Open Access | Case report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Interventional Therapy of Late Onset Tracheal Stenosis After Implantation of 125Iodine Seed Esophageal Stent
*Corresponding author: Yong-Zhen Wang
Mailing address: Department of Interventional Radiology and
Vascular Surgery, Nanjing Second Hospital, Nanjing University of
Chinese medicine, No. 1 Zhongfu Road, Gulou District, Nanjing,
Jiangsu 210003, China.
E-mail: yongzhenw@163.com
Received: 12 Jan 2019 Accepted: 15 March 2019
DOI: 10.31491/CSRC.2019.03.028
Abstract
This study reported a case of late-staged esophageal carcinoma, complicated by severe dyspha late onset tracheal stenosis after treating with 125Iodine seed stent implantation. The patient had progressive stenosis of the lower segment (left main trachea) at 6, 26, and 47 days postoperatively. The cause of stenosis might be related to direct press by stent, tumor proliferation, the aortic arch with violate pulsate and the complications caused by other therapies. Due to its short clinical utilization, 125Iodine seed stent may present some fatal complications. Therefore, the long-term efficacy of 125Iodine seed stent remains to be studied.
Keywords
125Iodine seed; esophagus stent; late onset; tracheal stenosis; complication
Introduction
Self-expandable metal stent has been extended to apply to advanced and late-staged esophageal cancer, with the safety and therapeutic efficiency of stent loaded with 125Iodine seeds confirmed [1,2]. The occurrence and condition of complication resemble the conventional stent, however, the late onset tracheal stenosis has been rarely reported. This paper reviewed 1 case of late-staged esophageal carcinoma, complicated with late onset tracheal stenosis and severe dysphagia, which had been treated with 125Iodine seed stent implantation.
Cases
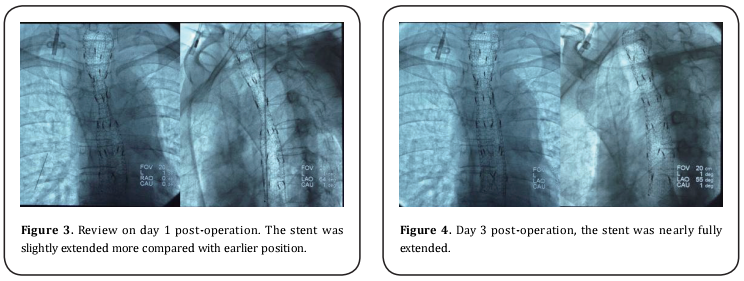
Female patient, 64 years old. She was diagnosed as esophageal carcinoma in February, 2008. Pathology test categorized as squamous carcinoma (Fig. 1). In operation, it was found that tumor tissue adhered extendedly with intra-meditational main vascular, caused the unreality to remove and application of alternative of radiotherapy (64 Gy/32f in total) combined with 4 periods of adjuvant chemotherapy (TP formula: Docetaxel + Nedaplatin). The tumor shrunk and symptoms alleviated temporally, till the dysphagia reoccurred and aggravated at the beginning of June, 2009. The patient then can only be fed with fluid. Combinatorial testing with barium swallows and tracheogram, gastroscopy and CT, it was diagnosed as “esophageal carcinoma stage III, severe esophageal stenosis and Stooler stage 3”. The patient was implanted with 125Iodine seed stent on August 1st, 2009. The stent was membrane-bundled knitting type, of upper cup, size: 20 mm X 10 cm, produced by Nanjing Weichuang Medical Technology Co., Ltd., Nanjing, China; 125Iodine seeds, 0.8mci X 24, produced by Xinke Pharmaceutical Co., Ltd., Shanghai, China. The implantation operation performed smoothly, and hardened lesion and severe stenosis were observed during operation. Post-implantation radiography image indicated the proper stent placing, but with poor stretch. The narrowest section measures as approximately 8 mm (Fig. 2).
Discussion
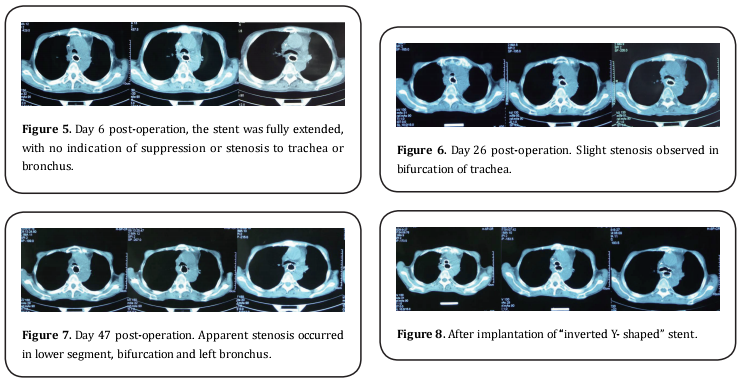
The radioactive element seed stent was created first
by Chinese doctors, which have been applied in clinic
successfully for decades. The late onset of tracheal stenosis has been rarely reported [1-4]. The CT images taken
on day 6, 26 and 47 post-operation shown progressive
stenosis of lower segment (left main trachea). The 125Iodine seed is composed of normal membrane-bundled
knitting stent, seeds storehouse weaved with alloyed silk
thread and radioactive particles. The possible causes for the late onset tracheal stenosis were analyzed as follows:
1. Direct press by stent: it is often resulted from using
over-sized stent or the pressure impacted by “cup” or
“ball” on either end of the stent to the posterior wall of
the trachea and/or bronchus. Such complication usually
released around 1 week after the operation, which can be
explained as opening of the cup or fully extension of the
stent. Such spatial change can cause pressure to trachea
and the posterior wall of bronchus. However, this case
cannot be explained by this cause.
2. Tumor proliferation: Continuously growing tumor or
lymph node of metastasis directly invades into or suppresses on bronchus. However, the following check by CT
confirmed that the tumor shrunk other than expanded
after stent implantation, which excludes this cause as
well.
3. The aortic arch with violating pulsate, with implantation period increasing, generally affected the tracheal
blood circulation, leading to denaturation, putrescence,
and cartilage ring collapse, characterized by its late onset.
4. Complications caused by other therapies, especially
the radiotherapy (including the external radiotherapy
and radioactive particle internal radiotherapy). The accumulating ray may result in tracheomalacia, bronchus
collapse, and subsequent stenosis.
Trachea pressure is a severe and lethal complication,
which usually occurs after stent implantation for middle
esophageal carcinoma of early stage [5-8]. It is frequently caused by mechanical pressure caused by the stent,
with position of occurrence consists with the case in this
report.
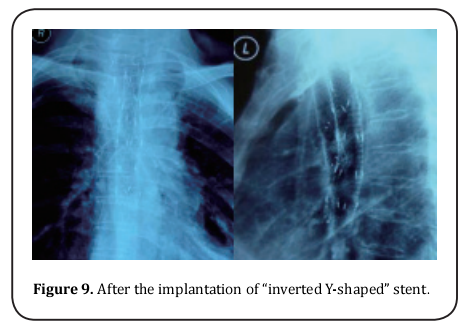
For this reported patient, it was reported of significant
collapse on anterior wall of left lower segment of and
left main bronchus, approximately the same place of the
aortic arch. This position was faced with violate pulsate
of the aortic arch and backed against with solid metal
stent. Due to the previous radiotherapy against esophageal carcinoma, the accumulated ray effect may have
lead to potential trachea damage, which may be worsen
by long term continuous exposure to 125Iodine seed carried by the stent. The cumulative effect of these factors
eventually resulted in the tracheomalacia, trachea collapse, and subsequent stenosis. Judged by the position
of pathological changes and detailed condition, it was
speculated that performing trachea or bronchus stent
implantation would alleviate the symptoms of patients.
Besides, the complication occurs in the lower segment
of left main bronchus, which indicated that “Y-shaped”
stent would relieve the stenosis [7,8].
The 125Iodine seed stent implantation method, accepted by clinical physicians, exerts radiotherapy to tumor
internally produces better anti-tumor effect for the patients with late stage esophageal carcinoma, to raise
living standards and prolong survival time. However,
its relatively short period of clinical application may involuntary hides some rare but lethal complications from
both patients and medical personnel. In summary, the
long term effect of 125Iodine seed stent remains to be
studied.
References
1. Guo, J. H., Teng, G. J., Zhu, G. Y., He, S. C., Fang, W., Deng,
G., and Li, G. Z. (2008) Self-expandable esophageal stent
loaded with 125I seeds: initial experience in patients with
advanced esophageal cancer. Radiology 247, 574-581
2. Wang, Z. M., Hang, X. B., Cao, J., Hang, G., Chen, K. M., Liu,
Y., and Liu, F. J. (2012) Intraluminal radioactive stent
compared with covered stent alone for the treatment
of malignant esophageal stricture. Cardiovasc Intervent
Radiol 35, 351-358
3. Zhu, H. D., and Guo, J. H. (2011) Esophageal stent
implantation for the treatment of esophageal strictures:its
current situation and research progress. Journal of
Interventional Radiology 20, 494-498
4. Wang, Y. Z., Wang, Y. H., Liu, R. B., He, D. F., and Liu, Y. (2009)
Clinical Application of Irradiation Stents in Esophageal
and Cardiac Cancer. China Modern Doctor 03, 29-30
5. Sharma, P., Kozarek, R., Practice Parameters Committee of
American College of, G. (2010) Role of esophageal stents in benign and malignant diseases. Am J Gastroenterol 105,
258-273
6. Kujawski, K., Stasiak, M., and Rysz, J. (2012) The evaluation
of esophageal stenting complications in palliative
treatment of dysphagia related to esophageal cancer. Med
Sci Monit 18, CR323-329
7. Han, X. W., Gang, W. U., Gao, X. M., Nan, M. A., and Wang,
Y. L. (2005) The clinical practice of inserting two stents
in esophagus and trachea. Journal of Interventional
Radiology 02, 163-166
8. Lin, A. J., Guo, Q. Y., Liu, Z. Y., and Lu, Z. M. (2010) Double
stents indwelling in malignant tracheal and esophageal
stenosis. Biomedical Engineering Clinical Medicine 03,
240-244