Open Access | Letter to Editor
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Hypopigmentation with muscular and subcutaneous atrophy as a complication of Intralesional Steroid injection in Ganglion
*Corresponding author: Sandip Kumar Rahul
Mailing address: Department of Pediatric surgery, Indira Gandhi
Institute of Medical Sciences, Patna, India.
Email: sandeep.rahul65@gmail.com
Received: 15 April 2021 / Accepted: 26 May 2021
DOI: 10.31491/CSRC.2021.06.073
Dear Sir
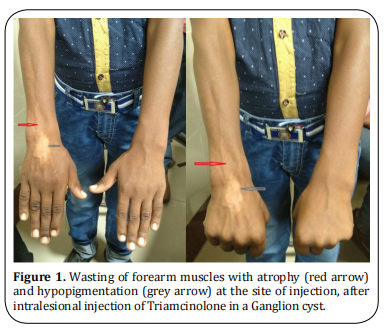
Although ganglion cysts are commonly encountered in surgical practice, recurrences have been reported with almost all modalities used in its management [1]. We report an unusual complication following intra-lesional steroid injection. Consent was taken from the father of the patient before presenting this case; permission was also taken from the Institutional Ethics Committee (Letter No. 106/IEC/2021/IGIMS, dated 12/05/2021). A ten- year-old-male presented with a ganglion cyst over the dorsum of the right hand which was treated with aspiration and intralesional Triamcinolone injection. Lesion disappeared when he came for follow-up after one month. He, however, developed hypopigmentation at the site of injection of steroid along with atrophy of the dorsal forearm muscles and subcutaneous tissue which became more obvious after five months of the procedure (Figure 1). There was no deficiency in the movements or sensation of the hand or forearm as per the patient but on examination; we found that extension at the wrist joint on the involved side was weaker. What could have caused this complication?
Local spillage of steroid, over-dosage, the effect of the
medication (more than anticipated) and nerve injury
could all be the cause. Lymphatic channels have an
important role in returning macromolecules from the
interstitial fluid into the venous circulation. Triamcinolone, being a macromolecule takes the lymphatic pathway but it also finds its way out due to its lipophilic
property by the virtue of the acetonide group between
carbon-15 and 16 in its structure [2, 3]. So, Injected
Triamcinolone takes the lymphatic pathway and may
come out at places to cause hypopigmentation and localized atrophy as seen in our case. It has been found
that the number of melanocytes is normal in such cases of steroid-induced hypopigmentation but it appears
that their functioning is suboptimal [4].
As far as muscle atrophy and myopathy following steroid usage is concerned, several investigators have
reported the atrophy of Type 2b fibers (fast-twitch)
fibers on exposure to steroids without any inflammation or necrosis and that it is more with the use of
fluorinated steroids like Triamcinolone as in our case
[5, 6]. Multiple mechanisms have been suggested to explain steroid-induced myopathy [7]. However, muscle
proteolysis mainly through the ubiquitin-proteasome
system is the most important mechanism [7]. Several investigators have observed muscular, subcutaneous and
fat atrophy following local steroid injection [8, 9].
On the dorsum of the hand, the scapholunate ligament
is the most important site for the occurrence of ganglions [10]. This was the site of the ganglion in our patient. Muscular atrophy which followed intra-lesional
steroid injection predominantly involved the Extensor
digitorum, Extensor pollicis longus and Extensor pollicis brevis. These affected the extensor movement
against resistance at the wrist joint and of the thumb
and other digits. However, the patient didn’t complain
of any difficulty in his daily work. For these findings,
the patient was evaluated by the physiotherapy team
who recommended passive range of motion movements, followed by active exercises and then resistance
exercises involving the extensors of the wrist and the
metacarpophalangeal and interphalangeal joints of the
involved digits. The patient did well with this exercise
regime. There are encouraging results of local electrical stimulation or focussed ultrasonic stimulation of
atrophic muscles in stimulating the atrophic muscles
to gain bulk and strength [11,12]. In our patient, local
electrical stimulation was used initially for a month on
alternate days and then exercise therapy was continued.
For subcutaneous fat atrophy, if it doesn’t get corrected
by itself after around a year of observation, the local fat
injection has been tried successfully [13]. Shumaker et.
al. discussed the positive role of local normal saline infiltration in four cases of persistent Cutaneous atrophy
following steroid injection [9]. Our patient didn’t need
any such intervention for fat or cutaneous atrophy.
Ganjoo et. al. reported a linear streak of depigmentation following a single intralesional Triamcinolone
injection in a ganglion over the anterior aspect of the
wrist [14]. A similar pattern of hypopigmentation has
been described by other investigators [2,4]. Venkatesan
et. al. reported linear hypopigmentation and cutaneous
atrophy following intra-articular steroids for De Quervain’s tendonitis [4]. For hypopigmentation, our patient
received 0.1% tacrolimus and 8- methoxy Psoralen
topically after consulting a dermatologist.
We have had recurrences with all modalities of treatment (surgery, simple aspiration, intralesional injection of steroids or sclerosants and closed rupture of
these cysts) at our center and we choose the appropriate intervention after discussing with the relatives all
these options including their complications. We have
used aspiration with intralesional steroid injection
using a single dart technique after appropriate counseling in a few of our patients who have not chosen an
invasive procedure like surgery for management.
In this case, Parents refused to get the involved sitebiopsied. This patient was then managed by the combined efforts of the dermatologists and Physiotherapists. After 20 months of intralesional injection, the
wasted muscles regained their original shape with
regular physiotherapy but some hypopigmentation has
still persisted.
We concluded that intralesional steroid injection may
result in significant hypopigmentation, atrophy of subcutaneous tissue and fat and muscular wasting at sites
distant to the injection site and these complications
along with high recurrence rate must be taken into
consideration while planning management of a Ganglion cyst.
Declarations
Authors’ contributions
All the authors were involved in the management of the patients; Sandip Kumar Rahul and Digamber Chaubey also did the framing of the manuscript; all the authors have read and approved the manuscript before submission.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethics approval
Consent was taken from both parents and the child before submitting the case and clinical pictures.
References
1. Chatterjee, S., Basu, A., Gupta, S., & Biswas, S. (2014).
Comparative study of recurrence and complications using various sclerosants by single dart technique in treatment of ganglion cysts. Indian Journal of Surgery, 76(5),
350-353.
2. Prasad, K., Madke, B., Kar, S., Sinha, A. K., & Yadav, N.
(2015). Linear rays of depigmentation along lymphatics
after intralesional corticosteroid therapy. Indian dermatology online journal, 6(6), 456-457.
3. Chembolli, L., Rai, R., & Srinivas, C. R. (2008). Depigmentation along lymphatic channels following intralesional
corticosteroid injection. Indian journal of dermatology,
53(4), 210.
4. Venkatesan, P., & Fangman, W. L. (2009). Linear hypopigmentation and cutaneous atrophy following intra-articular steroid injections for de Quervain’s tendonitis. Journal
of drugs in dermatology: JDD, 8(5), 492-493.
5. Surmachevska, N., & Tiwari, V. (2020). Corticosteroid Induced Myopathy. StatPearls [Internet].
6. Owczarek, J., Jasiñska, M., & Orszulak-Michalak, D. (2005). Drug-induced myopathies. An overview of the possible
mechanisms. Pharmacol Rep, 57(1), 23-34.
7. Schakman, O., Gilson, H., & Thissen, J. P. (2008). Mechanisms of glucocorticoid-induced myopathy. The Journal
of endocrinology, 197(1), 1-10.
8. Park, S. K., Choi, Y. S., & Kim, H. J. (2013). Hypopigmentation and subcutaneous fat, muscle atrophy after local corticosteroid injection. Korean journal of anesthesiology,
65(6 Suppl), S59.
9. Shumaker, P. R., Rao, J., & Goldman, M. P. (2005). Treatment of local, persistent cutaneous atrophy following
corticosteroid injection with normal saline infiltration.
Dermatologic surgery, 31(10), 1340-1343.
10. Angelides, A. C., & Wallace, P. F. (1976). The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic
anatomy, and surgical treatment. The Journal of hand
surgery, 1(3), 228-235.
11. Kus, G., & Yeldan, I. (2019). Strengthening the quadriceps
femoris muscle versus other knee training programs for
the treatment of knee osteoarthritis. Rheumatology international, 39(2), 203-218.
12. Bueno, C. R. D. S., Pereira, M., Favaretto Junior, I. A., Bortoluci, C. H. F., Santos, T. C. P. D., Dias, D. V., ... & Rosa Junior, G.
M. (2017). Electrical stimulation attenuates morphological alterations and prevents atrophy of the denervated
cranial tibial muscle. Einstein (Sao Paulo), 15(1), 71-76.
13. Imagawa, K., & Ohkuma, S. (2010). A case of fat injection for treating subcutaneous atrophy caused by local
administration of corticosteroid. Tokai J Exp Clin Med,
35(2), 66.
14. Shikhar, G., & Vinita, G. (2018). Perilymphatic Linear Depigmentation in a Child following intralesional Steroid
for Ganglion. Archives of Dermatology and Skin Care. 1(2), 1-2.