Open Access | Case Report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Pneumatosis intestinalis in a patient with trichobezoar – Rare association
*Corresponding author: Varuna Bhagya Pathirana
Mailing address: Department of General Surgery, Ward 32, National Hospital, Colombo, Sri Lanka.
Email: varunapath@gmail.com
Received: 29 December 2020 / Accepted: 28 January 2021
DOI: 10.31491/CSRC.2021.03.069
Abstract
This case report describes a young girl who presented with chronic epigastric pain and abdominal mass without noticeable psychiatric illness or trichotillomania and subsequently trichobezoar was found to be the reason for her symptoms. She underwent laparotomy to retrieve the bezoar. During laparotomy extensive pneumatosis of the small bowel was noted where this association was not previously reported in the literature. Since pneumatosis was not symptomatic no bowel resection was carried out. She made an uneventful recovery. This illustrates that trichobezoar is an important cause to consider in young females with chronic abdominal pain even in the absence of clear evidence for trichotillomania. Rarely, this can be associated with intestinal pneumatosis. Intestinal pneumatosis does not warrant treatment unless it causes symptoms.
Keywords
Trichobezoar; epigastric pain; pneumatosis intestinalis; trichotillomania; pneumoperitoneum
Introduction
Trichobezoar is a mass of ingested hair within the gastrointestinal tract [1]. This rare cause was found to be the reason for chronic epigastric pain of a young girl in this case report without apparent psychiatric illness. She was incidentally found to have pneumatosis intestinalis (PI) which may be or may not be related to trichobezoar [2].
Case Report
A 17-year-old girl presented with epigastric pain for
one-year duration associated with nausea, postprandial abdominal fullness, early satiety, and episodic vomiting occurring 3-4 times a month. Her bowel habits
were normal and there was no per rectal bleeding or
melena. She was admitted to the hospital due to worsening of symptoms over two weeks with more frequent
vomiting. She denies trichotillomania and there was no history of psychiatric illness or behavioral abnormality
and her school performances were average.
She was not pale, anicteric, BMI was 17.18 kg/m2
and
no abnormality was noted in her hair. Abdominal examination revealed a firm lump involving epigastric
and right hypochondria extending 6 cm from the costal
margin. The rest of the abdominal examination was
unremarkable. Her hemoglobin was 12.7 g/dl, serum
albumin was 4.0 g/dl and the rest of the laboratory investigations, including bilirubin levels, serum amylase,
and serum electrolytes were within the normal range.
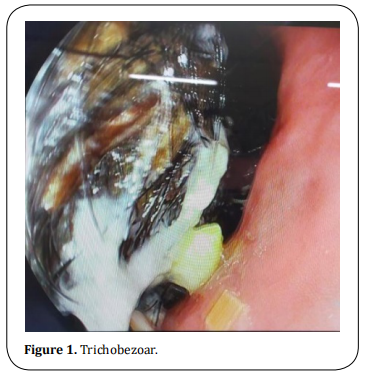
Gastroduodenoscopy revealed large trichobezoar
where the scope was not negotiable beyond the body
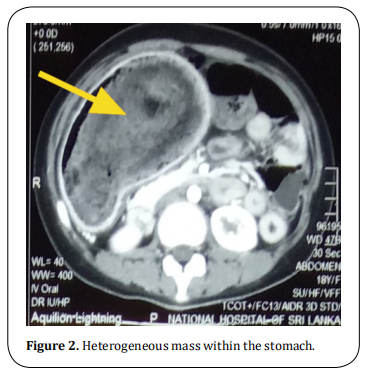
of the stomach (Figure 1). CECT showed grossly distended stomach with non-enhancing intraluminal mass
extending up to the first part of duodenum suggestive
of a bezoar (Figure 2) and intramural gas in the small
and large intestine suggestive of pneumatosis.
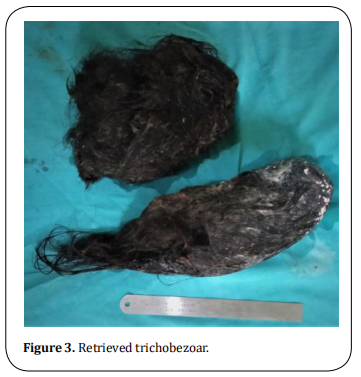
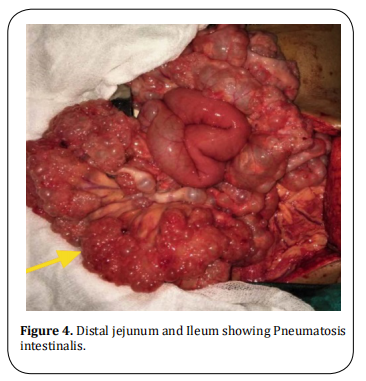
She underwent laparotomy and the bezoar was retrieved via gastrotomy (Figure 3). A gastric wall thickening was observed with a thickness of 5-6 mm. Distal
jejunum and entire ileum showed gaseous outpouchings
of variable size ranging from few millimeters to 1 cm indicating extensive intestinal Pneumatosis (Figure 4) and
was left unattended since the patient was asymptomatic. She made the uneventful postoperative recovery . She was referred to a psychiatrist on discharge from the
hospital and no active treatment was recommended.
Discussion
Bezoars are masses formed from ingested foreign material and identified in less than 5% of all upper gastrointestinal endoscopy [1]. They are most commonly
found in the stomach. Trichobezoar is the rarest of
them accounting for 6% of all bezoars and invariably
related to trichotillomania and trichophagia [1] which
can be a part of a psychiatric illness. Even though the
presence of trichobezoar is a piece of clear evidence
for trichophagia, some patients may deny these habits
similar to this case.
Bezoars can be asymptomatic particularly when they
are small and symptomatic patients have epigastric pain, nausea, and vomiting, early satiety which is nonspecific and can be overlooked as young patients may
not undergo routine endoscopy leading to delay of
diagnosis. Because around 90% of these patients are
young females [1,4], this case illustrates the importance
of considering trichobezoar as a cause for unexplained
abdominal pain in a young female even with the absence of clear psychiatric illness or evidence for trichotillomania.
Trichobezoar needs early intervention since it is
known for many complications such as gastric erosion
and bleeding, perforation, and gastric outlet obstruction. The extension of trichobezoar into the small bowel which is known as Rapunzel Syndrome can lead to
small bowel obstruction, pancreatitis, and cholangitis
[1,3,5]. Open surgery is considered the best method since
it is technically easy and has a high success rate of
complete removal of the bezoar with low complication
rates [1,3,5]. Laparoscopic and endoscopic interventions
are shown to be less effective [1,3,5]. Most patients will
only need gastrotomy and/or enterotomy for retrieval
of bezoar, but complicated cases may require subtotal
gastrectomy or intestinal resection [1]. Following the
successful removal of trichobezoar patients will need
surveillance endoscopy for few years to confirm the
patient has come out of trichotillomania [3].
Pneumatosis intestinalis (PI) is a rare condition that
has a wide range of clinical presentations from benign
asymptomatic condition to a life-threatening surgical
emergency due to adhesion obstruction or spontaneous bowel perforation [2,6]. Morphologically PI is seen
in “bubbles like” type (cystoides) which was noted in
this patient or a continuous band-like type [2]. It may be
idiopathic (primary), occasionally identified in asymptomatic patients, or secondary to various gastrointestinal or pulmonary diseases [2,7]. Inflammatory bowel
disease, chronic bowel infections and infestations,
bowel obstruction and pyloric obstruction, diverticulitis, bowel ischemia, toxic megacolon are some of the
common gastrointestinal conditions related to PI [7,8].
Some of the non-gastrointestinal conditions related
to PI are pulmonary diseases like asthma, and emphysema, collagen vascular diseases, immunosuppression,
organ transplantation ect [7,8]. Direct association with
trichobezoar and PI is not documented in the literature. Chronic inflammation of the bowel wall secondary to hair, partial pyloric, and small bowel obstruction
may have contributed to pneumatosis in this patient
since these causes are known to associate with PI [7].
Most of the time PI will present with symptoms related to its underlying disease. However, vomiting, abdominal distention, weight loss with the involvement of the
small bowel and diarrhea, hematochezia with the involvement of the large bowel is reported as the symptoms related to PI [8].
A plain abdominal x-ray may reveal pneumatosis but
a contrast-enhanced CT scan of the abdomen is more
sensitive in detecting PI and particularly in acute presentation it can help in identifying Intraluminal gas
from intramural gas, the air within the biliary system,
ischemic bowel, pneumoperitoneum, ascites which will
help in the decision to ope rate [2,6,7].
Pneumatosis intestinalis is treated according to the
underlying cause and surgery is usually reserved for
patients presenting with acute abdomen due to perforation or obstruction. Patients with clinical and laboratory evidence of abdominal sepsis elevated serum
amylase, and presence of portal venous gas need urgent surgery where asymptomatic cases are managed
non operatively [2,6,8]. Pneumoperitoneum alone should
not be considered as an indication for surgery since it
was noted in 50% of patients with PI [6]. In this patient
resection of the involved segment was not necessary
as it is uncomplicated and neither feasible considering
the extensive involvement of the small bowel.
Conclusion
Trichobezoar can be a cause for chronic unexplained abdominal pain in young females, where it may be not suspected in the absence of trichotillomania and hair loss. Trichobezoar and intestinal pneumatosis are rare clinical entities where this association was not documented previously. Pneumatosis intestinalis needs individualized treatment based on clinical presentation.
Declarations
Authors’ contributions
All authors made substantial contributions to merit inclusion as co-authors. All authors approved the final manuscript.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethics approval
Not applicable.
Consent for publication
Patient consent was obtained for publication without personal details.
References
1. García-Ramírez, B. E., Nuño-Guzmán, C. M., Zaragoza-Carrillo, R. E., Salado-Rentería, H., Gómez-Abarca, A., & Corona, J. L. (2018). Small-bowel obstruction secondary to
ileal trichobezoar in a patient with Rapunzel syndrome.
Case reports in gastroenterology, 12(3), 559-565.
2. Berritto, D., Crincoli, R., Iacobellis, F., Iasiello, F., Pizza, N.
L., Lassandro, F., ... & Grassi, R. (2014). Primary pneumatosis intestinalis of small bowel: a case of a rare disease.
Case reports in surgery, 2014.
3. Wolski, M., Gawłowska-Sawosz, M., Gogolewski, M.,
Wolańczyk, T., Albrecht, P., & Kamiński, A. (2016). Trichotillomania, trichophagia, trichobezoar-summary of three
cases. Endoscopic follow up scheme in trichotillomania. Psychiatr Pol, 50(1), 145-52.
4. Dindyal, S., Bhuva, N. J., Ramdass, M. J., & Narayansingh, V.
(2008). Trichobezoar presenting with the’comma sign’in
Rapunzel Syndrome: a case report and literature review.
Cases journal, 1(1), 1-4.
5. Gorter, R. R., Kneepkens, C. M. F., Mattens, E. C. J. L., Aronson, D. C., & Heij, H. A. (2010). Management of trichobezoar: case report and literature review. Pediatric surgery
international, 26(5), 457-463.
6. Tahiri, M., Levy, J., Alzaid, S., & Anderson, D. (2015). An approach to pneumatosis intestinalis: Factors affecting
your management. International journal of surgery case
reports, 6, 133-137.
7. Ho, L. M., Paulson, E. K., & Thompson, W. M. (2007). Pneumatosis intestinalis in the adult: benign to life-threatening causes. American Journal of Roentgenology, 188(6),
1604-1613.
8. Zhang, H., Jun, S. L., & Brennan, T. V. (2012). Pneumatosis
intestinalis: not always a surgical indication. Case reports
in surgery, 2012.