bladder neck was found. The histological finding of the transurethral resected biopsy of the mass revealed a benign submucosal leiomyoma of the bladder with no evidence of any malignancy. Using the Intuitive Da Vinci X system the tumor was excised using the ultrasound guidance to define the tumour margins, sparing the left ureteric orifice and ureter. The patient was discharged home on the day of surgery, with a urethral catheter in place. The catheter was successfully removed after 10 days, with cystogram prior confirming no leakage. The ureteric stent was removed by flexible cystoscopy two weeks later. The final histology was reported as a bladder leiomyoma with no evidence of malignant features and negative circumferential resection margins. Herein, in the current case we present a safe and effective technique for the excision of recurrent bladder leiomyoma using the robotic-assisted transvesical approach with intraoperative ultrasound guidance.
Keywords
Bladder, leiomyoma, robotic, partial cystectomy
Introduction
Bladder leiomyoma, a benign smooth muscle tumor, represents 0.43% of all bladder neoplasms. The clinical presentation is variable, depending on the location and size
of the tumour [1]. Patients may present with hematuria
or storage urinary symptoms; however, others may be asymptomatic discovering the lesion incidentally. The management of leiomyomas is mainly surgical, with different
approaches from transurethral resection to open segmental
resection or partial cystectomy described [2]. Bladder
leiomyoma were exceptionally resected in certain female
cases through trans-vaginal approach [3]. Laparoscopic
partial cystectomy was also suitable [4]. However, there
are very limited data on the robotic excision of bladder
leiomyoma [5].
Over the past 20 years, the application of robotic assisted
technology in urological oncology has totally transformed
the urologists’ manner for approaching tumors. Being a
feasible and safe technique with comparable oncologic
outcomes and increased surgeon comfort, convinced
urologists to make the robotic-assisted surgeries their top
choice in urological cancers [6].
The use of robotic-assisted surgical techniques in urology
offered many benefits over the established open surgery
and laparoscopy. As, in addition to the benefit of 3D
visualization of the surgical field, robotics allows good
motion scaling, thus large movements at the console are
translated into a very small motions at the operative site.
Furthermore, robots terminated the fulcrum effect of laparoscopic surgery, in which the movement of the instrument tips went in an opposite direction to the surgeon’s
hand; however with robotic instruments the movement
of instrument tips in the body goes in the same direction
as the surgeon’s hands in the console so that the degree of freedom during the operation is enhanced [7]. In addition, robotics-assisted surgery eliminates tremors, reduces
surgeon fatigue with more ergonomic positioning, so that
allowing precise and smooth surgery. Accordingly, robotic
assisted technique offers a higher dexterity and accuracy
with less surgical complications [8].
There is an expanding use of the intraoperative ultrasound
to handle and guide different intraoperative interventions. The main goal is the better visualization and location of lesions in order to provide interactive and precise
information during surgery, thus, helping surgeons for a
precise guidance during operation and in turn a potentially
improving of the outcomes [9].
In our case, we introduce a robotic-assisted intravesical
approach to excise bladder leiomyoma using intraoperative ultrasound guidance for accurate demarcation of lesion margins.
Case presentation
Our patient was a 51-year-old lady who presented with recurrent episodes of visible hematuria. She had no history
of smoking, no occupational risk factors, and no family
history of urological cancer. Her performance status was
zero and she was on no medications. She was initially
treated with antibiotics due to co-existing lower urinary
tract symptoms thought to be due to urinary tract infection
(UTI), but was subsequently referred to the urology clinic
due to non-resolution of these symptoms and ongoing hematuria.
Initial flexible cystoscopy was inconclusive, due to poor
views with a bladder full of debris. CT urography (CTU)
demonstrated two relatively large distal ureteric stones
measuring 15 mm and 10 mm in the longest diameter with
proximal hydroureteronephrosis and non-obstructing renal
stones in the contralateral kidney. The scan also identified
a soft tissue density mass measuring 20 × 23 × 20 mm
within the left posterior wall of the bladder extending toward the bladder neck (Figure 1).

Figure 1. CTU showed the soft tissue density mass within the left posterior wall of the bladder extending toward the bladder neck.
She subsequently proceeded to rigid cystoscopy with
transurethral resection biopsies and ureteroscopic LASER
fragmentation of the right ureteric stones. Cystoscopy revealed a normal bladder urothelium. The area of concern
on the CTU appeared as a bulge with, normal urothelium
adjacent to the left ureteric orifice. Loop resection biopsies
were taken from the bulging area and sent for histological
analysis. The tissue was relatively avascular on cutting.
Histology demonstrated a benign submucosal leiomyoma
of the bladder with no evidence of any malignancy. Due
to the anatomical position of the leiomyoma (adjacent to
the ureteric orifice and bladder neck) and the absence of
malignant features, a conservative management approach
was adopted with a plan for surveillance cystoscopic assessment.
Her first check flexible cystoscopy revealed a calcified
deposit in the region of her previous resection area with
progression in size. She underwent further transurethral
resection, which again reported benign leiomyoma on
histology. She continued on conservative follow-up, with
6-monthly imaging with CTU and magnetic resonance
imaging (MRI) demonstrating stable appearance of her
bladder leiomyoma for almost 14 months. Despite this,
she experienced increasing urinary storage symptoms
and hematuria. Subsequent CTU showed an increase in
both the intravesical and extravesical components and
calcifications (Figure 2). In view of her increasingly
bothersome symptoms and radiological progression, she
was counseled regarding surgical excision. It was felt that
continued conservative management risked further increase in size with resultant surgery being more complex
with a higher risk of functional complications. The patient
agreed to undergo robotic-assisted transvesical bladder
leiomyoma excision.

Figure 2. CTU showed an increase in both the intravesical and extravesical components and calcification.
Using the Intuitive Da Vinci X system, the patient was docked with the robot in 20° Trendelenburg using a standard cystectomy port placement, with a urinary catheter in place. The left side of the bladder was mobilized down to the endo-pelvic fascia with no division of the vascular pedicles. The bladder was then released anteriorly and dropped obliquely, leaving the right side undisturbed. The bladder was filled with saline and the tumor was characterized using intracorporeal USS. The bladder was opened with a cranio-caudal oblique incision down to the anterior border of the tumor at the bladder neck, again with USS guidance. Due to the proximity of the tumor to the left ureteric orifice, a 6/24 JJ stent was inserted. The tumor was then excised using USS guidance to define the tumor margins, sparing the left ureteric orifice and ureter. The bladder was closed using a single layer 3/0 V-Loc with bladder neck reconstruction. The patient was discharged home on the day of surgery with a urethral catheter in place (Figure 3A–E).
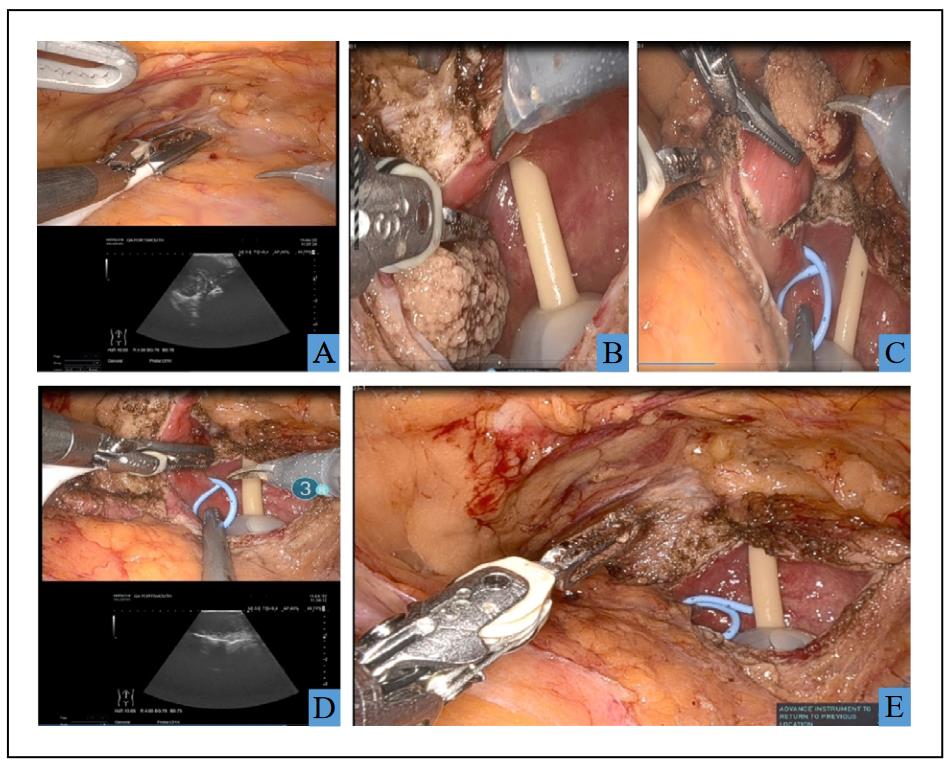
Figure 3. (A) Identification of the extent of the leiomyoma by ultrasound extravesically; (B) Cystostomy and visualisation of the boundaries of the lesion; (C) Stenting the left ureter and demarcation of the cutting margins; (D) confirmation of the margins by ultrasound intravesically prior to excision; (E) Bladder after excision of the lesion.
The catheter was successfully removed after 10 days, with cystogram prior confirming no leakage (Figure 4). The ureteric stent was removed by flexible cystoscopy two weeks later. The final histology was reported as a bladder leiomyoma with no evidence of malignant features and negative circumferential resection margins. The patient was reviewed 6 weeks postoperatively and reported to be fully continent with no ongoing lower urinary tract symptoms, and was discharged from follow-up.
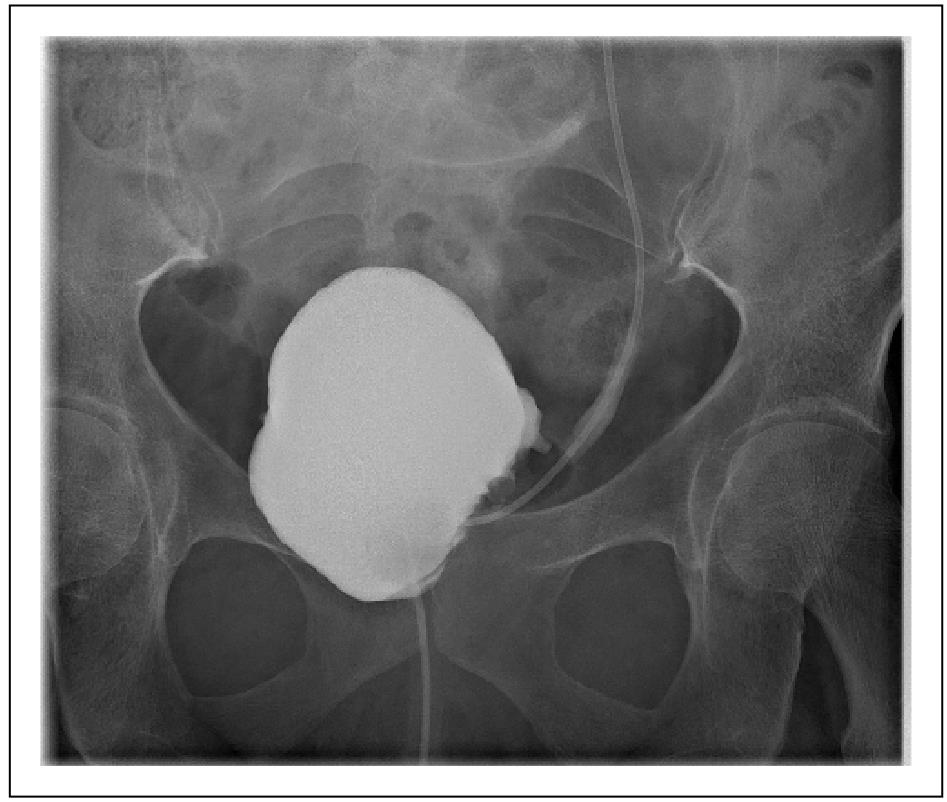
Figure 4. Cystogram prior catheter removal confirming no leakage.
Discussion
Despite being a rare neoplasm, bladder leiomyoma is the
most common soft tissue benign non-epithelial tumor of
the urinary bladder with variable clinical presentations
[10]. Our patient had a submucosal bladder leiomyoma
adjacent to the ureteric orifice and bladder neck. Nearly
80% of the affected patients suffered from symptoms
ranging from irritative to obstructive symptoms with associated hematuria, which comes in line with the clinical
presentation of our case [11]. On the other hand, other
patients were rarely asymptomatic [12].
Although bladder leiomyoma has benign nature, it may
behave as a malignant tumor, thus surgical removal using different surgical approaches is often preferred [11].
Surgical excision remains the definitive treatment for leiomyoma with excellent outcomes [1, 12]. However, laparoscopy, transurethral resection, and transvaginal resection
using a hysteroscope are also other options.
Robotic-assisted excision of bladder leiomyomas provides
the opportunity for this definitive treatment to be delivered
in a minimally invasive way, providing all of the well-described advantages to patients of minimally invasive surgery (MIS) [5]. Literature on the excision of bladder leiomyomas using robotic approaches is limited. However, the
use of the transvesical approach for leiomyoma excision
was reported [13]. Interestingly, the use of intraoperative
ultrasound guidance is a valuable tool that helps urologists
to implement different complex robotic procedures with
improved surgical outcomes [14]. Our procedure utilized
the addition of intracorporeal USS guidance that gives the
additional benefit of precise tumor identification, limiting
the degree of bladder mobilization required, providing
clear margin delineation, which should lead to a reduced
risk of functional bladder sequelae and incomplete resection. Given the availability of robotics in modern urology,
early use of robotic resection and reconstruction should be
considered over other techniques and conservative management.
Our case sheds light on two clinical findings; first, the
feasibility of robotic bladder leiomyoma excision using
the transvesical approach; second, utilizing intraoperative
ultrasound guidance during the procedure assisted us in
performing a precise and safer excision of the leiomyoma.
Hence, to the authors’ knowledge, there are very few
documented cases on the use of robotic-assisted bladder
leiomyoma excision in the literature; however, our case is
the first to describe the additional benefits of combining
robotics with intracorporeal USS guidance.
Conclusions
Leiomyomas are rare benign neoplasms of the bladder, which present with variable symptoms and may even be asymptomatic. Excision via a robotic transvesical approach offers a minimally invasive option for complete resection with minimal functional impact.
Declarations
Acknowledgments
NO grant or funding has been received to support this research from any funding agency.
Author contributions
Ali A: substantial contributions to the conception, design, methodology, drafting, writing, editing, reviewing, and final revision of the study; Wilby D: supervision, reviewing, and final revision of the work; Dossantos J: substantial contribution to the methodology of the work; Robinson R: supervision, methodology, reviewing, editing, and final revision of the work.
Financial Support and Sponsorship
None.
Conflict of interest statement
No conflict of interest.
Ethical Approval and Informed consent
According to institutional regulations, the patient has provided an informed consent for publication of images and information in this study. Any procedure performed was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
References
1. Caliskan S, & Sungur M. Bladder Leiomyoma. J Coll Physicians Surg Pak, 2017, 27(3): 189-190.
2. Zachariou A, Filiponi M, Dimitriadis F, Kaltsas A, & Sofikitis N. Transurethral resection of a bladder trigone leiomyoma: a rare case report. BMC Urol, 2020, 20(1): 152-157. [Crossref]
3. Nagai N, Katayama Y, Iguchi M, & Esa A. [A case of urinary retention due to a female paraurethral leiomyoma]. Hinyokika Kiyo, 1988, 34(4): 696-700.
4. Murota T, Komai Y, Danno S, Fujita I, Kawakita M, & Matsuda T. Endoscopic partial cystectomy for bladder leiomyoma using retroperitoneoscopic and transurethral procedures. Int J Urol, 2002, 9(3): 190-192. [Crossref]
5. Baird BA, Ericson CA, Augustus A, Geldmaker L, Wajswol E, & Young PR. Robotic transvesical bladder leiomyoma excision. Urol Case Rep, 2022, 43: 102054. [Crossref]
6. Skolarus TA, Zhang Y, & Hollenbeck BK. Robotic surgery in urologic oncology: gathering the evidence. Expert Rev Pharmacoecon Outcomes Res, 2010, 10(4): 421-432. [Crossref]
7. Kim VB, Chapman WH, Albrecht RJ, Bailey BM, Young JA, Nifong LW, et al. Early experience with telemanipulative robot-assisted laparoscopic cholecystectomy using da Vinci. Surg Laparosc Endosc Percutan Tech, 2002, 12(1): 33-40. [Crossref]
8. Murphy D, Challacombe B, Khan MS, & Dasgupta P. Robotic technology in urology. Postgrad Med J, 2006, 82(973): 743-747. [Crossref]
9. Porpiglia F, Checcucci E, Amparore D, Piramide F, Volpi G, Granato S, et al. Three-dimensional augmented reality robot-assisted partial nephrectomy in case of complex tumours (PADUA ≥10): a new intraoperative tool overcoming the ultrasound guidance. Eur Urol, 2020, 78(2): 229-238. [Crossref]
10. Park JW, Jeong BC, Seo SI, Jeon SS, Kwon GY, & Lee HM. Leiomyoma of the urinary bladder: a series of nine cases and review of the literature. Urology, 2010, 76(6): 1425- 1429. [Crossref]
11. Yoshioka T, Kawakita M, & Kameoka H. Cystoscopeassisted laparoscopic enucleation of a large progressive bladder leiomyoma. J Endourol Case Rep, 2019, 5(3): 120-123. [Crossref]
12. Tobias-Machado M, Pazeto CL, & Borges RC. Robot-assisted transvesical partial cystectomy for leiomyoma of bladder trigone. Int Braz J Urol, 2020, 46(2): 300. [Crossref]
13. Gok A. Transurethral resection of a large urinary bladder leiomyoma: a rare case report. Urol J, 2017, 14(4): 4052- 4054.
14. Ukimura O, Okihara K, Kamoi K, Naya Y, Ochiai A, & Miki T. Intraoperative ultrasonography in an era of minimally invasive urology. Int J Urol, 2008, 15(8): 673-680. [Crossref]