Open Access | Research Article
This work is licensed under a
Creative Commons Attribution-ShareAlike 4.0
International License.
Predictors of relaparotomy for persisting intra abdominal infection in secondary peritonitis
# These two authors contribute equally to the work as co-first authors.
* Corresponding author: Abel Shiferaw Tesfaye
Mailing address: Department of Surgery, Addis Ababa
University, college of health science, school of Medicine, Yeka Sub city, Addis Ababa, Ethiopia.
Phone
number: 0913921385
Email: abelshiferaw3417@gmail.com
Received: 24 June 2021 / Accepted: 19 July 2021
DOI:
10.31491/CSRC.2021.09.082
Abstract
Background: Peritonitis is one of the commonest causes of acute abdomen in Ethiopia. One of the causes
of high morbidity and mortality is persistent intraabdominal infection. The two essential approaches for
managing post-op collection are laparotomy on-demand and planned Relaparotomy. Despite multiple studies, both
have comparative mortality. This study aimed to identify clinical variables that are predictive of persistent
intraabdominal infection.
Methods: A retrospective study was conducted on patients who were operated on from Sept 2018 to April
2020 at two affiliated referral hospitals of AAU, college of Medicine; Yekatit 12 hospital Medical College and
Minilik II referral Hospital. All of the patients were cases of secondary peritonitis. Clinical progress of
the patients from admission to discharge/death was documented. Multiple preoperative and intraoperative
variables were analyzed to develop the predictive clinical model.
Results: Out of 172 laparotomy cases for secondary peritonitis, 40 (23.3%) required relaparotomy for
postop collection. From Patients who developed postop collection, 45% of them were diagnosed after pus/Gi
content leaked through the surgical wound. The mortality rate of patients who develop postop collection and
undergone relaparotomy was 27.5 % and 4.5% for those without postop collection. Logistic regression identified
4 variables as having significant predictive value: Duration of illness more than 5 days, Systolic BP 1000 ml, and small bowel as a source of contamination. Overall prediction
successes of the above model is 88.4% (sensitivity 53.3%, specificity 96.8%).
Conclusion: Management of persistent intra-abdominal infection is challenging. We have identified 4
clinical variables that predict persistent intraabdominal infection requiring relaparotomy. These sets of
variables can be a milestone for future validation study before being inserted in today to day clinical
practice.
Keywords
Relaparotomy, Predictors, Laparotomy, Secondary peritonitis, Intra-abdominal infection
Introduction
Peritonitis is one of the commonest causes of acute abdomen with a high mortality rate ranging from 10-60%
depending on the study in western countries [1] and it is one of the commonest causes of acute
abdomen in
Ethiopia [2-6]. Secondary Peritonitis accounts for approximately 90% of all peritonitis cases in
western
countries [7, 8].
Irrespective of the cause, successful management of peritonitis includes early
administration of antibiotics, timely and effective surgical intervention, and supportive care to maintain organ
function and limit the development of multiple organ failure [9-11]. One of the main causes of death
is failure
to control the initial infection and persistence of bacterial peritonitis. To minimize these risks, the concept
of “relaparotomy” was introduced.
Incidence of relaparotomy ranges from 0.5 -15% in various reported
studies [12-14]. The studies suggest early intervention reduces mortality by decreasing multi-organ
failure
[15].
Despite the development of antibiotics and significant improvement in intensive care
support,
mortality after relaparotomy ranges from 24 to 71 % [12, 13, 16].
The two essential approaches
for managing
post-op collection are RL on-demand (“wait and see” approach) and planned RL [17]. Planned
relaparotomy detects
persistent infection early, before the occurrence of MODS; while high negative relaparotomy is the drawback. In
On-demand relaparotomy, exploration is limited to patients who developed signs and symptoms of persistent
intraabdominal infection. The disadvantage of this strategy is the late detection of the postop collection after
SIRS develops.
Both strategies have advantages and disadvantages and are still used side-by-side in
clinical practice despite growing support for on-demand strategy. The studies conducted in the past few years do
not seem to suggest that either approach confers a superior advantage in terms of mortality
[18-21].
A
meta-analysis conducted by Lamme et al. in 2002 comparing planned vs on-demand relaparotomy strategies showed
in-hospital mortality was 0.70 (95 % confidence interval 0.27 to 1.80) in favor of the on-demand strategy, but
it was not statistically significant [18].
Rakic et al analyzing the outcomes of 65 patients
with severe
peritonitis and concluded although planned laparotomy seemed to have a lower mortality rate, there was no
significant difference after adjustments [19].
In 2004 Lamme et al conducted a retrospective
study on 278
patients with secondary peritonitis and found a significantly lower hospital mortality rate for on-demand
laparotomy (21.8% vs. 36%; p = 0.016) and a better two-year survival rate (65.8% vs. 55.5%; p = 0.031)
[20].
The only Randomized clinical trial was conducted by van Ruller et al. in 7 teaching hospitals in
the
Netherlands including a total of 232 patients [21]. The study showed death and major morbidity, were
similar in
the two groups at 12 months (mortality 29% on-demand and 36% planned; p = 0.23; morbidity 40% on-demand and 44%
planned; p = 0.58). However, there were significant differences in the secondary outcomes, with the on-demand
group having significantly shorter ICU stays (7 vs. 11 days), fewer hospital days (27 vs 35), and lower cost
(23% less).
As already mentioned both strategies have comparable mortality, but there is still ongoing
researches being done to find out some specifications that help to address specific strategies, specifically
planned relaparotomy. But in the end, all concluded rather than specifying a single strategy, they prefer to
give extra care and attention to patients with specific factors to have a low clinical threshold for early
relaparotomy in these patients.
The objective of this study was to identify preoperative and intraoperative
clinical factors that may predict ongoing abdominal infection and the need for relaparotomy to construct a
clinical model to assist clinicians in predicting the need for relaparotomy in patients with persisting
intraabdominal infection in secondary peritonitis.
There are very little data on this specific problem from
the developing world, where the spectrum of disease is markedly different from that in the developed world
[21-27].
Materials and Methods
Study design
A retrospective cross-sectional quantitative design was used to conduct the study, with an analytical approach adopted to determine the predictors of relaparotomy for persistent intraabdominal infection.
Study Setting
This study was conducted in the two affiliated referral hospitals of AAU, college of Medicine, Addis Ababa. These hospitals are Yekatit 12 teaching hospital and Minilik II referral Hospital. The surgical departments of these hospitals are the training sites for surgical residents of the postgraduate program of the College of Health Science, AAU.
Study population
A total of 172 consecutive patients with secondary peritonitis who had undergone laparotomy from Sept 1, 2019, to April 08, 2020, were included in this study.
Inclusion criteria
All patients admitted and operated for secondary peritonitis in the department in the two affiliated hospitals of AAU, college of Medicine within this time frame were included.
Exclusion criteria
Patient with initial laparotomy done in other hospitals
Patients with negative laparotomy
Patients with acute pancreatitis
Patients with mesenteric Ischemia
Patient with already planned relaparotomy
Patient with TB peritonitis
A patient who has undergone a relaparotomy for other causes (bleeding, wound dehiscence…)
Patients with peritonitis following trauma
Source of data
Patients’ medical chart was main source data. Basic demographic data (age, sex, place of referral) were
collected. The clinical symptoms, findings on physical examination, post-resuscitation vital signs, and
laboratory results were recorded. Intraoperative details were extracted from the operation note.
Additional
information was extracted from the emergency room triage paper, operation logbook, and HMIS.
Data were collected using a structured questionnaire and it was collected by the primary investigator.
Statistical analysis
The patients were divided into two groups, the relaparotomy, and the non-relaparotomy group. More than 20 preop
and intraop factors were evaluated concerning their significance in predicting the need for relaparotomy for
postop collection.
Student’s t-test for continuous variables and the chi-squared test for nominal variables
were run to identify any significant differences between the two groups. Logistic multiple regression was then
performed using all factors found significant on this univariate analysis. Those variables with a p-value less
than 0.05 were considered significant and were inserted in the predictive model.
All data analysis was
performed using IBM SPSS Statistics (version 23).
Ethical Consideration
Ethical clearance for the study was obtained from Addis Ababa University, College of Health Science Institutional Review Board. Data collection was undertaken after permission is obtained from the administration. The identities of the study participants will not be disclosed. The collected questionnaires were not transferred to a third party.
Operational definitions
1. Relaparotomy: - Abdominal operations that have to be redone within 60 days in association with the initial
surgery
Positive findings - turbid or purulent intra-abdominal fluid with/out Gi content.
Negative findings - minimal amounts of serous fluid with no other new findings in the abdomen.
2. Referred from any rural center:- being referred from outside of Addis Ababa.
3. Antibiotic intake before Surgery:- any antibiotic taken(PO or IV) for more than 24 hr with an intention of
treatment, before surgery.
4. Localized Peritonitis:- peritoneal inflammation localized to a specific quadrant.
5. Generalized peritonitis:- inflammation involving all or most of the peritoneal surface.
6. Previous abdominal surgery:- any open abdominal surgery that breaches the peritoneum.
Results
During the study period, 172 eligible cases were admitted and operated on for secondary peritonitis in the two
hospitals. 102 patients were operated on at Minilik II hospital and 70 patients were operated on at Yekatit
hospital.
Out of 172 patients, 70.9% of the patients were males and 29.1% were females. The Median age
group of patients was 25 yrs, with 53.5 % of them lie between 15 yrs and 34 yrs. 82% of patients were referred
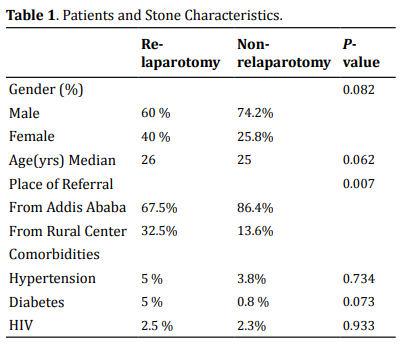
from Addis Ababa, while 18% were from outside of Addis Ababa (Table 1). The commonest comorbid disease that was
found was hypertension (4.1%), followed by HIV (2.3%) and DM (1.7%).
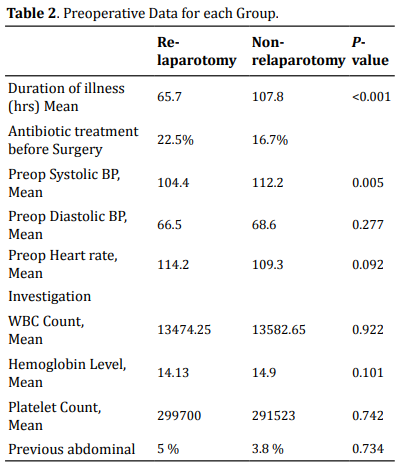
The median length of time from the onset of symptoms to seeking medical care was 3 days. In our study, 93% of our patients fall into ASA 1 and 2 scores. In physical examination, the median systolic BP was 110 and diastolic BP was 70. The median pulse rate was 110. Information about preoperative factors is also summarized in (Table 2).
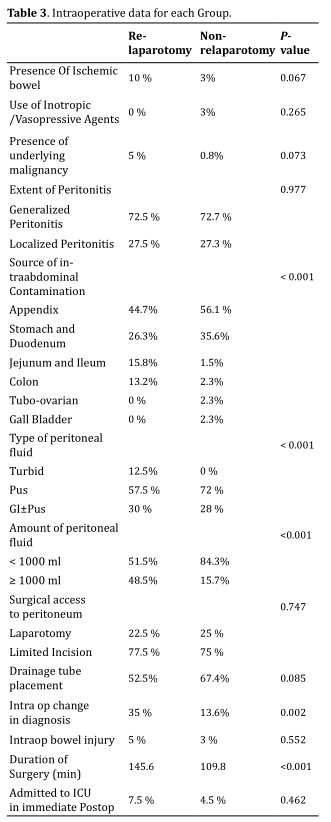
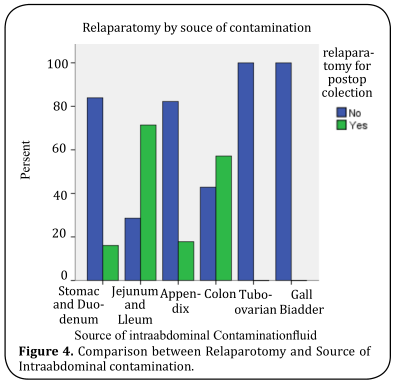
Of all cases of peritonitis, 72.7 cases had generalized peritonitis, while 27.3% had localized peritonitis. To
access the peritoneum, a limited incision was used in 24.4% of patients, while full laparotomy was used in 75.6%
of patients. While assessing the intraop factors, the most common cause of secondary peritonitis was complicated
appendicitis (52.9%), followed by perforated PUD (33.1%), small bowel pathology (4.7 %), and colonic pathology
(4.7%). During exploration, pus was found 68.8 % of the time, while GI content mixed with pus was found 28.5% of
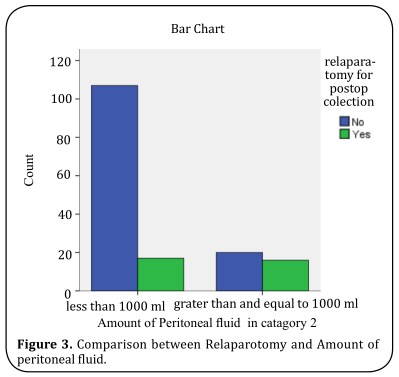
the time. The mean amount of peritoneal fluid was 673.4 ml, more than 1000ml of peritoneal fluid was found in
22.5 % of patients.
During exploration, ischemic bowel and underlying malignancy were found in 4.7 % and
1.7% of patients respectively. A drainage tube was left in 64 % of patients after exploration. Intraoperatively,
inotropes and/or vasopressors were required in 2.3% of patients. Intraop bowel injury was observed in 3.5% of
cases. In 18.6% of cases, the diagnosis was changed after exploration and intraop finding. 4.1% of patients had
previous abdominal surgery. The median duration of surgery was 110 min. All intraoperative data are shown in
(Table 3).
Out of 172 laparotomy cases for secondary peritonitis, 40 (23.3%) required relaparotomy for postop collection.
From Patients who developed postop collection, 45% of them were diagnosed after pus/Gi content leaked through
the surgical wound, while the rest were diagnosed with clinical signs augmented with imaging. Of the 40 patients
who developed postop collection, 33 (82.5%) of them only require 1 relaparotomy, 6 (15%) of them underdone 2
relaparotomy, and 1 (2.5%) was reoperated 3 times.
The median duration between laparotomy for peritonitis
and first relaparotomy for the postop collection was 7.5 days, with 30% of the cases, is beyond 10 days. The
mean duration of hospital stay for all peritonitis cases with no postop collection was 7 days, while those with
postop collection requiring relaparotomy were 21.9 days. In Our study, the mortality rate of patients who
develop postop collection and undergone relaparotomy was 27.5 % and 4.5% for those without postop
collection.
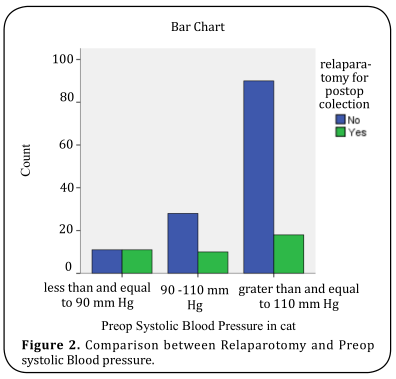
Based on the differences between the relaparotomy and nonrelaparotomy groups, several
parameters were found to be significant on Chi-square and student-t correlation tests. These variables were
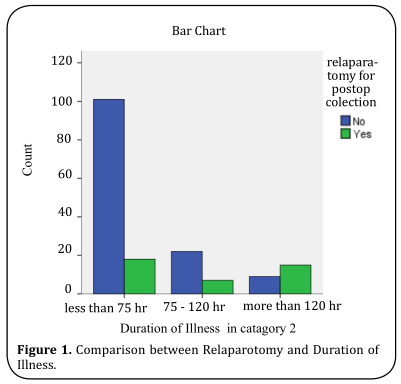
included in a logistic regression model to predict the need for relaparotomy. Duration of illness more than 5
days, Systolic BP 1000 ml, and small bowel as a source of contamination
was found to be significant on logistic regression (Figure 1-4). Overall prediction successes of the above model
are 88.4% (sensitivity 53.3%, specificity 96.8%), less than 75 hr.
Discussion
In Developing countries like ours, peritonitis is one of the causes of the acute abdomen that is associated with
high mortality and morbidity.
In this study, appendicitis was the commonest cause of peritonitis, which is
consistent with most studies in Ethiopia [2, 3, 5, 6] and Western countries [28]. The
overall mortality of
patients with secondary peritonitis is reported to be between 12% and 79% [19, 28-32], while in our
study, it is
9.9%. In our study, the incidence of relaparotomy for the postop collection was 23.3 %, which is in a higher
range than most western literature (0.5 -15%) [11, 12]. The mortality we observed after relaparotomy
was 27.8%,
comparable to most studies (24 to 71 %) [12, 13, 16].
The median interval to relaparotomy was 8
days (3 – 58 days) in our studies, which is more than most studies(Hutchins et al. – 5 days) [15]. The median
duration of hospital stay in our study was 21 days, which was comparable to a Randomized study done in the Netherlands in
teaching hospitals (27 days).
We have identified 4 independent predictors of subsequent relaparotomy with
multivariate analysis: Duration of illness > 5 days, Systolic BP <= 90 mmHg, Source of cont. (small bowel) and
amount of peritoneal fluid.
A systemic review done by lamme showed age, concomitant disease, upper
gastrointestinal source of peritonitis, generalized peritonitis, elimination of the focus, bilirubin,
creatinine, lactate, PaO2/FiO2 ratio, and albumin showed significant association [33].
Another study done
in Lithuania by A. Sileikis showed age, CRP, MPI, and duration of surgery as independent predictors for positive
relaparotomy [11]. In our study duration of surgery showed correlation on univariate analysis, but
not in
logistic regression. We did not include CRP and MPI b/c retrospective nature of our study.
A study done in
Houston, Texas by Jerry J. Kim, showed peripheral vascular disease, alcohol abuse, BMI of 29 kg/m2 or higher,
the finding of any ischemic bowel at initial laparotomy, and OR latency of 60 hours or longer were good
predictors of relaparotomy [34]. In our study, we could not include peripheral vascular disease and
BMI as
variables b/c of the retrospective nature of our study, while the presence of ischemic bowel did not show a
correlation.
A South African study done by V Y Kong, on complicated appendicitis found referral from a
rural center; duration of illness >5 days; heart rate >120 bpm; and perforation with associated GC as an
independent predictor [35]. When comparing to our study, duration of illness was also a strong
predictor, while
the place of referral had shown correlation on chi-square test, but did not show significant correlation on
logistic regression.
From all the above-mentioned studies, we can observe there is no universal model for
all; it depends on disease pattern, population distribution, and available resources. As we can see, 45% of our
patients were diagnosed after infectious fluid has leaked through the surgical wound. This signifies signs and
symptoms of persistent infection were subtle enough to be missed. So we can use this model to find patients who
are at increased risk of post-op collection requiring relaparotomy and intervene early before MODS occurs.
This study has some limitations. The retrospective nature of the study is the main one. A prospective study would
have given us a chance to analyze more variables and make a follow-up of patients complete. A smaller sample
size makes the generalizability of the study limited. Further prospective validation studies are required before
the widespread adoption of this predictive model in clinical practice.
Conclusion
Prevention is the best strategy in the management of persistent intrabdominal infection. The first surgery in
peritonitis must be complete to prevent post-op collection. To achieve this, early administration of
antibiotics; timely and effective surgical intervention, and Supportive are paramount. Despite the maximum
effort, some patients develop a persistent intraabdominal infection. The two main approaches to deal with postop
intraabdominal infection are planned and on-demand relaparotomy. Multiple studies have been done to confirm
whether planned or on-demand relaparotomy is superior, but still, none of them show significant differences in
mortality [28-30, 35]. These are partly because of a lack of standardized criteria to define when to
perform a
relaparotomy during disease.
The variables found in our study can be used as one of the criteria to find
patients at increased risk of post-op collection, so we can plan a relaparotomy or work up the patients to
detect persistent intraabdominal infection before the development of SIRS. This will decrease negative
relaparotomy while detecting persistent infection early before the development of MODS. The low sensitivity of
the model requires further studies before the widespread use of our predictive model.
Declarations
Authors’ contributions
Abel Shiferaw: Conceived the project, carried out to acquisition and analysis of data, contributed to drafting and approval of
the final manuscript
Henock
T/Selase: Made substantial contributions to conception and design of the study and provided technical support
Availability of Data and Material
The patients’ data were collected using Hard copy questionnaires that are available as a compiled file. The Data entered into SPSS version 23 is available and will be sent when requested by the review committee
Financial Support and Sponsorship
Financial support for this article is from Addis Ababa University, College of Health Science. The funding is for covering material costs during the conduction of the study.
Ethical Approval and Informed consent
Ethical clearance for the study was obtained from Addis Ababa University, College of Health Science Institutional Review Board.
Conflict of interest
All authors declared that there are no conflicts of interest
References
1.Farthmann, E. H., & Schöffel, U. (1990). Principles and limitations of operative management of intraabdominal
infections. World Journal of Surgery, 14(2), 210-217.
2.Wossen, M. T., editor Pattern of Emergency Surgical Operations Performed for Non-Traumatic Acute Abdomen at
Ayder Referral Hospital, Mekelle University, Tigrai, Ethiopia by the Year 2000-2003 Ec2019. 9(5), 4.
3.Gebrie, T. Management Outcome and Associated Factors of Surgically Treated Non Traumatic Acute Abdomen at
Attat
Hospital, Gurage Zone, Ethiopia. International Journal of Surgery Research and Practice.
4.Pawulos, W. (2017). Assessment of Non-Traumatic Acute Abdominal Cases Treated Operatively at Wolaita Sodo
Teaching and Referral Hospital, Southern Ethiopia. Assessment, 14.
5.Ayenew, Z., Gizaw, A., Workneh, D., & Fentahun, N. (2016). Outcome of non-traumatic surgical acute abdomen in
nekemte referral hospital southwest Ethiopia: a retrospective cross-sectional study. Surgery Current Research,
7(282), 1-5.
6.Berhane, Y., Girmay, K., & Gebresilassie, A. (2016). Outcome of emergency surgical operations performed for
non-traumatic acute abdomen among adults in Mekellehospital. European Journal of Pharmacology Medical Research,
3(14), 106-111.
7.Kujath, P., Rodloff, A. ( 2005). Peritonitis. ed Second edition Bremen, London, Boston, UNIMED,
36-41.
8.Gupta, S., & Kaushik, R. (2006). Peritonitis - the Eastern experience. World Journal of Emergency Surgery, 1,
13.
9.Malangoni, M. A., & Inui, T. (2006). Peritonitis - the Western experience. World Journal of Emergency Surgery,
1, 25.
10.Mandell, K., & Arbabi, S. (2010). Re-laparotomy for severe intra-abdominal infections. Surgical Infections,
11(3), 307-310.
11.Sileikis, A., Kazanavicius, D., Skrebunas, A., Ostapenko, A., & Strupas, K. (2013). Prediction for a planned
relaparotomy in secondary peritonitis. Central European Journal of Medicine, 8(4), 410-414.
12.Unalp, H. R., Kamer, E., Kar, H., Bal, A., Peskersoy, M., & Onal, M. A. (2006). Urgent abdominal
re-explorations. World Journal of Emergency Surgery, 1(1), 1-6.
13.Koirala, R., Mehta, N., Varma, V., Kapoor, S., Kumaran, V., & Nundy, S. (2015). Urgent Redo-Laparotomies:
Patterns and Outcome—A Single Centre Experience. Indian Journal of Surgery, 77(3), 195-199.
14.Agalar, F., Eroglu, E., Bulbul, M., Agalar, C., Tarhan, O. R., & Sari, M. (2005). Staged abdominal repair for
treatment of moderate to severe secondary peritonitis. World Journal of Surgery, 29(2), 240-244.
15.Hutchins, R. R., Gunning, M. P., Lucas, D. N., Allen-Mersh, T. G., & Soni, N. C. (2004). Relaparotomy for
suspected intraperitoneal sepsis after abdominal surgery. World Journal of Surgery, 28(2), 137-141.
16.Krivitskiĭ, D., Shuliarenko, V., & Babin, I. (1990). Indications for relaparotomy. Klinicheskaia khirurgiia,
(1), 18-21.
17.Mayberry, J. C., Goldman, R. K., Mullins, R. J., Brand, D. M., Crass, R. A., & Trunkey, D. D. (1999).
Surveyed
opinion of American trauma surgeons on the prevention of the abdominal compartment syndrome. Journal of Trauma
and Acute Care Surgery, 47(3), 509-514.
18.Lamme, B., Boermeester, M., Reitsma, J., Mahler, C., Obertop, H., & Gouma, D. (2002). Meta-analysis of
relaparotomy for secondary peritonitis. Journal of British Surgery, 89(12), 1516-1524.
19.Lojpur, B. A., Williams, B. A., & Sprung, J. (2005). Comparison of on-demand vs planned relaparotomy for
treatment of severe intra-abdominal infections. Croation Medical Journal, 46(6), 957-963.
20.Lamme, B., Boermeester, M., Belt, E., Van Till, J., Gouma, D., & Obertop, H. (2004). Mortality and morbidity
of
planned relaparotomy versus relaparotomy on demand for secondary peritonitis. Journal of British Surgery, 91(8),
1046-1054.
21.van Ruler, O., Mahler, C. W., Boer, K. R., Reuland, E. A., Gooszen, H. G., Opmeer, B. C., ... & Steller, E.
P.
(2007). Comparison of on-demand vs planned relaparotomy strategy in patients with severe peritonitis: a
randomized trial. Jama, 298(8), 865-872.
22.Kong, V. Y., Bulajic, B., Allorto, N. L., Handley, J., & Clarke, D. L. (2012). Acute appendicitis in a
developing country. World Journal of Surgery, 36(9), 2068-2073.
23.Kong, V., Aldous, C., Handley, J., & Clarke, D. (2013). The cost effectiveness of early management of acute
appendicitis underlies the importance of curative surgical services to a primary healthcare programme. The
Annals of The Royal College of Surgeons of England, 95(4), 280-284.
24.Kong, V. Y., Van de Linde, S., Aldous, C., Handley, J. J., & Clarke, D. L. (2013). Quantifying the disparity
in
outcome between urban and rural patients with acute appendicitis in South Africa. South African Medical Journal,
103(10), 742-745.
25.Kong, V. Y., Aldous, C., & Clarke, D. L. (2014). Understanding the reasons for delay to definitive surgical
care
of patients with acute appendicitis in rural South Africa: general surgery. South African journal of surgery,
52(1), 2-5.
26.Kong, V. Y., Van Der Linde, S., Aldous, C., Handley, J. J., & Clarke, D. L. (2014). The accuracy of the
Alvarado
score in predicting acute appendicitis in the black South African population needs to be validated. Canadian
Journal of Surgery, 57(4), E121.
27.Clarke, D., Thomson, S., Bissetty, T., Madiba, T., Buccimazza, I., & Anderson, F. (2007). A single surgical
unit’s experience with abdominal tuberculosis in the HIV/AIDS era. World Journal of Surgery, 31(5),
1088-1097.
28.Merlino, J. I., Malangoni, M. A., Smith, C. M., & Lange, R. L. (2001). Prospective randomized trials affect
the
outcomes of intraabdominal infection. Annals Of Surgery, 233(6), 859.
29.Christou, N. V., Barie, P. S., Dellinger, E. P., Waymack, J. P., & Stone, H. H. (1993). Surgical Infection
Society intra-abdominal infection study: prospective evaluation of management techniques and outcome. Archives
of Surgery, 128(2), 193-199.
30.Koperna, T., & Schulz, F. (1996). Prognosis and treatment of peritonitis: do we need new scoring systems?
Archives of Surgery, 131(2), 180-186.
31.Wittmann, D. H., Schein, M., & Condon, R. E. (1996). Management of secondary peritonitis. Annals Of Surgery,
224(1), 10.
32.Mulier, S., Penninckx, F., Verwaest, C., Filez, L., Aerts, R., Fieuws, S., & Lauwers, P. (2003). Factors
affecting mortality in generalized postoperative peritonitis: multivariate analysis in 96 patients. World
Journal of Surgery, 27(4), 379-384.
33.Lamme, B., Mahler, C. W., van Ruler, O., Gouma, D. J., Reitsma, J. B., & Boermeester, M. A. (2006). Clinical
predictors of ongoing infection in secondary peritonitis: systematic review. World Journal of Surgery, 30(12),
2170-2181.
34.Kim, J. J., Liang, M. K., Subramanian, A., Balentine, C. J., Sansgiry, S., & Awad, S. S. (2011). Predictors
of
relaparotomy after nontrauma emergency general surgery with initial fascial closure. The American journal of
surgery, 202(5), 549-552.
35.Kong, V. Y., van der Linde, S., Aldous, C., Handley, J. J., & Clarke, D. L. (2014). Developing a clinical
model
to predict the need for relaparotomy in severe intra-abdominal sepsis secondary to complicated appendicitis.
South African journal of surgery, 52(4), 91-95.