Open Access | Research Article
This work is licensed under a
Creative Commons Attribution-ShareAlike 4.0 International License.
A perspective of extremity vascular trauma epidemiology and its management in a resource limited set up
# These three authors contribute equally to the work as
co-first authors
* Correspondence author: Dawit Gebregiorgis
Mailing
address: Department of Surgery, School of Medicine,College of Health
Science, Addis Ababa University, Addis Ababa, Ethiopia.
E-mail: dawit.gebregiorgis@aau.edu.et
Received: 13 May 2021 / Accepted: 24 August 2021
DOI:
10.31491/CSRC.2021.09.080
Abstract
Background: Extremity vascular injuries are one of the major
causes of limb loss and potentially preventable deaths after trauma.
Although it is a major challenge, especially in countries with a less
established trauma center, early diagnosis, and intervention are
important for a better outcome. The aim of this study was to describe
the epidemiology, management strategies, and outcomes of extremity
vascular trauma in the Ethiopian setting.
Methods: A retrospective observational study was conducted
among all extremity vascular trauma patients who were admitted and
treated at Tikur Anbessa Specialized Hospital (TASH) Between June 2015
and May 2020.
Results: A total of 85 patients with extremity vascular trauma,
predominantly male (90.6%), were included in the study. The mean age
was 27 ± 9 years. Penetrating trauma caused 89.4% of extremity
vascular injuries. The majority of the injuries are caused by
stab/sharp (40%), bullet (29.4%) and road traffic accidents (17.7%).
The brachial artery was the commonest vessel injured accounting for
36.5% followed by femoral artery injury of (22.4%). The commonest
types of vascular injuries were complete transection (74.1%),
laceration (15.3%), and partial transection (8.2%). The most commonly
used method of vascular reconstruction was reverse interposition
venous graft accounting for 45.9%. Other methods were ligation &
hemostasis (20%), primary repair with End-to-End Anastomosis (17.7%),
primary simple repair (15.3%), and venous patch (1.2%). A limb salvage
rate of 91.8% was achieved despite a 67.1% of late presentation (>6
hours).
Conclusion: Vascular injuries are mainly due to violence and
road traffic accidents. Limb loss and mortality due to this injury can
be mitigated by improving health policies, implementing emergency
ambulatory systems, and provision of vascular services with better
training centers.
Keywords
Trauma, vascular injury, epidemiology, vascular reconstruction, outcome
Introduction
Trauma is one of the leading worldwide health problems that cause an
estimate of more than 5.8 million people to die each year (10% of the
world’s total death) [1, 2]. Though vascular injury
accounts for only 1-2% of the total injury, hemorrhages resulting
fromthe injury are a major cause of potentially preventable deaths
[3-6]. Although uncommon following civiliantrauma,
vascular injuries may be responsible for upto 20% of trauma deaths
[7] and the highest utilization of hospital
resources [3, 4, 8]. Vascular injuries to
theextremity are common accounting for up to half of allvascular
injuries, and it is the third leading cause ofpotentially survivable
injury [5, 9-11].
Extremity vascular trauma
patients tend to be predominantly male and mainly occur in the younger
population with average ages in the 30’s
[3, 4, 10]. Extremity vascular injury can result
from both blunt and penetrating mechanisms. Those with blunt vascular
injury to the extremity have a higher rate of mortality (2-5%) than
penetrating trauma mainly due to associated non-vascular injuries in the
blunt trauma. The amputation rate is also higher in blunt extremity
vascular injuries [4, 12].
In Ethiopia, injury
is a major cause of mortality with an estimated rate of 12% and
extremity injury resulting in fracture and/or dislocation is the
commonest one [13, 14]. Studies have also shown a
higher incidence of amputation in trauma patients with comminuted
fractures associated with vascular injury [15-17].
In Ethiopia, a literature review showed very limited studies done on
vascular trauma. The aim of this study was to describe the extremity
vascular trauma experience of a tertiary hospital (TASH) in Ethiopia in
terms of epidemiology, management strategy, and outcome.
Materials and methods
Tikur Anbessa specialized hospital (TASH) is an 800-bed tertiary
referral hospital that offers diagnosis & treatment for approximately
500,000 patients a year. The hospital gives specialized clinical
services including vascular surgery for patients referred from the whole
country. The hospital is equipped with 14 operating theaters; one is
dedicated to vascular surgery. Recently, the center has also acquired a
new bi-plane and a monoplane cardiac catheterization laboratory that can
also serve peripheral vascular disease.
A retrospective
cross-sectional study was conducted on patients with extremity vascular
trauma between June 2015 and May 2020. All patients who were diagnosed
and treated for extremity vascular trauma with a named blood vessel
injury were included in the study. While those patients with an injury
to the named blood vessel proximal to the junctional zone (central
injury), proximal to the axillary artery (upper extremity), proximal to
the common femoral artery (lower extremity), and non-extremity
peripheral vascular injuries were excluded.
Records were reviewed
to examine demographic, anthropometric, residence, occupation, duration,
type, site, mechanism, and any other associated injuries. A clinical,
laboratory, radiological, echocardiographic, operative data, type of
repair, perioperative complications, hospital stay, and other covariates
like other morbidity and mortality were collected using a structured
data abstraction format prepared for this study. Data were collected
through self-administered a structured questionnaire from an existing
HMIS logbook, registry book, and patients chart at TASH. During data
collection, the principal investigator did supervise all activities
during the data collection. Data completeness and consistency were
checked on spot questionnaires, and missed variables were turned back
for correction. Data was then cleaned manually for consistency, for any
missing values, and finally entered into SPSS Version 23.0 for analysis.
Descriptive analysis was performed using SPSS version 23.0 to describe
the study variables. Frequency analysis was run for socio-demographic,
clinical diagnosis, and management outcomes. Finally, the findigs were
described in the text, percent, and means, and presented using frequency
tables and charts.
Ethical clearance was granted from Institutional
Review Board; Collage of Health Science Addis Ababa University. A letter
of permission to retrieve a medical record of needed patients from an
archive was then obtained from Tikur Anbessa Specialized Hospital. Every
aspect of human rights, which includes the right to privacy and
confidentiality, was maintained throughout the study and measures were
taken to maintain anonymity by not including patients’ names in the
questionnaire.
Results
A total of 85 patients with extremity vascular trauma who attended and were treated at the TASH surgical department and who met the eligibility criteria were enrolled in the study. Extremity vascular trauma accounts for 62% of the total vascular injuries attended during the five-year study period.
Socio-demographic & economic characteristic
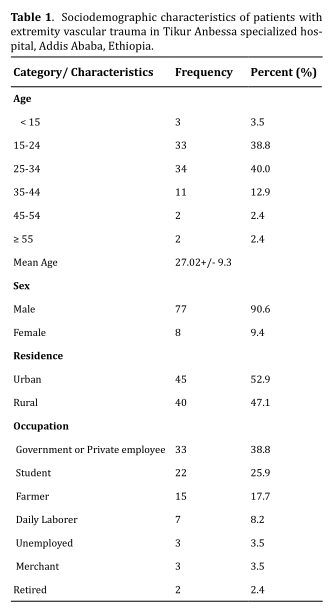
Among the total of 85 extremity vascular trauma patients, 77 (90.6%) were males while the remaining 8 (9.4%) were females. The ratio of males to females was 9.6:1. The median age (IQR) was 26 years with the range being from 13 to 60 years. Most of the cases (78.8%) were between the age group of 15 to 35 years. Urban residents accounted for 45 (52.9%) and 40 (47.1%) were from a rural area of the country. In this study, majority of the patients were either government or private sector employee 33 (38.8%) and students 22 (25.9%). Additionally, farmers constitute 15 (17.7%) and daily laborers 7 (8.2%) (Table 1).
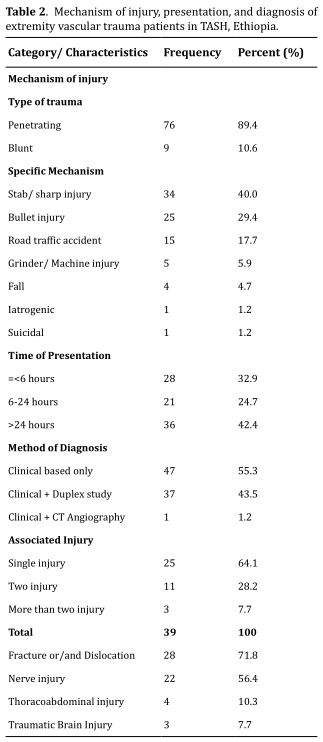
Clinical presentation, mechanism of Injury and Diagnosis
As shown in Table 2 majority of the patients 57 (67.1%) presented after 6
hours of injury. Penetrating trauma accounted for 89.4% of the cases;
which is significantly higher than blunt trauma (10.6%). Unintentional
injuries were the primary causes 43 (50.6%) of extremity vascular trauma
and intentional injuries which have a relatively equal proportion;
resulted in 42 (49.4%) of vascular trauma. Stab (or Sharp) injuries
34 (40.0%) were the commonest causes of extremity vascular trauma, which
was followed by Bullet injury 25 (29.4%). Other causes include road
traffic accident 15 (17.7%), grinder or machine injury 5 (5.9%), fall
4 (4.7%), iatrogenic 1 (1.2%), and suicidal 1 (1.2%).
Diagnosis of
extremity vascular trauma was made clinically in 55.3% of patients , and
in the remaining cases Doppler Ultrasound 37 (43.5%) and Computed
Tomography Angiography 1 (1.2%) were supplemented. There was an
associated injury apart from the vascular injury in 39 (45.9%) of cases
with 14 (35.9%) of them having more than one (Table 2). The commonest
associated injury was bone fracture (with or without dislocation), which
accounted for 28 (71.8%); followed by peripheral nerve injury 22 (56.4%).
Median nerve injury was seen in 10 (45.5%) cases and is the commonest
peripheral nerve injured.
Anatomical distribution and type of vascular injury
Vascular injuries to the upper and lower extremities were found to be
proportionally distributed with 54.1% and 45.9%, respectively. The
arterial injury was identified in 80 (94.1%) cases and there was a
concomitant venous injury to it in 42 (52.5%). An isolated venous injury
was found in 5 (5.9%) cases.
The commonest type of arterial vascular
injury was brachial artery 31 (38.8%) and femoral artery injury was the
second common arterial injury with 19(23.8%). The most dominant type of
vascular injury was complete transection with 63 (74.1%) followed by
laceration 13 (15.3%), partial transection 7 (8.2%), wall defect 1 (1.2%),
and contusion 1 (1.2%) which could be with or without thrombosis (Table
3).
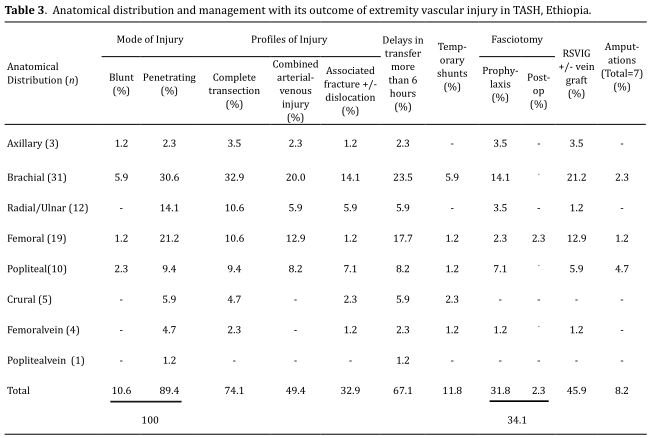
Management and outcome
Upon arrival (on referral) to TASH; eighteen (21.2%) patients had been
operated on at forwarding locations and ten (11.8%) patients came after
a temporary shunt was applied to the injured vessels & eight (9.4%)
patients had a ligated vessels for hemostatic purpose. Since patients
who had a shunt were not heparinized and traveled a long distance before
reaching the tertiary hospital, they were all found to be non-patent.
The material used was an intravenous set plastic tube and was applied to
five patients with brachial artery injury and one for each injury to the
superficial femoral artery, popliteal artery, posterior tibial artery,
anterior tibial artery and femoral vein.
Open surgical techniques
were employed for all cases. As illustrated in Table 3 the method used
for vascular reconstruction mainly was reverse interposition venous
graft (commonly GSV) in 39 (45.9%); followed by ligation 17 (20%), primary
end to end anastomosis 15 (17.7%), and primary repair 13 (15.3%); in which
fogarty thrombectomy was coupled for those with thrombosis. The venous
patch was done for one patient (1.2%) with a wall defect and for the
patient with vascular contusion who had a thrombosis an arteriotomy then
thrombectomy was done. Fasciotomy was done in 29 (34.1%); as prophylaxis
in 27 (93.1%), and post-operatively for compartment syndrome in 2 (6.9%).
The type of anesthesia used was generral anesthesia in 66 (77.6%), spinal
anesthesia in 10 (11.8%), and block in 9 (10.6%) from which 2 (2.3%) were
converted to GA.
Surgical wound infection was the commonest postop
complication with 32 (37.6%), followed by palsy 17 (20%), graft failure or
occlusion 9 (10.6%), sepsis 2 (2.4%) and bleeding 1 (1.2%). Graft occlusion
occurred early within the first 30 days, despite early surgical
intervention the amputation rate was 7 (8.2%). The early patency rate was
59 (69.4%). After a median follow-up period of 9 months (range, 3-24),
long-term results showed a patency rate of 71.8% with preservation of
limb function in 55 (64.7%). The disability rate was 30 (35.3%), which was
due to palsy/weakness 18 (60%), amputated limb 7 (23.3%), and wound
contracture 5 (16.7%). No patients expired and all were discharged home.
The median length of hospital stay was 9 days, with the range of 2 to
102 days.
Discussion
Vascular trauma, especially to the extremity is a common health care
problem in our setup, and prompt diagnosis and management of this injury
are mandatory to reduce the risk of ischemic limb loss and hemorrhages
threatening the life of the patient. An epidemiological approach to the
characterization of many health care problems that have been applied so
far showed a significant benefit. Even though an epidemiologic approach
to a civilian extremity vascular trauma has a benefit, it has not been
applied extensively in most of the world [18]. This study
serves as a baseline to the current and future trends of the
epidemiology and management outcome of extremity vascular trauma in our
institution(TASH).
Vascular trauma to the extremity predominantly
occurs in males than females with the range of 70 to 95% [4, 19-22] Our
study also shows a male predominance of 90.6%. Trauma in general is more
common in the younger age group; accounts for the majority of mortality
in the younger population of the USA [1]. Perkins ZB, et al. [4]. Murad
M, et al. [23], and Sah B, et al. [22]; all showed a higher incidence of
vascular trauma in the younger, 30s and 40s age group. The median age in
our study was 26 years with a 78.8% occurrence of extremity vascular
trauma between the age group of 15 to 35 years. The study also has shown
that it mainly affects the working force of the population. A Nigerian
study by Adeoye, et al. [20]. also showed a younger age group
predominance in civilian vascular trauma.
Extremity civilian trauma
from both blunt and penetrating mechanisms is common. Despite having a
difference in the pattern & mechanism of injury based on the age group,
according to Konstantinidis A, et al. [24]. extremity trauma accounts
for 1.6% of the total civilian trauma. Though blunt trauma has a higher
risk of limb loss and mortality because of the high impact forces
causing extensive damage to the soft tissue, bones, and nerves;
penetrating trauma tends to result in a higher rate of extremity
vascular injuries to the long tracked vessels [12, 25]. Penetrating
trauma accounts for 89.4% of extremity vascular injury in the current
study. The commonest mechanisms of injury were found to be due to
homicidal or interpersonal violence, which is stab or sharp injury (40%)
and bullet injury (29.4%) followed by road traffic injury (17.7%). A
Nigerian study was done by Adeoye et al. [20]. and a UK study by Z.B.
Perkins et al. [4]. showed nearly the same patterns of the mechanism of
civilian vascular trauma. A systemic review of trauma in Ethiopia done
by A. Azaj, et al. [14] showed that the commonest mechanism of trauma,
in general, was motor vehicle injury with an average of 30.3% followed
by homicidal injury of 24.4%. Even if it doesn’t reflect the mechanism
of injury pertaining specifically to the civilian vascular trauma, it
can help us to mitigate and where to focus in terms of preventive
measures.
Trauma to vessels of the extremity based on the mechanism
and level of vascular injury might also have an injury to other tissues.
Most patients with vascular injury to both the upper and lower limb can
suffer from an associated injury and it could reach up to 90% [12, 20,
22, 26, 27]. Our study showed that 45.9% of cases with an associated
injury. One of the risks to patients with the extremity vascular injury
is limb loss; it is most commonly due to the magnitude of associated
injuries to the soft tissue, bones (i.e., Gustilo III C open fracture),
or nerves; apart from a delay in the diagnosis and/or revascularization
& thrombosis of the injured vessel [28]. Orthopedic fracture is the most
commonly observed associated injury followed by nerve injury [20, 22].
In Blunt trauma an associated fracture and/or dislocation could reach up
to 95% [25] and if it is a comminuted fracture, regardless of the
mechanism, the risk of amputation increases [16, 17, 29, 30]. The
current study also showed that fracture and/or dislocation was the
commonly associated injury, followed by nerve injury.
Ischemia
tolerance time for muscles and nerves is only 6-8hours. So early
presentation and intervention within the golden period of injury to the
extremity vessels has a better limb outcome. This is facilitated by
rapid transportation and the availability of a nearby trauma center or
health facility which is lacking in most low-income countries. A
Nigerian [19] and Nepalese [22] study demonstrated that only 33% and
48%, respectively, of extremity vascular trauma patients presented
within the golden hour. Our study also showed that a small proportion of
patients(32.9%), presented within 6 hours. In the Latin American survey,
78% of patients were managed within 6 hours of injury [31]. Because of
the urgent need for prompt management and lack of available diagnostic
technology, most decisions in low-income countries are mainly based on
clinical criteria [19, 31]. The clinical-based decision was employed in
55.3% of patients in the current study.
The commonly injured vessel
in our study was the brachial artery accounting for 36.5% followed by a
femoral artery with 22.4%; in which Onakpoya, et al. [19]. and De Silva,
et al. [32]. had shown a similar pattern with the upper extremity injury
being predominant. Even if the anatomic distribution of extremity
vascular trauma depends on the mechanism of injury, most studies
reported an otherwise different pattern with a higher incidence of lower
extremity injury and femoral artery injury being the commonest one [4,
10, 22, 31, 33].
Hafez, et al. [30]. noted that complete arterial
transection is one of the factor that determined limb outcome after
revascularization. The most frequent type of vascular injury as reported
by Sah B, et al. [22]. and Onakpoya, et al. [19]. was complete
transection with 62% & 67.5%, respectively. Our study has also shown a
similar result; that complete transection was the commonest type
accounting for 74.1%, which is followed by laceration (15.3%).
The
goals in the management of extremity vascular trauma are immediate
bleeding control, rapid resuscitation, and restoration of blood flow. A
variety of surgical techniques has been employed to restore blood flow
and the choice of repair was dependent on the extent and severity of
vascular trauma. Open surgical techniques were used in all cases and
reverse interposition venous graft was the most commonly used technique
in our study which was employed in 45.9% of cases. Khan, et al. [21].
reported that a similar method was used in 53.1%, but studies which were
done in Africa and other parts of Asia showed that the commonly used
method was end-to-end primary anastomosis [19, 20, 22]. After
revascularization a compartment syndrome can develop and it has a
negative impact on the limb outcome. But the widespread application of
prophylactic fasciotomy has influenced its true incidence [34]. In our
study prophylactic fasciotomy was done in 31.8% of cases.
The most
common complication in this study was wound infection which is seen in
more than one-third of the cases. It was also observed as the commonest
complication in different set-up, but with a lower incidence [19, 20,
22]. Extremity vascular injuries can also lead to significant
disability. The amputation rate in the current study was 8.2%, and more
than half were post popliteal artery injury. Viable limb with good
long-term functional outcome was achieved in 64.7% of cases. An African
study from Nigeria reported a limb viability rate of 58.3% [19]. A
factor that affects the outcome of vascular trauma to the extremity
mainly includes limb ischemia time and blunt trauma or the presence of
associated injury [4, 19, 21].
This study had several limitations.
Since the study was a retrospective one, it is subjected to an
information bias. Even if the source of information was from the
hospital database and patients’ charts because of the poor
documentation, it was difficult to get the full scale of the problem.
Also it was not from a well-organized trauma system which would have
given us better information. In addition, the study was done in a single
tertiary hospital, so it doesn’t truly reflect the magnitude of the
problem.
Conclusion
Extremity vascular injury mainly affects the working force and young adults of society. It could be attributed to the rise of violence which directly increases the incidence of extremity vascular injuries. Vascular injury to the extremity is a surgical emergency where a delay in the diagnosis and treatment can lead to limb loss or death. After arrival to the hospital; bleeding control, resuscitation, and restoration of blood flow are the mainstays of management. Even though, intervention with endovascular techniques is increasing in the western setup because of the unavailability of its service in our setup only open surgical techniques are applied.
Recommendations
The Ethiopian Ministry of Health should emphesize on the preventive measures to tackle the rising incidence of vascular injuries due to violence and road traffic accidents by collaborating with the Ministry of Transportation. Also should work on the expansion of vascular services with trained health professionals. Teaching hospitals should integrate a well-organized trauma system into their trauma centers if there is any. Health professionals training who are equipped with the management of vascular injuries should be made by these hospitals. Clinicians need to be aware of the impact of vascular injuries and their potential outcomes. They should also be well trained and vigilant in the management of vascular injury to the extremity. Further study should be employed by all concerned bodies to assess the overall magnitude of extremity vascular injuries at the community level.
Declarations
Funding
No funding was received.
Conflict of interest
All authors declared that there is no competing interest.
Authors approval
The manuscript has been read and approved by all authors
Availability of data and materials
A soft copy of all data used for this article are available from the corresponding author, it can be made available up at a reasonable request.
Ethics approval
The study was approved by the Research & Ethical committee of Addis Ababa University, College of health science.
References
1. Kauvar, D. S., & Wade, C. E. (2005). The epidemiology and modern
management of traumatic hemorrhage: US and international perspectives.
Critical Care, 9 Suppl 5(Suppl 5), S1-9.
2. Organization, W.
H. (2014). Injuries and violence: the facts 2014.
3. Loh, S.
A., Rockman, C. B., Chung, C., Maldonado, T. S., Adelman, M. A., Cayne,
N. S., ... & Mussa, F. F. (2011). Existing trauma and critical care
scoring systems underestimate mortality among vascular trauma patients.
Journal Of Vascular Surgery, 53(2), 359-366.
4. Perkins, Z.
B., De’Ath, H. D., Aylwin, C., Brohi, K., Walsh, M., & Tai, N. R.
(2012). Epidemiology and outcome of vascular trauma at a British Major
Trauma Centre. European Journal of Vascular and Endovascular Surgery,
44(2), 203-209.
5. Eastridge, B. J., Mabry, R. L., Seguin,
P., Cantrell, J., Tops, T., Uribe, P., ... & Blackbourne, L. H. (2012).
Death on the battlefield (2001-2011): implications for the future of
combat casualty care. Journal of Trauma and Acute Care Surgery, 73(6
Suppl 5), S431-437.
6. Beck, B., Smith, K., Mercier, E.,
Bernard, S., Jones, C., Meadley, B., ... & Cameron, P. (2019).
Potentially preventable trauma deaths: A retrospective review. Injury,
50(5), 1009-1016.
7. Sugrue, M., Caldwell, E. M., Damours, S.
K., Crozier, J. A., & Deane, S. A. (2002). Vascular injury in Australia.
Surgical Clinics of North America, 82(1), 211-219.
8. Caps,
M. T. (1998). The epidemiology of vascular trauma. Seminars In Vascular
Surgery, 11(4), 227-231.
9. Sidawy, A. N., & Perler, B. A.
(2018). Rutherford’s Vascular Surgery and Endovascular Therapy, E-Book:
Elsevier Health Sciences.
10. Mattox, K. L., Feliciano, D.
V., Burch, J., Beall, A. C., Jr., Jordan, G. L., Jr., & De Bakey, M. E.
(1989). Five thousand seven hundred sixty cardiovascular injuries in
4459 patients. Epidemiologic evolution 1958 to 1987. Annals Of Surgery,
209(6), 698-705; discussion 706-697.
11. Barmparas, G.,
Inaba, K., Talving, P., David, J. S., Lam, L., Plurad, D., ... &
Demetriades, D. (2010). Pediatric vs adult vascular trauma: a National
Trauma Databank review. Journal Of Pediatric Surgery, 45(7),
1404-1412.
12. Tan, T. W., Joglar, F. L., Hamburg, N. M.,
Eberhardt, R. T., Shaw, P. M., Rybin, D., ... & Farber, A. (2011). Limb
outcome and mortality in lower and upper extremity arterial injury: a
comparison using the National Trauma Data Bank. Vascular and
Endovascular Surgery, 45(7), 592-597.
13. Organization, W. H.
(2018). Noncommunicable diseases country profiles 2018.
14.
Azaj, A., Seyoum, N., & Nega, B. (2013). Trauma in Ethiopia revisited: a
systematic review. East and Central African Journal of Surgery, 18(2),
108-118.
15. Gebreslassie, B., Gebreselassie, K., & Esayas,
R. (2018). Patterns and Causes of Amputation in Ayder Referral Hospital,
Mekelle, Ethiopia: A Three-Year Experience. Ethiopian Journal of Health
Sciences, 28(1), 31-36.
16. Perkins, Z. B., Yet, B., Glasgow,
S., Cole, E., Marsh, W., Brohi, K., ... & Tai, N. R. (2015).
Meta-analysis of prognostic factors for amputation following surgical
repair of lower extremity vascular trauma. British Journal of Surgery,
102(5), 436-450.
17. Kauvar, D. S., Sarfati, M. R., & Kraiss,
L. W. (2011). National trauma databank analysis of mortality and limb
loss in isolated lower extremity vascular trauma. Journal of Vascular
Surgery, 53(6), 1598-1603.
18. Seyoum, N., D, G. G., & Nega,
B. (2019). Pattern of Vascular Diseases at Tikur Anbessa Specialized
Hospital, Addis Ababa, Ethiopia. Ethiopian Journal of Health Sciences,
29(3), 377-382.
19. Onakpoya, U. U., Eyekpegha, J. O.,
Ogunrombi, A., Ohuche, A. S., & Ojo, T. O. (2019). Pattern of Extremity
Arterial Injury and Outcome of Repair in Southwest, Nigeria. Nigerian
Journal of Surgery, 25(1), 85-90.
20. Adeoye, P. O., Salami,
M. A., Oyemolade, T. A., & Adegboye, V. O. (2013). CIVILIAN VASCULAR
INJURIES IN AN URBAN AFRICAN REFERRAL INSTITUTION. East African Medical
Journal, 90(12), 404-408.
21. Khan, F. H., Yousuf, K. M., &
Bagwani, A. R. (2015). Vascular injuries of the extremities are a major
challenge in a third world country. Journal of Trauma Management &
Outcomes, 9, 5.
22. Sah, B., Shrestha, K. G., Tiwari, K. K.,
& Reddy, J. (2017). Analysis of consecutive cases of vascular injury in
tertiary level hospital in Central Nepal. Journal of College of Medical
Sciences-Nepal, 13(3), 357-362.
23. Murad, M., Eweda, A.,
Abdel-Moamen, H., Hussien, M., & Elsaghir, M. (2013). Vascular trauma
and its management: one and a half years after the 25th January
revolution. Journal of the Arab Society for Medical Research, 8(1),
43-47.
24. Konstantinidis, A., Inaba, K., Dubose, J.,
Barmparas, G., Lam, L., Plurad, D., ... & Demetriades, D. (2011).
Vascular trauma in geriatric patients: a national trauma databank
review. Journal of Trauma, 71(4), 909-916.
25. Rozycki, G.
S., Tremblay, L. N., Feliciano, D. V., & McClelland, W. B. (2003). Blunt
vascular trauma in the extremity: diagnosis, management, and outcome.
Journal of Trauma, 55(5), 814-824.
26. Franz, R. W., Shah, K.
J., Halaharvi, D., Franz, E. T., Hartman, J. F., & Wright, M. L. (2011).
A 5-year review of management of lower extremity arterial injuries at an
urban level I trauma center. Journal Of Vascular Surgery, 53(6),
1604-1610.
27. Franz, R. W., Goodwin, R. B., Hartman, J. F.,
& Wright, M. L. (2009). Management of upper extremity arterial injuries
at an urban level I trauma center. Annals Of Vascular Surgery, 23(1),
8-16.
28. Feliciano, D. V., Moore, E. E., West, M. A., Moore,
F. A., Davis, J. W., Cocanour, C. S., ... & McIntyre, R. C., Jr. (2013).
Western Trauma Association critical decisions in trauma: evaluation and
management of peripheral vascular injury, part II. Journal of Trauma and
Acute Care Surgery, 75(3), 391-397.
29. Mullenix, P. S.,
Steele, S. R., Andersen, C. A., Starnes, B. W., Salim, A., & Martin, M.
J. (2006). Limb salvage and outcomes among patients with traumatic
popliteal vascular injury: an analysis of the National Trauma Data Bank.
Journal Of Vascular Surgery, 44(1), 94-100.
30. Hafez, H. M.,
Woolgar, J., & Robbs, J. V. (2001). Lower extremity arterial injury:
results of 550 cases and review of risk factors associated with limb
loss. Journal Of Vascular Surgery, 33(6), 1212-1219.
31.
Sonneborn, R., Andrade, R., Bello, F., Morales-Uribe, C. H., Razuk, A.,
Soria, A., ... & Ostria, G. (2002). Vascular trauma in Latin America: a
regional survey. Surgical Clinics of North America, 82(1), 189-194.
32.
de Silva, W., Ubayasiri, R. A., Weerasinghe, C. W., & Wijeyaratne, S. M.
(2011). Challenges in the management of extremity vascular injuries: A
wartime experience from a tertiary centre in Sri Lanka. World Journal of
Emergency Surgery, 6, 24.
33. Liu, J. L., Li, J. Y., Jiang,
P., Jia, W., Tian, X., Cheng, Z. Y., & Zhang, Y. X. (2020). Literature
review of peripheral vascular trauma: Is the era of intervention coming?
Chinese Journal of Traumatology, 23(1), 5-9.
34. Branco, B.
C., Inaba, K., Barmparas, G., Schnüriger, B., Lustenberger, T., Talving,
P., ... & Demetriades, D. (2011). Incidence and predictors for the need
for fasciotomy after extremity trauma: a 10-year review in a mature
level I trauma centre. Injury, 42(10), 1157-1163.