Open Access | Case Report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Aneurysmal bone cyst arising in iliopubic chondromyxoid fibroma – a case report
*Corresponding author: João Soares do Vale
Mailing address: Rua Padre Cruz, 148 1º, 4050-219 Porto, Portugal.
Email: jsoaresvale@gmail.com
Received: 15 April 2021 / Accepted: 26 May 2021
DOI: 10.31491/CSRC.2021.06.074
Abstract
Chondromyxoid fibroma is rare cartilaginous tumor, accounting for 0.5% of all primary bone tumors and 2% of benign bone tumors. Areas of aneurysmal bone cysts (ABC) may be found within CMF in 8.6% of cases. A 20-year-old man presents pain due to a mass on iliopubic ramus that was diagnosed as an aneurysmal bone cyst arising from a chondromyxoid fibroma. This case confirms the rare association between aneurysmal bone cyst and chondromyxoid fibroma. Although aneurysmal bone cyst is more frequently associated with highly vascularized tumors, it is important to consider the diagnosis in the presence of chondromyxoid fibroma.
Keywords
Chondromyxoid fibroma; scecondary aneurysmal bone cyst; iliopubic ramus
Introduction
Chondromyxoid fibroma (CMF) was described by Jaffe
and Lichtenstein as a distinctive entity in 1948 [1]. The
definition given by the World Health Organization
(WHO) is a benign cartilaginous neoplasm, composed
of lobules formed by spindle-shaped cells with myofibroblastic features at the periphery, and stellate and
chondrocyte-like cells towards the center, the extracellular matrix of the lobules are fibrous at the periphery
and myxoid and chondroid towards the center [2].
This rare cartilaginous tumor, accounting for 0.5% of
all primary bone tumors and 2% of benign bone tumors, occurs predominantly in adolescents and young
adults and more commonly in males [2,3]. This tumor
can occur at almost any osseous site, with a predilection for bones of the lower extremities, usually the
proximal tibia [2,3]. Flat-bones account for 25 to 30.3%
of cases, with ilium been the most affected [2,4,5].
Areas of aneurysmal bone cysts (ABC) may be found
within CMF in 8.6% of cases [4].
ABCs is the result of specific pathologic change, which
is probably the result of trauma or a tumor-induced
anomalous vascular process [6]. The most common is
giant cell tumor, but others like osteoblastoma, angioma, chondroblastoma, telangiectatic osteosarcoma are
common too [6].
To the best of our knowledge, there is not any case
of an aneurysmal bone cyst arising from an iliopubic
chondromyxoid fibroma.
Case Report
A 20-year-old man with no relevant medical history
presents mechanical pain in the left inguinal region
with 6 months of evolution. Physical examination revealed a 4 cm x 2 cm x 2 cm palpable mass in the groin.
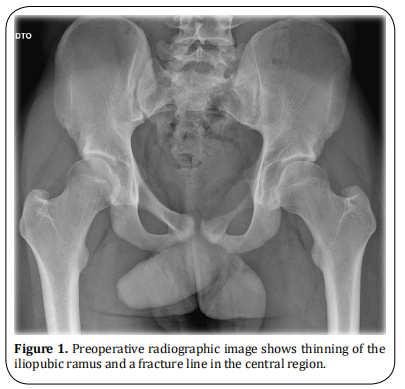
The conventional radiography (Figure 1) revealed an
osteolytic tumor in the left ilio-pubic ramus, with cortical thinning and a fracture line in the central region.
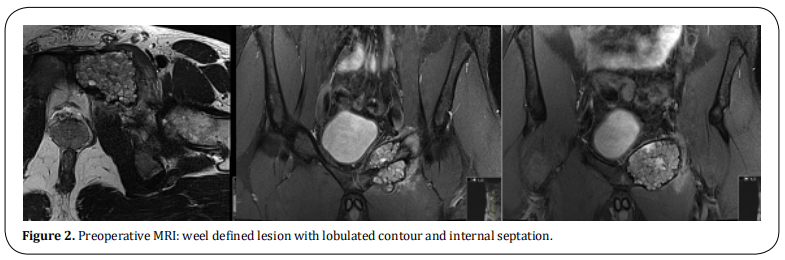
MRI presents a well-defined lesion with lobulated contour and internal septation (Figure 2) suggesting an
aneurysmal bone cyst or telangiectatic osteosarcoma.
Ultrasonography-guided percutaneous biopsy diagnosed a chondromyxoid fibroma.
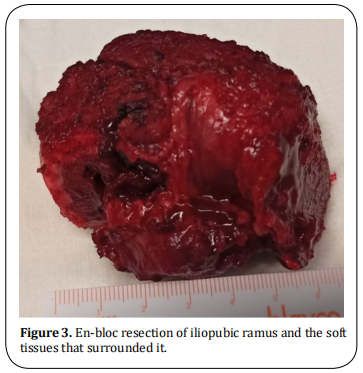
The tumor excision was performed through an anterior approach. A Pfannenstiel incision was extended
to the proximal region of the left thigh, in order to
isolate and protect the femoral neurovascular bundle.
The spermatic cord was recognized and protected. The
bladder was protected as well. Pubic symphysis and
the anterior rim of the acetabulum were identified and
used as anatomical references to osteotomies. An enbloc resection of iliopubic ramus and the soft tissues
that surrounded it was made (Figure 3). No pelvic ring
reconstruction was considered for mechanical purposes. The abdominal wall was reinforced with GoreTex® mesh, that was attached to symphysis, anterior
acetabular rim and abdominal wall muscle fascia to
prevent intra-pelvic herniation.
The patient was discharged home 2 days after surgery,
with partial weight bearing and no evidence of complications.
Microscopic examination showed complete excision of
the lesion, with free margins.
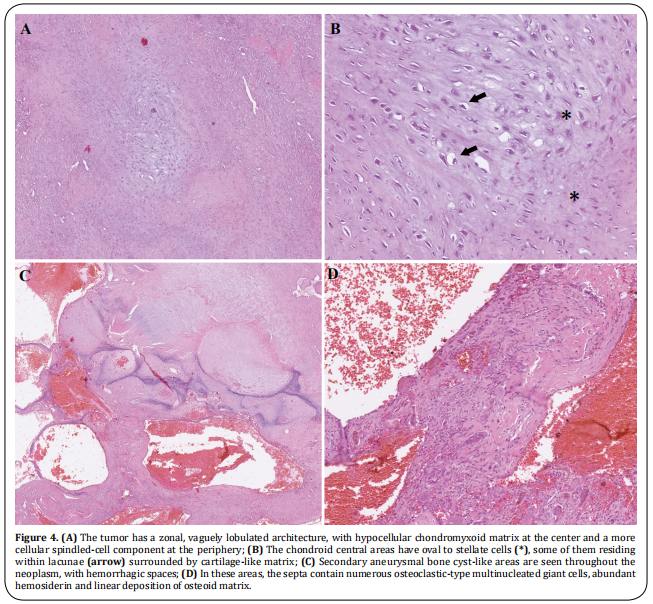
Histological analysis revealed a benign mesenchymal
neoplasm, well delimitated and organized in chondromyxoid lobes of variable cellularity, with stellate
cells in myxoid areas and lacunar cells in chondroid
areas features consistent with chondromyxoid fibroma
(Figure 4A and 4B). There were also abundant hemorrhagic cavitated areas developing within the tumor,
with septa rich in osteoclastic-type multinucleated
giant cells and with deposition of linear immature osteoid, typical of aneurysmal bone cyst transformation
(Figure 4C and 4D), explaining the images seen in MRI.
The neoplasm occupied and expanded the ischio-pubic
ramus, reaching the subcartilaginous area of the pubic
symphysis, but it didn’t invade the adjacent soft tissue,
as it was surrounded by a thin layer of woven bone, a
consequence of cortical bone remodeling.
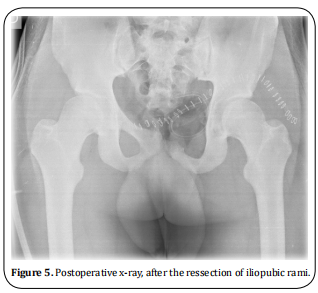
After 1 year of follow-up, the patient is pain-free, without functional impairment or complications. There is
no recurrence until the present (Figure 5).
Discussion
This case represents an unusual localization for this
type of tumor. A literature review of 278 cases of CMF
of bone, reported that 30.3% of cases occurred in flat
bones. Of these only 1 case (1.2%) was located on the
pubis and 2 on ischium (2.4%) [4].
As the name indicates, chondromyxoid fibromas show
a variety of histological features. The classic histological feature is stellate or spindle-shaped cells arranged
in lobules in a myxoid background [4]. However, a lobulated pattern was seen in only 86.7% of cases, and can
present a macro or microlobular pattern isolated or a
mixture [4].
In our case, the tumor was accompanied by an area of
ABC. The origin of the term ABC comes from an article by Jaffe and Lichtenstein in 1942 [7]. They postulated
that ABC might be a secondary phenomenon due to
hemorrhagic “blow-out” in a preexisting lesion, which
may be destroyed in the process [7]. A preexisting lesion was identified in approximately one third [6].
ABCs conventional treatment has been the surgical
removal of the entire lesion or as much as possible,
with recurrence seen in 10-70% of cases [2,6]. Spontaneous regression following incomplete removal is very
unusual [2]. More recently, non-surgical polidocanol
sclerotherapy demonstrates to be a safe and effective
option even for aggressive ABCs, depending on location and surgical risks [8]. Appropriate treatment requires realizing that it has a specific pathophysiologic
origin and identifying the preexisting lesion. If no coexisting lesion is identified, lesions are usually treated with curettage and bone grafting [6].
The typical treatment of CMF by curettage has a 20%
to 25% recurrence rate, lowering to 7% with the addition of bone grafting [9,10]. Resection provides lower
recurrence rates but is not always feasible.
Based on the system proposed by Enneking WF and
Dunham WK, this case of CMF involves zone III (involvement of pubis and ischium bones) [11]. A review of
8 cases describing surgical management of CMF of the
pelvis, reported two cases of involvement of superior
ramus of the pubis. One was treated with resection
without grafting and complicated with pelvic internal
organs herniation. In the second case, reconstruction
was done using fibular strut allograft, with no complication on follow-up [12]. Another case of CMF of iliopubic ramus presented good results with aggressive
curettage and chip bone grafting. The author reclaims
this procedure as safe, easy, and less morbid for this
anatomic site [13].
In our case, we resected iliopubic ramus and used a
Gore-tex® surgical mesh to prevent intra-pelvic herniation. Resection should be performed for large lesions
or in anatomic sites such as the complex pelvis. Such
a procedure does not increase the risk of fracture and
reduces the likelihood of recurrence or a second surgery.
The secondary ABC arising from CMF was verified
histologically. It is associated with a significant recurrence rate and the surgical strategy adopted was then
confirmed the most appropriate.
This case represents a rare tumor, in an uncommon
location, with an atypical histological transformation.
This case shows the rare association between ABC and CMF. Although secondary ABCs are more frequently
associated with highly vascularized tumors, it is important to consider the diagnosis of CMF in the presence of an ABC, as it may alter the clinical approach to
minimize the risk of recurrence.
Declarations
Authors’ contributions
João Vale: Wrote the manuscript, Performed the literature review;
Sara Diniz: Edited the paper;
Filipe Rodrigues: Edited the manuscript;
Ana Ribau: Edited the paper;
André Coelho: Edited the manuscript;
Vânia Oliveira: Edited the manuscript;
Pedro Cardoso: Edited the manuscript.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethics approval
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
1. HL, J. (1948). Chondromyxoid fibroma of bone. A distinctive benign tumor likely to be mistaken especially for
chondrosarcoma. Arch Pathol, 45, 541-551.
2. Spieler, P., & Rössle, M. (2012). Soft Tissue and Bone. In
Nongynecologic Cytopathology (pp. 1053-1105). Springer, Berlin, Heidelberg.
3. Greenspan, A., Jundt, G., & Remagen, W. (2007). Differential diagnosis in orthopaedic oncology. Lippincott Williams & Wilkins.
4. Wu, C. T., Inwards, C. Y., O’laughlin, S., Rock, M. G., Be about, J. W., & Unni, K. K. (1998). Chondromyxoid fibroma
of bone: a clinicopathologic review of 278 cases. Human
pathology, 29(5), 438-446.
5. Zillmer, D. A., & Dorfman, H. D. (1989). Chondromyxoid
fibroma of bone: thirty-six cases with clinicopathologic
correlation. Human pathology, 20(10), 952-964.
6. Kransdorf, M. J., & Sweet, D. E. (1995). Aneurysmal bone
cyst: concept, controversy, clinical presentation, and imaging. AJR. American journal of roentgenology, 164(3),
573-580.
7. JAFFE, H. L., & Lichtenstein, L. (1942). Solitary unicameral bone cyst: with emphasis on the roentgen picture, the
pathologic appearance and the pathogenesis. Archives of
Surgery, 44(6), 1004-1025.
8. Brosjö, O., & Tsagozis, P. (2014). Treatment of an aggressive aneurysmal bone cyst with percutaneous injection
of polidocanol: a case report. Journal of medical case reports, 8(1), 1-4.
9. Subach, B. R., Copay, A. G., Martin, M. M., Schuler, T. C., &
Romero-Gutierrez, M. (2010). An unusual occurrence
of chondromyxoid fibroma with secondary aneurysmal
bone cyst in the cervical spine. The Spine Journal, 10(2),
e5-e9.
10. Gherlinzoni, F., Rock, M., & Picci, P. (1983). Chondromyxoid fibroma. The experience at the Istituto Ortopedico
Rizzoli. JBJS, 65(2), 198-204.
11. Enneking, W. F., & Dunham, W. K. (1978). Resection and
reconstruction for primary neoplasms involving the innominate bone. The Journal of bone and joint surgery.
American volume, 60(6), 731-746.
12. Jamshidi, K., NAJD, M. F., & JAFARI, D. (2015). Chondromyxoid fibroma of pelvis, surgical management of 8
cases. Arch Iran Med, 18(6), 367-370.
13. Arikan, M., Toğral, G., Yildirim, A., & Aktaş, E. (2016).
Chondromyxoid fibroma of the pubic ramus: a case report and literature review. Acta Orthop Traumatol Turc,
50(1), 115-119.