Open Access | Case Report
This work is licensed under a Creative
Commons Attribution-ShareAlike 4.0 International License.
A case of duodenal perforation and pancreatic bleeding after flexible ureteroscopy for right renal pelvis UTUC
* Corresponding author: Stefano Spagna
Mailing address: San Raffaele Hospital, Via Olgettina, 60, 20132,
Milan, Italy.
Email: spagnastefano92@gmail.com
* Corresponding author: Guido Giusti
Mailing address: San Raffaele Hospital, Via Olgettina, 60, 20132,
Milan, Italy.
Email: drguidogiusti@gmail.com
Received: 17 July 2023 / Revised: 08 August 2023 / Accepted: 29 August 2023 / Published: 26 September 2023
DOI: 10.31491/UTJ.2023.09.012
Abstract
Upper tract urothelial carcinoma (UTUC) can be managed by flexible ureteroscopy (f-URS) and tumor laser ablation if kidney-sparing surgery is possible. This procedure can be affected by minor to serious complications, including life-threatening sepsis, ureteral strictures, and ureteral and renal pelvis injuries. Here, we present the case of a 53-year-old man with history of high-grade right renal pelvis and bladder tumor who undergone multiple endoscopic treatments and has already refused radical surgery. F-URS and laser ablation with Thulium: YAG laser for UTUC recurrence of the right renal pelvis was performed, but the procedure was stopped due to significant bleeding which impaired vision. Postoperatively, the patient developed hematemesis and hemodynamic instability due to duodenal lesion and active bleeding documented on computed tomography scan. An emergency exploratory laparotomy was performed to drain the hemoperitoneum, repair the duodenal lesion, and concurrent radical right nephroureterectomy was carried out. A second surgery was necessary for repairing duodenal fistula. After one week, the patient presented again with recurrent hematemesis and hemorrhagic shock. He underwent angiography and selective embolization of the duodenal branch of the superior mesenteric artery and as well as branches of the gastroduodenal artery successfully and the patient recovered with no other complications. This is the first case of duodenal perforation and pancreatic bleeding due to flexible ureteroscopy and laser ablation of right renal pelvic urothelial carcinoma.
Keywords
UTUC, flexible ureteroscopy, laser ablation, bleeding, duodenum
Introduction
Upper tract urothelial carcinoma (UTUC) is an uncommon neoplasm and accounts for only 5–10% of all urothelial carcinomas [1]. Kidney-sparing endoscopic management of UTUC is a feasible option in patients with a solitary kidney and/or impaired renal function, as well as in cases of bilateral or low-risk tumors [2]. Flexible ureteroscopy (f-URS) can be used to perform diagnostic biopsies as well as ablate the tumor in the ureter or renal pelvis using laser technology. The potential risks of this procedure range from minor complications such as urinary tract infection (UTI) and hematuria to serious complications including life-threatening sepsis, ureteral strictures, and ureteral and renal pelvic injuries. [3, 4]. Here, we present the first described case of duodenal perforation and pancreatic bleeding due to flexible ureteroscopy and laser ablation of right renal pelvic urothelial carcinoma.
Case description
A 53-year-old man, with a significant medical history of
peptic ulcer disease on treatment with proton-pump inhibitor (PPI) was referred to the urology department for highrisk UTUC involving the right renal pelvis and ureter. He
was first treated in 2017 for right renal pelvis tumor and
histology showed pTa G3 urothelial carcinoma. He refused
right nephroureterectomy. During a follow-up period of 2
years, he underwent at least six endourological procedures
(ureteroscopy and biopsies and endoluminal instillation of
mitomicin C through MJ stent) to treat recurrent UTUC.
He has also undergone multiple endoscopic bladder resections (TURB) for concurrent high grade bladder cancer followed by intravesical immunotherapy with BCG. Considering the extent of the disease, multiple recurrences and
the limitations of the endoscopic treatment, he was repeatedly offered right radical nephroureterectomy (RNU), but
the patient declined radical treatment.
In February 2019, he underwent right f-URS. A wireless
and sheathless “no-touch” technique was performed using an 8.5 F flexible digital ureteroscope (Flex-XC, Karl
Storz, Tuttlingen, Germany) [5]. Multiple papillary lesions were found in all the major calyces and the renal
pelvis. Biopsy was performed with a tipless 1.9 F nitinol
basket, followed by tumor ablation with a 200µm fiber for
thulium: YAG (Tm:Yag) laser (Cyber-TM, Quanta System, Samarate, Italy). The laser was set to 10 watts for the
procedure. After an initial bloodless ablation, endoscopic
vision deteriorated due to the development of significant
bleeding. The laser power was increased up to 30 watts in
the effort of controlling the ongoing bleeding, but unsuccessfully. The decision was then made to terminate the
procedure and a single J ureteral stent was placed under
fluoroscopy without relevant findings on retrograde pyelography.
On postoperative day (POD) 1, the patient presented with
acute hematemesis and hematuria. Computed tomography
(CT) scan showed a large clot in the right renal pelvis clot.
Duodenoscopy was also carried out in emergency and the
patient was found to have a 1 cm perforation in the second
part of the duodenum. This was treated endoscopically
with injection of epinephrine to remove some clots adhering to the lesion and then 4 metallic clips were applied to
close it (Figure 1).

Figure 1. EGDS and application of metallic clips for duodenal bleeding.
Unfortunately, the next day the patient developed hemodynamic instability and a drop of hemoglobin from 13 to 9 g/dL. An emergency exploratory laparotomy was performed with intraoperative findings of massive hemoperitoneum due to active bleeding from a 1 cm perforation of the anterior duodenal wall and from the pancreatic head (Figure 2).
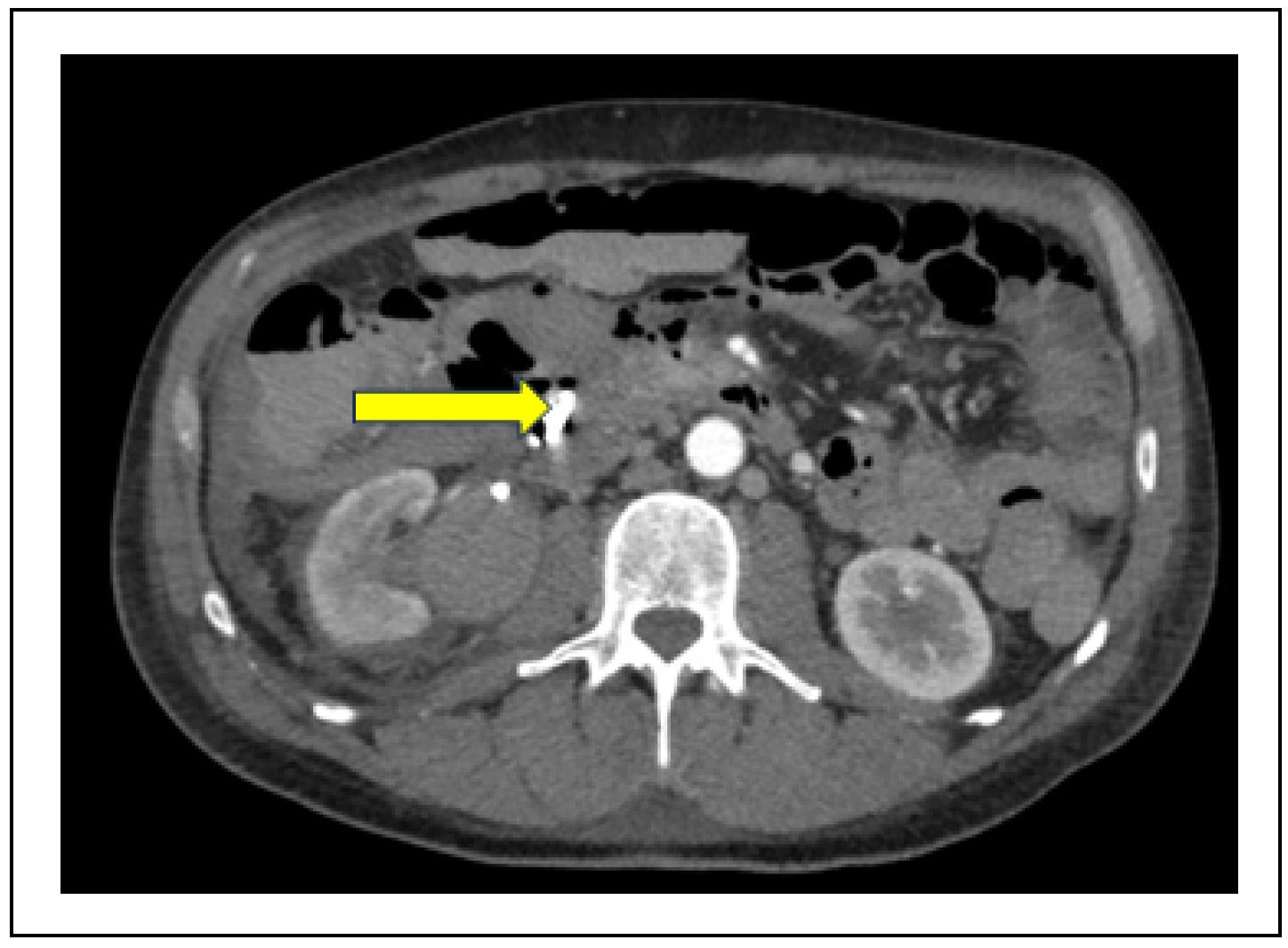
Figure 2. CT scan and hemodynamic instability: active bleeding and hemoperitoneum.
After the abdomen was washed out, the pancreatic head bleeding was controlled with hemostatic sutures and the duodenal perforation was repaired. A right radical nephroureterectomy was also performed at the same setting. The patient received 4 pints of packed cell transfusion during surgery. Postoperatively, the patient was clinically stable but was admitted to the intensive care unit for monitoring. On POD 8, the drain output was suspicious for enteric content, hence a CT scan and gastrografin swallow were performed. The scans demonstrated a duodenal fistula. The patient was then brought back into the operating room for repair of the duodenal fistula (Figure 3).
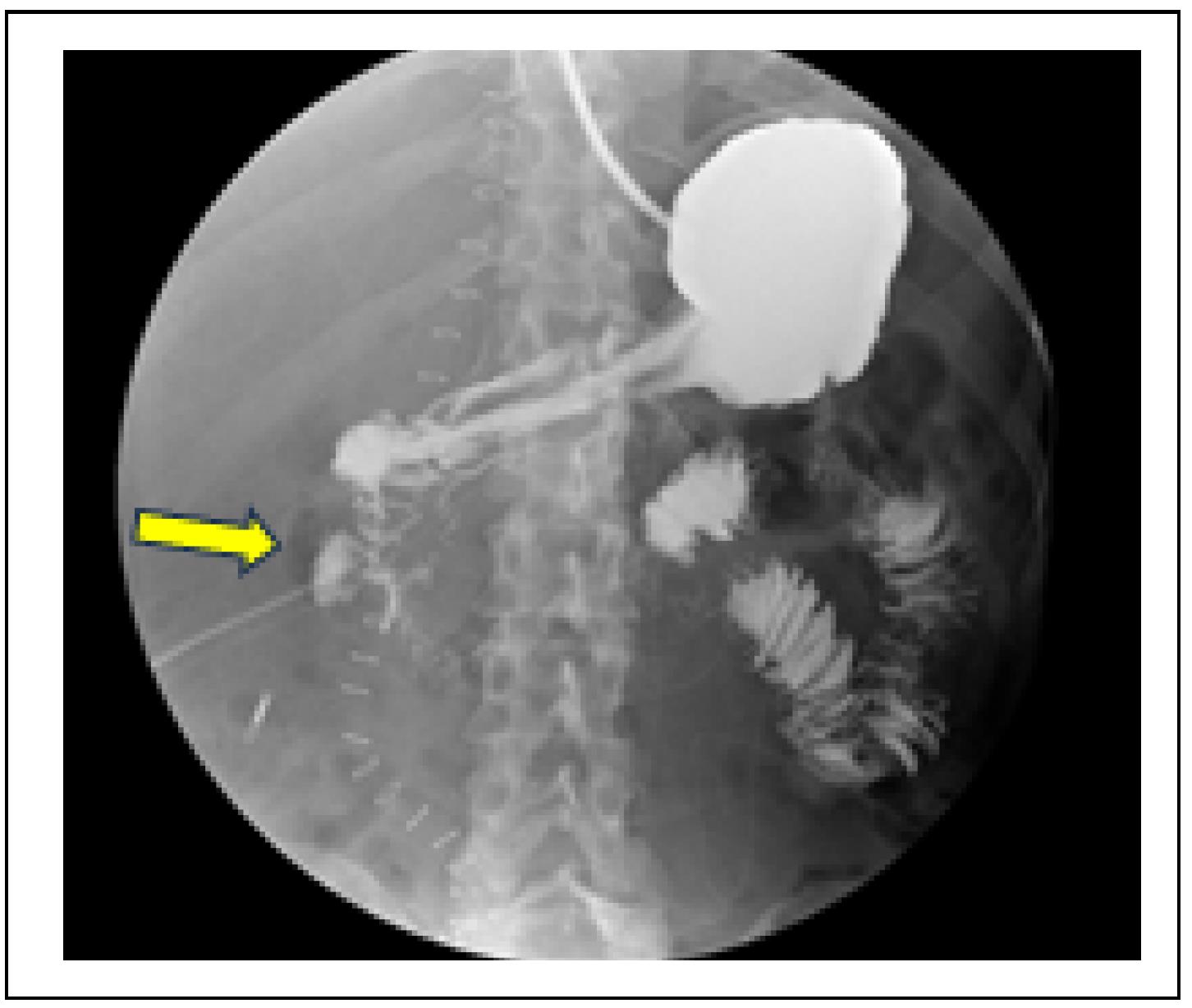
Figure 3. Abdomen X-Ray with gastrografin: duodenal fistula.
The patient recovered gradually following the second duodenal repair surgery. However, after one week, the patient presented with recurrent hematemesis and hemorrhagic shock. A CT angiogram documented recurrent active bleeding near the previous metallic clips used in the repair of the duodenal perforation. A celiac and mesenteric arteriography through femoral puncture was carried out and the patient underwent selective embolization of the duodenal branch of the superior mesenteric artery and as well as branches of the gastroduodenal artery successfully by microcoil placement (Figure 4 & 5).
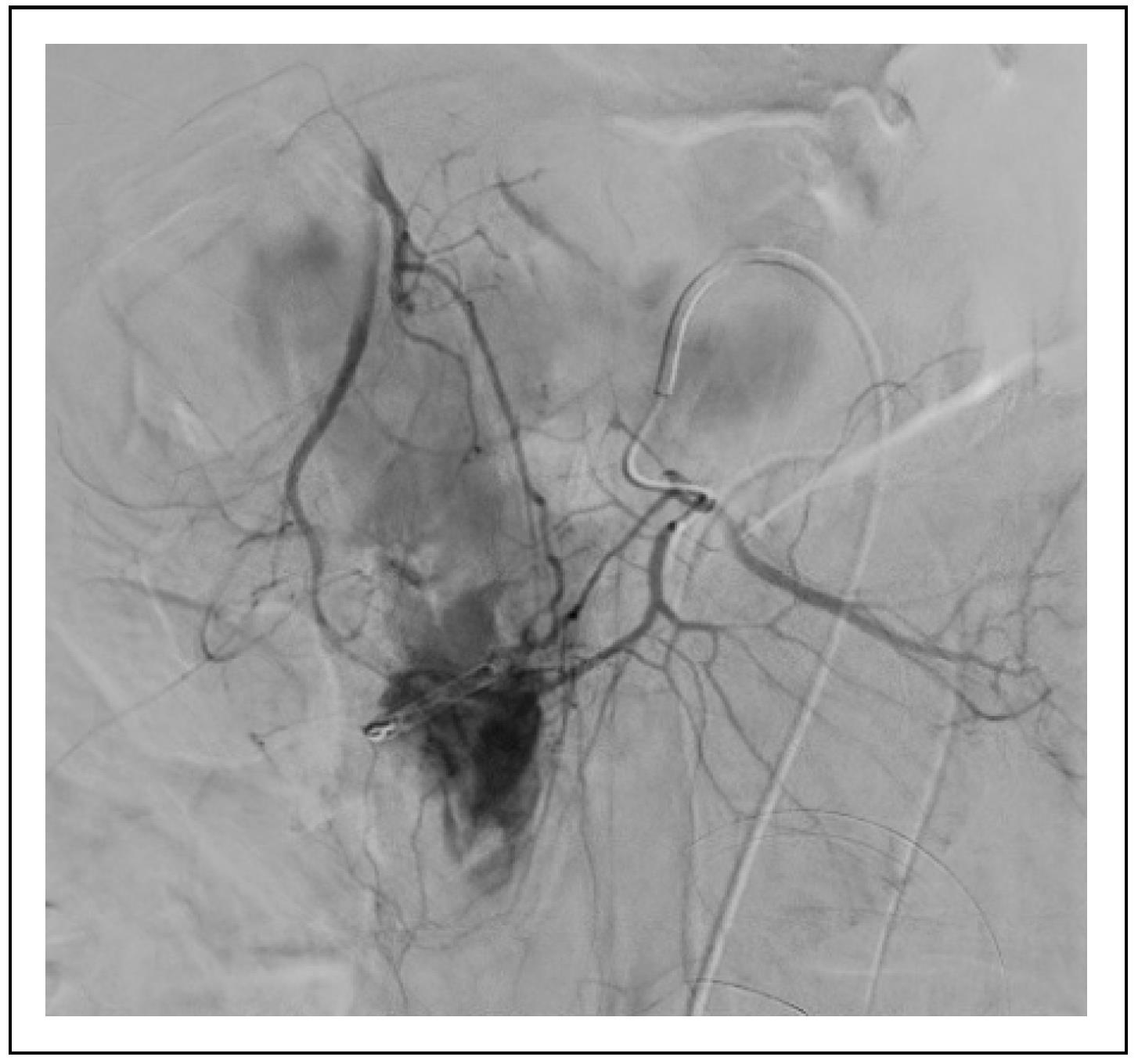
Figure 4. Active bleeding from mesenteric and gastroduodenal artery at angiography.

Figure 5. Hemostasis after selective angioembolization.
Subsequently, the patient recovered without further hematemesis and hemoglobin levels remained stable. He
was discharged from the hospital on the 30th postoperative
day since first surgery.
Final histologic examination of the right radical nephroureterectomy specimen was reported to be pTis urothelial
carcinoma of the right renal pelvis. He is now still on
periodic follow-up with flexible cystoscopy, with the last
bladder recurrence in May 2022.
Discussion
According to the current European Association of Urology (EAU) guidelines, RNU remains the gold standard
for high-risk UTUC [2]. Nevertheless, conservative treatment should be considered as an option in patients with
imperative indications for kidney-sparing surgery, such as
in solitary kidney, bilateral UTUC, or chronic renal failure, as well as for clinically low-risk UTUC [6]. In some
cases where the patient chooses to avoid radical surgery,
it is important to ensure that the patient is aware of the
possible risks of disease progression and the necessity of
close endoscopic follow-up. To date, f-URS is useful for
both endoscopic tumor ablation and a close postoperative
surveillance of the UTUC after kidney-sparing treatment
[7]. Endoscopic procedures in the upper urinary tract are
associated with the risk of trauma to the ureter and pyelocaliceal system [8]. These injuries are classified as a major
complication of f-URS and are usually reported to be due
to the use of a ureteral access sheath (UAS) [4]. This is
the reason why we usually prefer to apply a “no touch”
technique when performing f-URS for UTUC and avoid
traumatism on the ureteral wall that can cause lesions or
bleeding. In the described case, therefore, the pelvic wall
perforation must have been due to tumor laser ablation
with thulium: YAG laser in the setting of poor visibility
due to significant bleeding. In endourology, adequate irrigation is fundamental. UAS are very useful to guarantee
good irrigation and consequently a good intraoperative vision. According to this concept, more evidence is appearing in the literature to encourage this practice also during
procedures for UTUC. Moreover, Douglawi et al. demonstrate a protective role for UAS in bladder recurrence in
urothelial cancer [9].
In a review of URS complications by Linehan et al. [3],
the authors found rates of bleeding ranging from 1.6%
to 27.3%, but only a few were serious enough to require
hospitalization and/or blood transfusion. Bleeding during
URS treatment for UTUC was more frequently associated
with patients who had previously received adjuvant instillations [3]. Renal pelvic wall perforation is an even rarer
event, with rates varying from 1.3% to 7.4% of cases.
There are also some disease-related factors to consider,
such as tumor location and invasiveness. In this case, the
patient presented with a large tumor involving the entire
anterior wall of the renal pelvis and all the calyces, and
the diseased urothelium is more prone to injury and perforation.
The choice of laser for the ablation of the tumor also contributes to the risk of injury to the collecting system, and
hence the characteristics of the laser must be considered.
Proietti et al. evaluated the effects of both Tm:YAG and
Holmium:YAG (Ho:YAG) lasers on upper urinary tract
urothelium, with a focus on incision depth and coagulation
area [10]. This study showed a lower penetrative power
for Tm:YAG (due to lower peak power, better water absorption and continuous mode) compared to Ho:YAG,
with a higher coagulation effect without excessive carbonization of tissue. Despite these advantages in choosing the
Tm:YAG laser, a major bleeding was encountered in the
described case, resulting in poor vision that led to the inadvertent perforation of the renal pelvis with the involvement of the duodenum and the pancreas. In addition, the
patient had a history of peptic ulcer disease, and this underlying pathology may have contributed to the fragility
of the duodenal wall. The second segment of duodenum
“C” lies over the right renal hilum, hence its proximity resulted in the injury with the renal pelvis perforation (Figure 6).
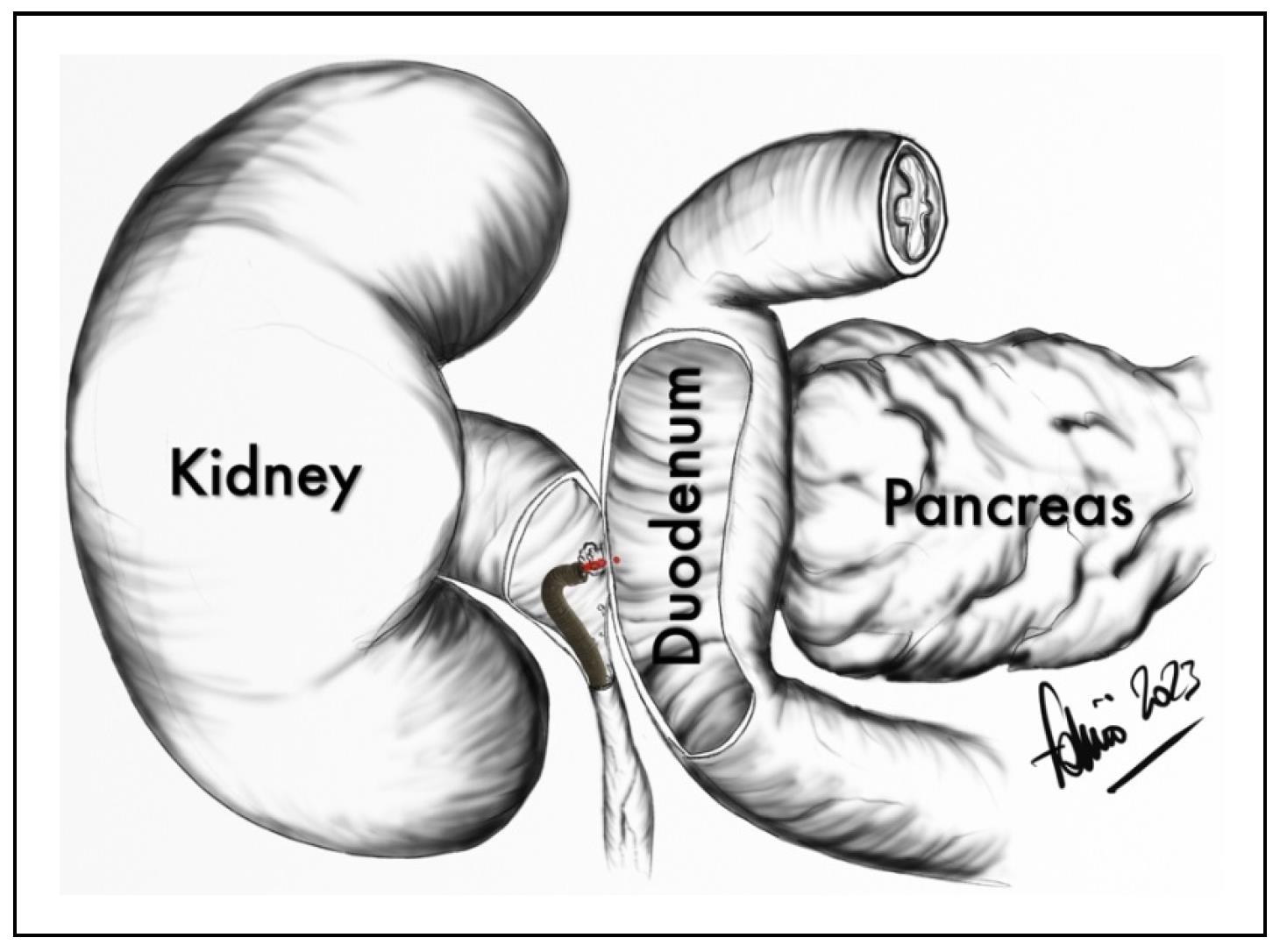
Figure 6. Anatomical relationship between the right renal pelvis, the II portion of duodenal C loop, and the pancreatic head.
Duodenal perforation is a rare condition, but is associated
with high morbidity and mortality, ranging from 8% to
25% [11]. Isolated duodenal injuries after trauma are rare,
and the pancreas is frequently injured concomitantly due
to their close anatomical relationship. The second segment
of the duodenum is the most commonly injured part (36%).
When isolated minor CT findings are discovered, the clinical case can be managed conservatively with close monitoring, otherwise patients usually require surgical intervention. Endoscopic management with supportive medical
therapies is the first-line therapy for gastrointestinal upper
bleeding and is highly effective. The standard approach
includes pre-injection of the bleeding area with epinephrine before removing clots with a cold guillotining snare
technique. Numerous meta-analyses indicate that adding a
second procedure, such as a second injectant agent (alcohol, thrombin, or fibrin glue), thermal contact, or clips, is
superior to epinephrine injection alone [12]. This was the
treatment of choice, and in this case, the endoscopic management appeared adequate enough to solve the bleeding
and repair the defect without surgery (primary repair [13]
vs. duodenectomy [14]). However, approximately 10% of
all patients will either continue to bleed or experience rebleeding within 48 h of the endoscopic treatment. While
surgical therapy has historically been considered the next
line of treatment for upper GI refractory bleeding, angioembolization has now become the next line of therapy [15].
Given the dual supply to the duodenum from the celiac
trunk (GDA), as well as the superior mesenteric artery
(through the inferior pancreaticoduodenal arcades), embolization that is distal to the site, and proximal to the bleeding is needed for effective embolization [15]. In this case,
the placement of the coils was able to stop the contrast
medium spreading seen on the arteriography and was able
to stop the bleeding.
The main complication after transarterial embolization is bowel ischemia. Although the upper gastrointestinal tract
has a rich collateral blood supply, ischemic complications can still occur in 7 to 16% of cases [12], in which
unfavourable evolution is very likely, but fortunately this
was not the case. As a matter of fact, the following postoperative course was finally uneventful. In literature, a
very limited number of cases of iatrogenic injury of the
duodenum during endourologic surgery were found: one
in a patient with an indwelling right ureteral DJ stent [16]
and 4 cases of duodenal perforation during percutaneous
nephrolithotomy [17].
Conclusions
Herein, we describe the first case of duodenal injury occurring during operative ureteroscopy for UTUC. The injury was due to laser ablation of the tumor in poor visibility condition on background of tissue fragility. Urologists should pay special attention when using lasers in endourology, especially during soft tissue treatment: the latest generation high-power lasers are very effective, but are also able to deliver an energy that may clearly exceed the amount needed, becoming dangerous and counterproductive, especially in case of severe bleeding. In this scenario, when controlling of the bleeding in the upper urinary tract is not achievable, always consider stopping the procedure in order to avoid life-threatening complication like this and involving interventional radiologists. Early recognition, diagnosis, and timely intervention are crucial in the management of these rare but serious complications.
Declarations
Financial Support and Sponsorship
None.
Conflicts of interest statement
G.G.: consultant for Coloplast, Rocamed, Olympus, Boston Scientific, BDBard, Cook Medical, Quanta system. S.P.: consultant for Quanta System. The other authors have no conflicts of interest to declare.
Ethical Approval and Informed consent
The patient has provided an informed consent for publication of images and information in this study.
References
1. Siegel RL, Miller KD, & Jemal A. Cancer statistics, 2019. CA Cancer J Clin, 2019, 69(1): 7-34. [Crossref]
2. Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, et al. European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol, 2021, 79(1): 62-79. [Crossref]
3. Linehan J, Schoenberg M, Seltzer E, Thacker K, & Smith AB. Complications associated with ureteroscopic management of upper tract urothelial carcinoma. Urology, 2021, 147: 87-95. [Crossref]
4. De Coninck V, Keller EX, Somani B, Giusti G, Proietti S, Rodriguez-Socarras M, et al. Complications of ureteroscopy: a complete overview. World J Urol, 2020, 38(9): 2147-2166. [Crossref]
5. Johnson GB, Portela D, & Grasso M. Advanced ureteroscopy: wireless and sheathless. J Endourol, 2006, 20(8): 552-555. [Crossref]
6. Proietti S, Marchioni M, Eisner BH, Lucianò R, Saitta G, Rodríguez-Socarrás ME, et al. Conservative treatment of upper urinary tract carcinoma in patients with imperative indications. Minerva urology and nephrology, 2021, 73(2): 245-252. [Crossref]
7. Cho SY. Current status of flexible ureteroscopy in urology. Korean J Urol, 2015, 56(10): 680-688. [Crossref]
8. Abboudi H, Ahmed K, Royle J, Khan MS, Dasgupta P, & N’Dow J. Ureteric injury: a challenging condition to diagnose and manage. Nat Rev Urol, 2013, 10(2): 108-115. [Crossref]
9. Douglawi A, Ghoreifi A, Lee R, Yip W, Seyedian SSL, Ahmadi H, et al. Bladder recurrence following diagnostic ureteroscopy in patients undergoing nephroureterectomy for upper tract urothelial cancer: is ureteral access sheath protective? Urology, 2022, 160: 142-146. [Crossref]
10. Proietti S, Rodríguez-Socarrás ME, Eisner BH, Lucianò R, Basulto Martinez MJ, Yeow Y, et al. Thulium:YAG versus holmium:YAG laser effect on upper urinary tract soft tissue: evidence from an ex vivo experimental study. J Endourol, 2021, 35(4): 544-551. [Crossref]
11. Ansari D, Torén W, Lindberg S, Pyrhönen HS, & Andersson R. Diagnosis and management of duodenal perforations: a narrative review. Scand J Gastroenterol, 2019, 54(8): 939-944. [Crossref]
12. Barkun AN, Bardou M, Kuipers EJ, Sung J, Hunt RH, Martel M, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med, 2010, 152(2): 101-113. [Crossref]
13. Karveli E, Gogoulou I, Patsaouras PA, Papamichail M, & Ioannides C. Triple tube drainage for the treatment of complex duodenal injury: a case report and literature update. Cureus, 2023, 15(6): e39995. [Crossref]
14. Watanabe G, Satou S, Tsuru M, Momiyama M, Nakajima K, Nagao A, et al. Pancreas-sparing partial duodenectomy as an alternative to emergency pancreaticoduodenectomy for a major duodenal perforation: a case report. Clin J Gastroenterol, 2023, [Crossref]
15. Kuyumcu G, Latich I, Hardman RL, Fine GC, Oklu R, & Quencer KB. Gastrodoudenal embolization: indications, technical pearls, and outcomes. J Clin Med, 2018, 7(5). [Crossref]
16. Wall I, Baradarian R, Tangorra M, Badalov N, Iswara K, Li J, et al. Spontaneous perforation of the duodenum by a migrated ureteral stent. Gastrointest Endosc, 2008, 68(6): 1236-1238. [Crossref]
17. Dahril, Oetama H, & Mustafa A. Duodenal perforation and a broken guidewire fragment inside the duodenum during supine percutaneous nephrolithotomy (PCNL) without adequate prior imaging: A case report. Urol Case Rep, 2019, 22: 25-27. [Crossref]