Open Access | Research
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Statins adherence and associated muscle symptoms in older coronary heart disease patients
* Corresponding author: Marat V. Ezhov
Mailing address: Academician Chazov street, Moscow 121552, Russia.
Email: MVEzhov@cardio.ru
Received: 01 October 2023 / Revised: 13 November 2023 / Accepted: 07 December 2023 / Published: 26 December 2023
DOI: 10.31491/APT.2023.12.125
Abstract
Background: The purpose of the study was to assess adherence to statin therapy and the incidence of statinassociated muscle symptoms in elderly patients with coronary heart disease (CHD) in a real-world clinical setting.
Methods: A cross-sectional observational study was conducted in 10 regions of Russia in clinics with the participation of 166 physicians and 959 patients with CHD aged ≥ 65 years (mean age 69 years, 47.5% women). Medical records were reviewed for medical history, blood lipid levels, and statin type and dosage. A questionnaire was applied to evaluate statin-associated muscle symptoms and reasons for refusal or termination of statin intake.
Results: Risk factors for atherosclerosis in patients were as follows: arterial hypertension–93%, obesity–59.6%, type 2 diabetes mellitus–24.6%, smoking–20.4%. Myocardial infarction and stroke were reported in 31.6% and 9.1% of patients, respectively. Statins were prescribed to 77% of patients. The main reasons for poor adherence to statin therapy were fear of adverse events (46%), lack of motivation to continue treatment (29.4%), polypharmacy (27.6%), memory impairment (26.5%) and insufficient treatment effectiveness (18.8%). Only 11.7% of patients discontinued statin intake due to side effects, whereas 13.5% of patients interrupted treatment because of cost. Muscle symptoms of mild to moderate severity occurred in 9.2% of patients; the rate of increase in serum creatine kinase was 0.83%.
Conclusion: Elderly patients with CHD have demonstrated poor adherence to statin therapy in real-world clinical settings. The incidence of statin-associated muscle symptoms was approximately 10%.
Keywords
Statins, adherence, older patients, coronary heart disease, statin-associated muscle symptoms
Introduction
Epidemiological, genetic, and randomized clinical studies have confirmed the key role of low-density lipoprotein
cholesterol (LDL-C) in the development of atherosclerotic
cardiovascular disease (ASCVD) [1-4]. Statins are the
first-line drugs for the treatment of hypercholesterolemia
and atherosclerosis [2, 3]. A large-scale meta-analysis
of the Cholesterol Treatment Trialists, which included 170,000 patients from 26 trials, showed that a 1 mmol/L reduction in plasma LDL-C was associated with a 10%
reduction in all-cause death, a 20% reduction in coronary heart disease (CHD) death, a 23% reduction in major adverse cardiovascular events, and a 17% reduction in stroke
[5]. The current treatment strategy is to use statins at the
maximum tolerated dose [2, 3]. However, in real-world
clinical practice, statins are often prescribed at inadequate doses, which lead to failure to achieve target LDL cholesterol levels in most patients.
Poor adherence to statin therapy is linked to a significantly increased risk of cardiovascular events and death [6, 7]. Reasons for non-adherence fall into three categories:
patient-related, physician-related, and health care systemrelated. Patient-related factors (skepticism, lack of symptomatic benefit, perceived or actual side effects) have a
greater impact on adherence [8].
Side effects are considered the most common reason for statin discontinuation, and statin-associated muscle symptoms (SAMS) are one of the leading causes of statin
non-adherence [9]. Observational studies and registries indicate that the incidence of SAMS can vary from 11% to
29% [9-11]. Patients may report mild to moderate muscle
pain or weakness, which is often not associated with increased creatine kinase activity [9]. Muscle symptoms are
often overlooked by clinicians and, as a result, their incidence in different patient populations is poorly defined.
More than 80% of patients who die from CHD are over 65 years of age [12]. A previous meta-analysis of 24,674
elderly patients without known ASCVD found that statins reduced the incidence of myocardial infarction by 39%
and stroke by 24% [13]. The Cholesterol Treatment Trialists meta-analysis showed a relative risk reduction of
major cardiovascular events in patients of all ages receiving statin therapy [5]. According to the 2019 European
Society of Cardiology/European Atherosclerosis Society guidelines, statin therapy in older patients should be initiated at a low dose and gradually increased up to the target
values of LDL-C, as recommended for younger patients [3].
The 2018 American College of Cardiology/American Heart Association recommendations advise limiting the
prescription of high-intensity statin regimen in patients > 75 years of age [10]. Attention should be paid to safety
issues and the risk of adverse events when prescribing statins to older patients. Older patients have comorbidities
and are taking multiple medications that increase the likelihood of side effects, including myalgia, with or without
increased creatine kinase. According to the World Health Organization, more than 50% of patients over the age of
55 develop musculoskeletal symptoms [14].
Thus, the evaluation of low statin adherence in a cohort of elderly patients is very important. This paper describes the
first large program in Russia aimed at studying statin prescription rates and adherence, related muscle symptoms,
and identification of the causes of treatment failure and poor adherence to statins in elderly patients (≥ 65 years) with CHD in a real clinical setting.
Materials and methods
This cross-sectional observational study was conducted in 10 regions of Russia in outpatient clinics involving 166 physicians and 959 patients with CHD aged ≥ 65 years
(mean age 68.9 ± 0.2 years, 47.5% women).
Inclusion criteria were as follows: age ≥ 65 years, presence of primary hyperlipidemia (Fredrickson types IIa and
IIb) and confirmed CHD. This study was conducted in accordance with the Helsinki Declaration and approved by the Institutional Review Board/Ethics Committee.
All subjects provided informed consent to participate in the study. Medical records were reviewed for medical
history, blood lipid levels, and statin type and dosage. A questionnaire was applied to evaluate statin-associated
muscle symptoms and reasons for refusal or termination of statin intake.
SAS software (version 6.12) was used for statistical analysis. For continuous variables, the mean ± standard error of
the mean was applied. Categorical parameters were presented as percentages. One-way analysis was performed
and the presence of collinearity among variables was assessed. Logistic regression was applied to calculate odds
ratios (OR). A binary logistic regression model was used to build a 95% confidence interval (CI) and a point estimate of the OR. Differences were considered statistically
significant at P < 0.05.
Results
Among the included patients, 62.7% were in the age group 65–69 years, 26.3% in the age group 70–74 years, 8.7% in the age group 75–79 years, and 2.3% in the age group ≥ 80 years (Table 1). Almost half of the participants were women; 721 patients suffered from angina pectoris. One third of the patients suffered from myocardial infarction (MI). Most patients had arterial hypertension. One fifth of the patients were current smokers. Obesity and type 2 diabetes were more common in women. Most patients were receiving antihypertensive medication and had elevated levels of LDL-C and triglycerides.
Table 1
Characteristics of patients.
| Parameters | Total cohort (n = 958) | Male (n = 503) | Female (n = 455) | Р (Male vs. Female) | Age, years | 69.8 ± 0.2 | 69.4 ± 0.2 | 70.3 ± 0.2 | 0.002 |
|---|---|---|---|---|---|
| Angina pectoris, class % | |||||
| I | 6.8 | 8.2 | 5.3 | > 0.05 | |
| II | 53.2 | 51.3 | 55.4 | > 0.05 | |
| III | 15.3 | 17.1 | 13.2 | < 0.05 | |
| IV | 2.4 | 4.4 | 0.2 | < 0.05 | |
| Myocardial infarction in the past, % | 31.6 | 40 | 22.4 | 0.001 | |
| Arterial hypertension, % | 93 | 91.5 | 94.8 | < 0.05 | |
| Stroke in the past, % | 9.1 | 7.9 | 10.3 | > 0.05 | |
| Smoking, % | 20.4 | 33.4 | 5.9 | 0.001 | |
| Obesity, % | 59.6 | 53.8 | 66.8 | 0.001 | |
| Type 2 diabetes, % | 24.6 | 19.1 | 30.8 | 0.001 | |
| Body mass index, kg/m2 | 29.4 ± 0.1 | 28.6 ± 0.2 | 30.2 ± 0.2 | 0.0001 | |
| Total cholesterol, mmol/L | 6.85 ± 0.04 | 6.77 ± 0.05 | 6.95 ± 0.06 | < 0.05 | |
| LDL cholesterol, mmol/L | 4.62 ± 0.04 | 4.52 ± 0.05 | 4.73 ± 0.06 | < 0.01 | |
| Triglycerides, mmol/L | 2.19 ± 0.03 | 2.21 ± 0.04 | 2.17 ± 0.05 | > 0.05 | |
| HDL cholesterol, mmol/L | 1.14 ± 0.01 | 1.04 ± 0.02 | 1.23 ± 0.02 | 0.0001 | |
| Glucose, mmol/L | 5.71 ± 0.04 | 5.62 ± 0.06 | 5.81 ± 0.06 | < 0.05 | |
| Creatinine, µmol/L | 90.6 ± 0.8 | 92.6 ± 1.1 | 88.1 ± 1.2 | < 0.01 | |
Note: LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Statins have been prescribed to most patients (n = 738, 77%), but only 294 (39.8%) took them regularly. The remaining patients either did not take statins at all (n = 138) or took them intermittently (n = 306). The main reasons for poor adherence to statin therapy were fear of adverse events (46%), lack of motivation (29.4%), polypharmacy (27.6%), memory impairment (26.5%), and insufficient effectiveness (18.8%) (Table 2).
Table 2
Reasons for poor adherence to statin therapy.
| Causes | Patient groups, % | Р (Male vs. Female) | ||
|---|---|---|---|---|
| Total (n = 446) | Male (n = 240) | Female (n = 204) | ||
| Fear of adverse events | 46.0 | 46.3 | 46.1 | > 0.05 |
| Lack of motivation | 29.4 | 33.3 | 25.0 | < 0.05 |
| Polypharmacy | 27.6 | 25.0 | 30.9 | < 0.05 |
| Memory impairment | 26.5 | 25.0 | 28.4 | < 0.05 |
| Insufficient effectiveness | 18.8 | 16.2 | 22.1 | < 0.05 |
| Lack of knowledge | 17.3 | 17.9 | 16.8 | > 0.05 |
| Physician's recommendation | 13.5 | 15.4 | 11.3 | > 0.05 |
| Adverse effects | 11.7 | 10.8 | 12.8 | < 0.05 |
| Drug cost | 7.6 | 8.3 | 6.9 | < 0.05 |
Other reasons were lack of knowledge about the need for continuous drug intake, recommendation by another physician, and adverse events. Only 7.6% of patients
complained about the cost of the drug.
The majority of patients (65.8%) had taken statins for 3 months, 30.1% for 4 to 12 months, and 27.3% for up to 5
years (Figure 1). Only 6.9% of patients took statins continuously for more than 5 years.
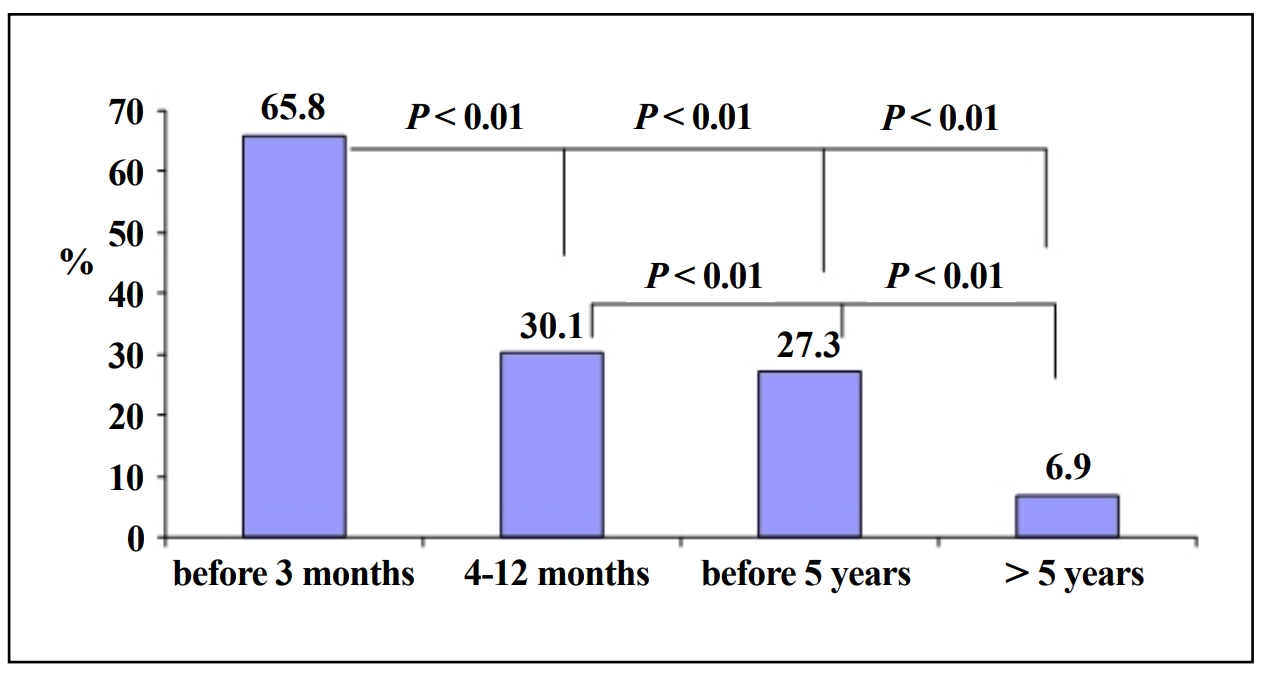
Figure 1. Duration of statin intake by older CHD patients.
Better adherence to statins was more common among women, those with a family history of CHD, previous myocardial infarction, no history of muscular symptoms, use of beta-blockers, and knowing cholesterol level (Table 3). Multivariate analysis showed that the probability of statin discontinuation markedly increased in patients with memory problems, smoking, in case of another physician's recommendation or no recommendation, due to polypharmacy, drug cost, lack of cholesterol control, and lack of and disbelief in treatment efficacy, and presence or fear of side effects (Table 4).
Table 3
Characteristics of older patients depending on duration of statin intake.
| Parameters | Duration of statin intake | Р | |
|---|---|---|---|
| < 3 months (n = 225) | > 1–5 years (n = 214) | ||
| Male | 131 (58.2) | 113 (52.3) | 0.048 |
| Higher education | 125 (57.7) | 140 (65.4) | 0.055 |
| Knowing cholesterol levels | 96 (42.7) | 131 (61.2) | 0.001 |
| Smoking | 53 (23.6) | 36 (16.8) | 0.062 |
| Family history of CHD | 122 (54.2) | 132 (61.7) | 0.006 |
| Arterial hypertension | 210 (93.3) | 202 (94.4) | 0.063 |
| Obesity | 123 (54.7) | 117 (54.7) | 0.126 |
| Type 2 diabetes | 63 (28) | 52 (24.3) | 0.077 |
| History of myocardial infarction | 84 (37.3) | 103 (48.1) | 0.001 |
| History of stroke | 15 (6.7) | 24 (11.2) | 0.056 |
| History of muscles symptoms | 20 (8.9) | 14 (6.5) | 0.015 |
| Use of beta-blockers | 126 (56) | 159 (74.3) | 0.001 |
Note: Data presented as n (%).
Table 4
Factors associated with the statin discontinuation and duration of treatment.
| Variables | OR | 95% CI | Р |
|---|---|---|---|
| Reasons for statin discontinuation | |||
| Memory impairment | 10.01 | 5.71–17.53 | 0.0001 |
| Another physician recommendation | 5.61 | 3.94–7.99 | 0.0001 |
| Absence of the physician recommendation | 5.59 | 3.74–8.37 | 0.0001 |
| Drug cost | 3.86 | 1.72–8.71 | 0.001 |
| Absence of cholesterol measurements | 3.16 | 1.98–5.06 | 0.0001 |
| Lack of treatment efficacy | 2.93 | 2.34–3.85 | 0.0001 |
| Disbelief in treatment efficacy | 2.28 | 1.45–3.59 | 0.0004 |
| Side effects | 2.04 | 1.14–3.66 | 0.017 |
| Fear of side effects | 1.68 | 1.23–2.30 | 0.001 |
| Polypharmacy | 5.14 | 3.25–8.13 | 0.0001 |
| Smoking | 1.49 | 1.06–2.09 | 0.024 |
| Factors increasing the probability of long-term statin intake | |||
| Physician recommendation | 5.53 | 3.60–8.47 | 0.0001 |
| Regular control of cholesterol level | 3.64 | 2.17–6.12 | 0.00016 |
| Knowing cholesterol level | 1.47 | 1.13–1.92 | 0.004 |
| Motivation for statins intake | 2.42 | 1.79–3.27 | 0.0001 |
| Beta-blockers intake | 2.22 | 1.67–2.94 | 0.0001 |
| Concomitant diseases | 3.45 | 1.21–9.84 | 0.020 |
| History of myocardial infarction | 1.57 | 1.19–2.05 | 0.001 |
| History of stroke | 2.04 | 1.53–2.70 | 0.001 |
| Stroke in the past | 1.63 | 1.04–2.56 | 0.032 |
Note: LDL, low-density lipoprotein; HDL, high-density lipoprotein.
Only 14.5% of elderly patients were on a high-intensity statin regimen (male 15.5%, female 9.9%), of whom 88% were treated with atorvastatin and 12% with rosuvastatin. In individuals continuously taking statins, creatine kinase levels were increased above the normal range in 0.83% (5 out of 600 patients). Mild to moderate muscle symptoms were observed in 55 (9.2%) patients, regardless of gender.
Discussion
The main finding of our study is that in real clinical practice in Russia, about 60% of elderly patients did not have
a clear understanding of the importance of constant use of statins. We included almost 1000 CHD patients ≥ 65 years
of age who were clearly eligible for statin therapy, but 23% of them had not received a statin recommendation
from their physicians. Among others, 18.7% of patients refused to take statins or 41.5% took statins intermittently. In our study, the leading reason for inconsistent
use of statins (46% of cases) was fear of adverse events, although side effects in those taking statins developed
four times less frequently than expected (only 11.7% of patients). The second most common reason for non-adherence to treatment (29% of cases) was lack of motivation
for treatment due to a lack of belief in its effect. About 27% of patients reported memory impairment, which was
also a major barrier to chronic statin use. Polypharmacy was another reason for treatment discontinuation. Women
were more likely to experience side effects, leading to higher rates of treatment discontinuation. This provided
better control of LDL-C levels in men compared to women, although men had less faith in the ability of statins to
prolong their lifespan. Poor control of cholesterol levels, despite taking the drug, was the reason for refusal to take
statins in every fifth patient. Adherence to statin treatment increased significantly when target LDL-C levels were
achieved. The most important evidence base is that high adherence to statins provides a significant reduction (59%)
in cardiovascular risk in patients with target LDL cholesterol levels [15]. It is well known that polypharmacy, co-morbidity,
the presence of multiple risk factors, and high LDL-C levels at baseline at any age significantly reduce
adherence to statin therapy. [16, 17]. Only a persuasive,
convincing, and detailed explanation of the necessity of
taking lipid-lowering drugs for cardiovascular risk reduction can increase adherence of older patients to the therapy. A large observational study of 19,518 subjects older
than 65 years had shown that all-cause mortality rate was 34% lower and cardiovascular disease events were 20%
fewer among those who had adhered to statin treatment for primary prevention [18]. In 542 hospitalized patients
with angiographically confirmed CAD with a mean age of 69 years from an area with the highest CAD mortality
rate, only 85% of patients were receiving statins at discharge, with a further decline in statin adherence of 15.7%
at 12 months of follow-up [19]. Similarly, in a large study
of 62,070 patients (mean age 66 years, 65% male), statin therapy was associated with 25% relative reduction of
3-year risk of major cardiovascular events (P < 0.0001) [20]. In a study of 347,104 patients with ASCVD, it was
found that the lower the adherence to statin therapy, the higher the risk of all-cause mortality [21].
The USAGE (Understanding Statin Use in America and Gaps in Education) Internet survey assessed the behavior
of 10,138 US adults who were former or current statin users. Muscle symptoms were reported by 60% and 25% of
former and current users, respectively [22]. The primary
reasons for switching from one statin to another were cost (32%) and SAMS (33%), whereas the primary reason for
discontinuation was side effects (62%). Lack of efficacy was mentioned only 13% of respondents [23]. Nearly half
of the participants switched a statin at least once [22]. In our study, we assessed the reasons for discontinuation, but
not for switching statins. Also, the USAGE survey demonstrated that females were more likely to have discontinued
statin intake than males [24], whereas we found no differences in statin discontinuation between women and men.
Importantly, the larger ACTION (Adherence and concerns with statins and medication discussions with physicians)
survey confirmed the main findings of USAGE [25].
Gender differences in treatment adherence may be due to biological or social reasons. Women are less likely than men to believe that statins are safe and effective. Women
perceive themselves to be at low risk of fatal cardiovascular events [26, 27].
Adherence is typically measured as a single fixed average over the entire follow-up period, but should be considered
over time and across behaviors. A retrospective cohort study that controlled for time-dependent factors influencing prior adherence and the temporal sequence between
factors found that adherence to statins in women reduced
the risk of cardiovascular events by approximately onefifth compared with non-adherence [28]. Thus, adherence
is a complex behavior that requires training, motivation, and lifestyle changes. Other factors, such as socioeconomic status, also play a role. In previous studies, adherence
to statin treatment was lower in women than in men [29].
There are no studies on gender differences in adherence to statins in the Russian population. The lack of gender
differences in adherence in our study may be countryspecific.
Our study reveals two important trends in current statin therapy. First, the cost of statins is not a limiting factor for
their use in clinical practice. Second, the number of side
effects with statins was much lower than expected. Elevations in creatine kinase levels associated with statins occurred in less than 1% of patients, while mild to moderate
muscle symptoms were observed in 9.2% of patients. The PRIMO (Prediction of muscle risk in observation) study
conducted in France in patients with hyperlipidemia (30% aged ≥ 65 years) treated with high-dose statins showed
that the incidence of mild to moderate muscle symptoms was 10.5% [11]. In our study, only 14.5% of participants
received high-intensity statin therapy, and overall, statinrelated muscle symptoms (including asymptomatic creatine kinase elevations) were observed in 10% of
participants. Moreover, we showed that statin therapy in older
patients was administered for the first 3 months, after which adherence to treatment sharply decreased. Prescribing statins to older patients would likely be justified
by a balanced approach based on the benefits of statins with the lowest risk of adverse events. It is assumed that
proper treatment of an elderly patient requires mutual understanding and agreement between the patient and the
physician [22]. Ensuring the quality of life of an elderly
patient is an important issue in terms of medical care. We need to expand and improve outpatient care for this group
of patients, avoiding polypharmacy as much as possible and providing medications based on expected benefits and
potential risk of complications.
Our study has several limitations. First, physicians involved in the study retrospectively analyzed medical
records and questionnaires filled by patients. Second, we cannot exclude the possibility that some patients may
have provided inaccurate information about their attitudes toward statin treatment due to cognitive problems. However, our study provides novel and valuable information
on statin adherence in elderly patients in a real-world setting.
Conclusions
Elderly patients with CHD in real-world clinical settings in Russia demonstrated poor adherence to statin therapy, and the incidence of statin-associated muscle symptoms was about 10%.
Declarations
Acknowledgments
The authors thank Alexander D. Deev for statistical analysis.
Conflicts of interest
Authors declare no conflict of interests.
Financial support and sponsorship
National Medical Research Center of Therapy and Preventive Medicine, Ministry of Health of the Russian Federation.
Ethical approval
This study was conducted in accordance with the Helsinki Declaration and approved by the Institutional Review Board/Ethics Committee.
References
1. Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European atherosclerosis society consensus panel. Eur Heart J, 2017, 38(32): 2459-2472. [Crossref]
2. Jacobson TA, Ito MK, Maki KC, Orringer CE, Bays HE, Jones PH, et al. National lipid association recommendations for patient-centered management of dyslipidemia: part 1--full report. J Clin Lipidol, 2015, 9(2): 129-169. [Crossref]
3. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J, 2020, 41(1): 111-188. [Crossref]
4. Holmes MV, Asselbergs FW, Palmer TM, Drenos F, Lanktree MB, Nelson CP, et al. Mendelian randomization of blood lipids for coronary heart disease. Eur Heart J, 2015, 36(9): 539-550. [Crossref]
5. Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet, 2010, 376(9753): 1670-1681. [Crossref]
6. Mazhar F, Hjemdahl P, Clase CM, Johnell K, Jernberg T, Sjölander A, et al. Intensity of and adherence to lipidlowering therapy as predictors of major adverse cardiovascular outcomes in patients with coronary heart disease. J Am Heart Assoc, 2022, 11(14): e025813. [Crossref]
7. Phan DQ, Duan L, Lam B, Hekimian A, Wee D, Zadegan R, et al. Statin adherence and mortality in patients aged 80 years and older after acute myocardial infarction. J Am Geriatr Soc, 2019, 67(10): 2045-2049. [Crossref]
8. Lansberg P, Lee A, Lee ZV, Subramaniam K, & Setia S. Nonadherence to statins: individualized intervention strategies outside the pill box. Vasc Health Risk Manag, 2018, 14: 91-102. [Crossref]
9. Stroes ES, Thompson PD, Corsini A, Vladutiu GD, Raal FJ, Ray KK, et al. Statin-associated muscle symptoms: impact on statin therapy-European atherosclerosis society consensus panel statement on assessment, aetiology and management. Eur Heart J, 2015, 36(17): 1012-1022. [Crossref]
10. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. J Am Coll Cardiol, 2019, 73(24): e285-e350. [Crossref]
11. Bruckert E, Hayem G, Dejager S, Yau C, & Bégaud B. Mild to moderate muscular symptoms with high-dosage statin therapy in hyperlipidemic patients--the PRIMO study. Cardiovasc Drugs Ther, 2005, 19(6): 403-414. [Crossref]
12. Rosengren A. Better treatment and improved prognosis in elderly patients with AMI: but do registers tell the whole truth? Eur Heart J, 2012, 33(5): 562-563. [Crossref]
13. Savarese G, Gotto AM, Jr., Paolillo S, D’Amore C, Losco T, Musella F, et al. Benefits of statins in elderly subjects without established cardiovascular disease: a metaanalysis. J Am Coll Cardiol, 2013, 62(22): 2090-2099. [Crossref]
14. Briggs AM, Cross MJ, Hoy DG, Sànchez-Riera L, Blyth FM, Woolf AD, et al. Musculoskeletal health conditions represent a global threat to healthy aging: a report for the 2015 world health organization world report on ageing and health. Gerontologist, 2016, 56 Suppl 2: S243-255. [Crossref]
15. Wei L, MacDonald TM, Watson AD, & Murphy MJ. Effectiveness of two statin prescribing strategies with respect to adherence and cardiovascular outcomes: observational study. Pharmacoepidemiol Drug Saf, 2007, 16(4): 385- 392. [Crossref]
16. Perreault S, Blais L, Dragomir A, Bouchard MH, Lalonde L, Laurier C, et al. Persistence and determinants of statin therapy among middle-aged patients free of cardiovascular disease. Eur J Clin Pharmacol, 2005, 61(9): 667- 674. [Crossref]
17. Ofori-Asenso R, Jakhu A, Curtis AJ, Zomer E, Gambhir M, Jaana Korhonen M, et al. A systematic review and metaanalysis of the factors associated with nonadherence and discontinuation of statins among people aged ≥65 years. J Gerontol A Biol Sci Med Sci, 2018, 73(6): 798-805. [Crossref]
18. Eilat-Tsanani S, Mor E, & Schonmann Y. Statin use over 65 years of age and all-cause mortality: a 10-year followup of 19 518 people. J Am Geriatr Soc, 2019, 67(10): 2038-2044. [Crossref]
19. Waßmuth S, Rohe K, Noack F, Noutsias M, Treede H, & Schlitt A. Adherence to lipid-lowering therapy In patients with coronary heart disease from The state of Saxony-Anhalt, Germany. Vasc Health Risk Manag, 2019, 15: 477-483. [Crossref]
20. Anderson JL, Knowlton KU, May HT, Bair TL, Armstrong SO, Lappé DL, et al. Temporal changes in statin prescription and intensity at discharge and impact on outcomes in patients with newly diagnosed atherosclerotic cardiovascular disease-real-world experience within a large integrated health care system: the IMPRES study. J Clin Lipidol, 2018, 12(4): 1008-1018.e1001. [Crossref]
21. Rodriguez F, Maron DJ, Knowles JW, Virani SS, Lin S, & Heidenreich PA. Association of statin adherence with mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol, 2019, 4(3): 206-213. [Crossref]
22. Cohen JD, Brinton EA, Ito MK, & Jacobson TA. Understanding statin use in America and gaps in patient education (USAGE): an internet-based survey of 10,138 current and former statin users. J Clin Lipidol, 2012, 6(3): 208-215. [Crossref]
23. Wei MY, Ito MK, Cohen JD, Brinton EA, & Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol, 2013, 7(5): 472-483. [Crossref]
24. Karalis DG, Wild RA, Maki KC, Gaskins R, Jacobson TA, Sponseller CA, et al. Gender differences in side effects and attitudes regarding statin use in the understanding statin use in America and gaps in patient education (USAGE) study. J Clin Lipidol, 2016, 10(4): 833-841. [Crossref]
25. Brinton EA. Understanding patient adherence and concerns with statins and medication discussions with physicians (ACTION): a survey on the patient perspective of dialogue with healthcare providers regarding statin therapy. Clin Cardiol, 2018, 41(6): 710-720. [Crossref]
26. Nanna MG, Wang TY, Xiang Q, Goldberg AC, Robinson JG, Roger VL, et al. Sex differences in the use of statins in community practice. Circ Cardiovasc Qual Outcomes, 2019, 12(8): e005562. [Crossref]
27. Venditti V, Bleve E, Morano S, & Filardi T. Gender-related factors in medication adherence for metabolic and cardiovascular health. Metabolites, 2023, 13(10): 1087- 1093. [Crossref]
28. Lavikainen P, Helin-Salmivaara A, Eerola M, Fang G, Hartikainen J, Huupponen R, et al. Statin adherence and risk of acute cardiovascular events among women: a cohort study accounting for time-dependent confounding affected by previous adherence. BMJ Open, 2016, 6(6): e011306. [Crossref]
29. Bots SH, Inia JA, & Peters SAE. Medication adherence after acute coronary syndrome in women compared with men: a systematic review and meta-analysis. Front Glob Womens Health, 2021, 2: 637398. [Crossref]