Open Access | Case Report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
The rare patient with infrainguinal stent restenosis a complication: Atherectomy device fracture
Corresponding author: Metin Onur BEYAZ
Mailing address: : Departmant of Cardiovascular Surgery, Tayfur
Ata Sokmen Faculty of Medicine, Hatay Mustafa Kemal University, Hatay, Turkey.
E-mail: metinonurbeyaz@gmail.com
Received: 22 March 2021 / Accepted: 24 January 2022
DOI: 10.31491/CSRC.2022.03.086
Abstract
Excisional atherectomy alone or followed by balloon angioplasty in patients with infra-inguinal peripheral artery disease is an acceptable and appropriate treatment strategy. In this article, a case study of a 67-year-old man who had an intravascular foreign body removed due to an aterectomy device fracture while performing atherectomy due to peripheral arterial disease in the Cardiovascular Surgery Unit of our hospital is presented. The foreign body was demonstrated by a digital subtraction angiography examination. Access to the superficial femoral artery was made by an incision on the anterior 1/3 of the right thigh, and the broken atherectomy part was excised. Surgical intervention may be required to remove the intravascular foreign body that is broken during peripheral artery atherectomy.
Keywords
Peripheral artery disease; atherectomy; foreign body
Introduction
Peripheral artery disease (PAH) is a clinical condition
that has been increasing in recent years. Although it
has various clinical variations for itself, the majority
of patients suffer from claudication which affects their
lifestyle [1]. In addition to the medical and surgical approach, angiographic treatment methods, especially
infrainguinal atherectomy, and additional balloon angioplasty have been widely used [2]. Cilostazol which
has clearly proven efficacy in medical treatment can’t
be used in patients with left ventricular failure. That
is why we use endovascular methods like angioplasty,
atherectomy, or a combination of these in patients with
infra-inguinal peripheral artery disease [3]. Performing
angioplasty to the superficial femoral artery (SFA) isgenerally an inadequate treatment. It is characterized
by a high degree of calcification of the SFA and the
widespread involvement of the disease and a much
higher prevalence of occlusion than stenosis [4]. There
are a number of atherectomy devices for SFA disease
including rotational atherectomy, orbital atherectomy,
and excisional. There is no comparison has been made
between available atherectomy devices in randomized
studies [5]. There is no clear signal of superiority among
these treatment modalities in observational studies.
Thus, the choice of device is left to the experience and
expertise of the surgeon.
We present a case of a 67-year-old male, who was previously treated with an infrainguinal stent in an external center. The stent was totally cluded and we were
planned to treat using excisional atherectomy and balloon angioplasty.
In this case, the blood vessel was occluded within
3 months following stenting. It is unique in that the
atherectomy catheter is broken in the patient scheduled for atherectomy treatment.
In this case report, the mechanism and management of
the complication are discussed
Case Report
A 67-year-old male patient was admitted to our clinic
with the complaint of right calf claudication, which has
been progressive for the last 4 weeks and restricted his
lifestyle. There was no history of ischemic rest pain or
non-healing wounds. On the right, he had an ABI (Anke
Brachial Index) of 0.6.
His past medical history was remarkable in terms of
coronary artery disease, tobacco use, and femoropopliteal bypass above the knee with PTFE graft to the same
extremity and peripheral artery stenting below the
inguinal ligament. Diagnostic angiography showed extensive right iliac artery disease, total occlusion in the
common femoral artery and right SFA, and old nitinol
stents totally occluded in both the common femoral
artery (CFA) and distal of the SFA. After consultation
with the patient, it was decided to continue endovascular treatment of the right external iliac, CFA, and SFA.
The left common femoral artery access is done without any complications. A long angiographic sheet was
placed into the left iliac artery and it was advanced
in a retrograde way until it reached the external right
iliac artery. Lesions in the external iliac and femoral
arteries were crossed with a 0.18 mm nitinol wire. We
advanced it with the wire of the atherectomy device.
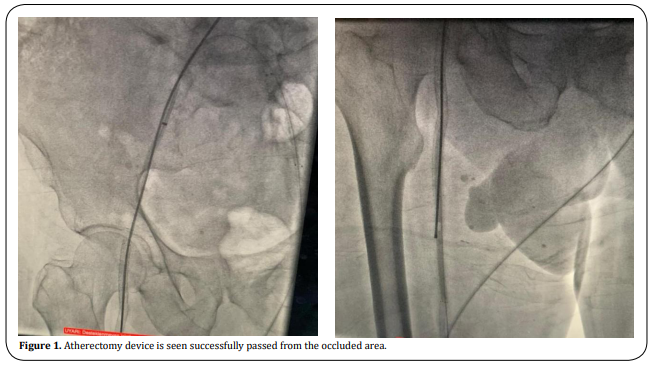
Occlusions within the common femoral artery and
distally to the external iliac artery were successfully
passed with atherectomy (Figure 1). When the distal
of the SFA was reached, the atherectomy catheter was
broken in the old nitinol stent, which was understood
to be subintimal after the procedure.
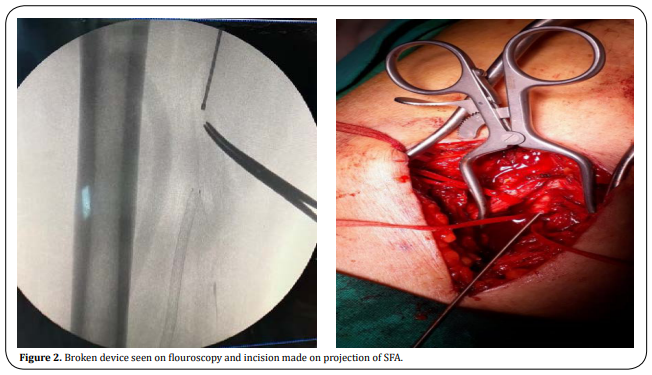
The patient was operated under general anesthesia
under emergency conditions. Under fluoroscopy, the
tip of the atherectomy catheter was found and marked.
The skin was passed subcutaneously, SFA was found
and returned. Transverse arteriotomy was performed
after 1 cc heparinization. The broken end of the atherectomy device (18 cm) was grasped with forceps
and taken out. Proximal and distal embolectomy was
performed. Inflow and run-off current was seen. The
artery was primarily repaired with 0.6 prolene. (Figure
2).
Discussion
There are other potential complications of atherectomy, but the fracture is rare. There are studies in the
literature in which the guide wires were broken independently of atherectomy [6]. The most unique feature
of our case is that it did not contain the total occlusion
of the old nitinol stents before atherectomy, and unfortunately, the old stent placed by another hospital was
positioned out of the lumen.
Contact between the incisor of the atherectomy device
and the subintimal stent might be among the factors
that contributed to this complication, because of loss of
structural strength. Various methods have been reported for retrieving broken devices using techniques suchas catheter use, biopsy forceps, and balloon inflation [7].
In our case, the use of a trap atherectomy catheter was
not appropriate because the severed piece was quite
long (18 cm). In addition, it was thought that the pressure balloon inflation technique was not applicable
due to the risk of rupture of the vessel wall by the very
hard foreign body. Although the guidewire technique
is theoretically possible to retrieve the split end, the
capture guidewires will not always be entangled. With
endovascular methods and the use of infra-inguinal
stents, there is a success rate above 95%. However,
because of the nitinol stent structure, the risk of subintimal placement, and the movements of the limbs,
the chance of success decreases to 50% [8]. Because of
these risks, atherectomy and balloon angioplasty are
thought to be more appropriate in stents in the infra
inguinal artery [9].
Conclusion
The use of atherectomy should be reconsidered in cases with infrainguinal stent implantation due to the subintimal location of the SFA stent and the risk of more risky complications of the atherectomy device.
Declarations
Authors’ contributions
Made substantial contributions to conception and design of the study and performed data analysis and interpretation: Beyaz MO, Sadikoglu Lale B, Kaya S; Performed data acquisition, as well as provided administrative, technical, and material support: Oruc D, Hakkoymaz S, Urfalı S.
Availability of data and materials
All data of the patients are stored at Hatay Mustafa Kemal University where the operations are performed.
Conflicts of interest
The authors declared that there are no conflicts of interest to disclose
Ethical approval and consent to participate
We studied in accordance with the ethical guidelines set by the Helsinki Declaration and the International Association of Heart and Lung Transplantation (ISHLT). A retrospective study was made by obtaining signed documents and approvals from all patients for procedures, including the approval of the use of patient data in future retrospective studies.
References
1. Campia, U., Gerhard-Herman, M., Piazza, G., & Goldhaber, S. Z. (2019). Peripheral Artery Disease: Past, Present, and Future. American Journal of Medicine, 132(10), 1133-1141.
2. Firnhaber, J. M., & Powell, C. S. (2019). Lower Extremity Peripheral Artery Disease: Diagnosis and Treatment. American Family Physician, 99(6), 362-369.
3. Tsigkou, V., Siasos, G., Rovos, K., Tripyla, N., & Tousoulis, D. (2018). Peripheral artery disease and antiplatelet treatment. Current Opinion in Pharmacology, 39, 43-52.
4. Tang, Q. H., Chen, J., Hu, C. F., & Zhang, X. L. (2020). Comparison Between Endovascular and Open Surgery for the Treatment of Peripheral Artery Diseases: A Meta-Analysis. Annals of Vascular Surgery, 62, 484-495.
5. Safian, R. D., Niazi, K., Runyon, J. P., Dulas, D., Weinstock, B., Ramaiah, V., & Heuser, R. (2009). Orbital atherectomy for infrapopliteal disease: device concept and outcome data for the OASIS trial. Catheterization and Cardiovascular Interventions, 73(3), 406-412.
6. Tsujimura, T., Ishihara, T., Iida, O., Asai, M., Masuda, M., Okamoto, S., ... & Mano, T. (2019). Successful percutaneous retrieval of a detached microcatheter tip using the guide-extension catheter trapping technique: A case report. Journal of Cardiology Cases, 20(5), 168-171.
7. Gallagher, K. A., Meltzer, A. J., Ravin, R. A., Graham, A., Shrikhande, G., Connolly, P. H., ... & McKinsey, J. F. (2011). Endovascular management as first therapy for chronic total occlusion of the lower extremity
arteries: comparison of balloon angioplasty, stenting, and directional atherectomy. Journal of Endovascular Therapy, 18(5), 624-637.
8. Schillinger, M., Sabeti, S., Dick, P., Amighi, J., Mlekusch, W., Schlager, O., ... & Minar, E. (2007). Sustained benefit at 2 years of primary femoropopliteal stenting compared with balloon angioplasty with optional stenting. Circulation, 115(21), 2745-
2749.
9. Clegg, S., Aghel, A., & Rogers, R. K. (2014). Late presenting, contained rupture of the superficial femoral artery following atherectomy and stenting: case report and literature review. Catheterization and Cardiovascular Interventions, 84(2), 257-261.