Open Access | Case Report
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Solitary cerebral metastasis from undiagnosed prostate cancer. Potential role of multiparametric MRI prostate in pre-treatment diagnostic protocols
*Corresponding author: Avinash Kumar Kanodia
Mailing address: Consultant Radiologist, Radiology Department,
Ninewells Hospital & Medical School, Dundee, United Kingdom.
Email: avinash.kanodia@nhs.scot
Received: 23 August 2020 / Accepted: 05 September 2020
DOI: 10.31491/CSRC.2020.09.058
Abstract
A 73-year-old man presented with a three-week history of weakness and loss of co-ordination of the left-hand side and weakness of left-hand grip. MRI brain revealed an enhancing lesion in the right parietal lobe, adjacent to the central sulcus, with surrounding oedema and a small satellite lesion in motor cortex. Body CT and FDGPET CT revealed no obvious primary neoplasm. The patient underwent craniotomy with resection of the lesion, subsequent histopathology confirmed a metastatic carcinoma of likely prostate cancer primary origin. The patient was on 5-ARI (Finasteride) for lower urinary tract symptoms that decrease serum PSA levels to half and had benign feeling prostate on digital rectal examination (DRE). Subsequent MRI prostate confirmed presence of a lesion with very high probability of prostate cancer. The patient’s serum Prostate Specific Antigen (PSA) level was 6.8 (13.6 corrected for Finastride) which is relatively low in the context of metastatic disease. Given the recent NICE guidelines of using pre-biopsy multiparametric MRI (mpMRI) for diagnosis of prostate cancer, we suggest that in patients with cerebral metastases of unknown primary, with negative body CT, FDG PET-CT, low PSA and negative DRE, mpMRI prostate should be included in diagnostic protocol in the selected group of men, to enable early diagnosis and performing more suitable and targeted treatment.
Keywords
Brain metastasis; prostate cancer; multiparametric MRI; metastasis of unknown origin
Introduction
Prostate cancer (PCa) is the second most common cancer among males worldwide and remains the sec ond largest contributor to cancer-related mortality amongst males in the UK [1,2]. However, it is still con sidered mostly an indolent disease with overall 5-year survival rate for PCa estimated at 86.6% [3]. Early clinical manifestations of PCa are often non-specific or absent at the time of diagnosis and PCa is known to metastasize widely, preferentially to bone and lymph nodes [4]. Traditionally, the diagnosis is confirmed via prostate biopsy, frequently following a rise in Prostate Specific Antigen (PSA), although its rise depends upon disease burden and is most notable with skeletal metastases. Confirmed cerebral metastases in PCa are considered rare, occurring mostly as single, supratentorial lesion [5], however it is not certain if the low incidence is also partly due to undiagnosed cases with cerebral metastasis of unknown origin, since targeted prostate imaging is not performed unless prostate cancer is clinically suspected, and not all such cases are resected/biopsied. Traditional whole body CT imaging would certainly miss these lesions and would lead to false belief of absence of prostate cancer, in particular in those men on 5-alpha reductase inhibitor (5-ARI) such as Finastride, a drug known to lower PSA levels. However, there is now a new approach to diagnose prostate cancer with principal role of pre-biopsy multiparametric MRI (mpMRI) [6], we believe that it can further alter the diagnostic approach for assessment of brain metastases from unknown primary.
Case Presentation
A 73-year-old man with a past medical history of
sarcoidosis and benign prostate enlargement (BPE)
presented with three-week history of progressive grip
weakness and loss of co-ordination in the left hand. His
family reported personality changes and occasional
episodes of urinary incontinence. Patient was a non
smoker. He had a single previous episode of painless
haematuria 9 years ago, which spontaneously resolved.
He was investigated by Urology and investigations including, flexible cystoscopy, CT urography and urine
cytology were all satisfactory. His digital rectal examination (DRE) showed BPE and the patient was commenced on the 5-ARI, Finasteride, for treatment of BPE
to good effect.
CT head revealed a solid-cystic intra-axial enhancing
lesion high within the right anterior parietal lobe (adjacent to central sulcus) with surrounding vasogenic
oedema. The patient’s cerebral lesion was thought
to be suspicious for metastasis and subsequent body
CT CAP (chest, abdomen and pelvis) revealed no primary neoplasm but lung appearances and mediastinal
lymphadenopathy in keeping with known sarcoidosis.
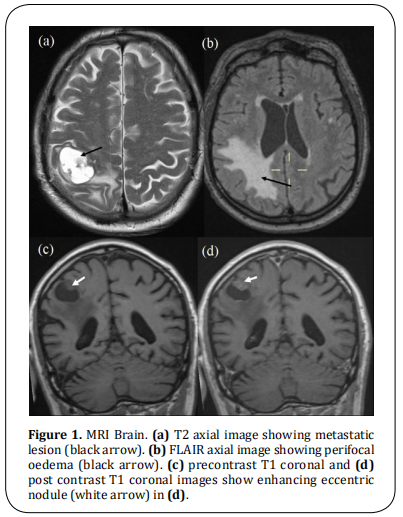
MRI of the brain confirmed presence of a single lesion,
just posterior to the right central sulcus (Figure 1). A
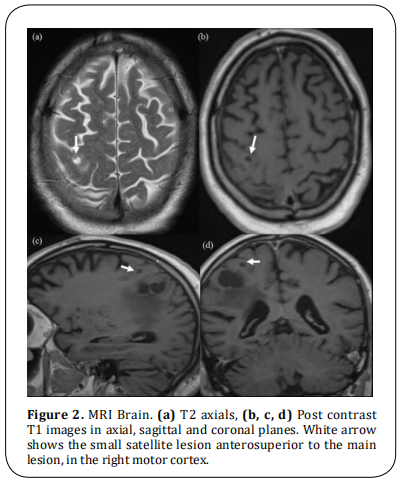
small satellite lesion was also noted just anteriorly in
the vincinity, in motor cortex (Figure 2). The patient
underwent BrainLab guided craniotomy and resection
of the main lesion without complications, the smaller
satellite lesion was left in situ, due to location in the
highly eloquent area.
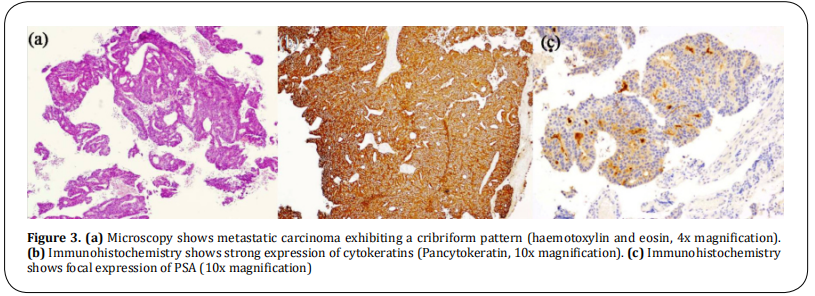
Histopathological analysis of the lesion reported a metastatic carcinoma with a cribriform pattern (Figure 3). The resected specimen expressed pancytokeratin with occasional cells expressing CK20. PSA showed focal expression, with evidence of prostein and focal PAP expression. There was no expression of CK7, p40, TTF1, CDX2 or PAX8. The specimen’s overall appearances and immunohistochemistry profile were consistent with a PCa primary.
A serum PSA level taken immediately post-op measured 6.8 ng/ml. In light of the past Finasteride use, the patient’s PSA level was corrected to at least 13.6 ng/ml (6.8 x 2) - considered beyond normal limits for a 73-year-old Caucasian male [normal reference range (0 - 6.5 ng/ml) for ages 70 to 79 years]. [7] Whole-body FDG PET scan was negative for bony metastases, repeat DRE denoted a small, smooth feeling prostate. A subsequent multiparametric MR imaging (mpMRI) of the prostate confirmed presence of a solitary 11mm highly likely (PI-RADS 5) peripheral zone cancer with early extracapsular extension (4mm) but again, no evidence of regional metastasis (Figure 4). Following Urology consultation, the patient proceeded to have Degarelix hormone injections repeated every 28 days. Docetaxel chemotherapy was considered, but not commenced due to the patient’s overall poor performance status.

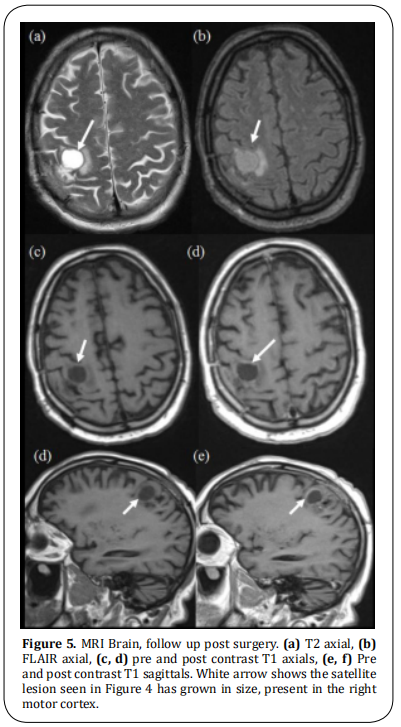
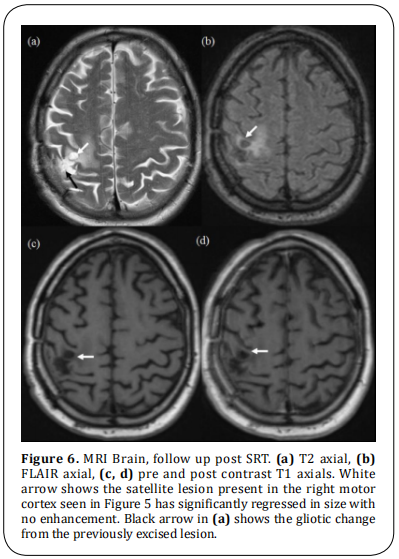
Six months post craniotomy, the patient experienced localised seizures. Interval MR imaging demonstrated progression of the satellite (cerebral) lesion (Figure 5). Due to presence in eloquent area, no further surgery was performed but the patient had stereotactic radiotherapy (SRT) delivered to his brain. At the time of writing, the patient remains well with significant improvement in appearances on follow up MR imaging (Figure 6) and undetectable PSA one-year post craniotomy.
Discussion
Cerebral metastases of unknown origin are an important clinical problem. Once detected by either head CT
or MRI, a CT CAP is usually performed to try to detect
the site of primary cancer, however, it is emphasised
that CT is quite insensitive in detecting cancers in certain organs, including prostate, thus there is limited
utility of a CT scan for this purpose. A FDG PET-CT may
also be performed, which however is not sensitive for
small lesions or certain cancer types. In the future, tailored-imaging approach may needed for organs where
significant progress has taken place in the detection
and characterisation of primary cancers. Prostate cancer is an example where pre-biopsy mpMRI has now
an established role in the diagnostic pathway.
There is currently no active screening programme for
PCa in the UK. The symptoms of PCa are relatively non specific, mainly related to lower urinary tract, such
as urgency, frequency and nocturia, that overlap with
presentation of benign prostatic hyperplasia. Clinical suspicion for PCa arises with an increase in serum
prostate-specific antigen (PSA) levels or detected abnormality on digital rectal examination (DRE), which
can be negative particularly with anterior prostate
lesions, notably, repeat DRE following histological diagnosis in this case was also unremarkable, thus, reiterating that a normal examination cannot rule out PCa.
If clinical assessment of the prostate using a combination of blood PSA levels and a DRE is negative, no
routine imaging for prostate is performed. Thus it is
possible, that some of the potential cases of PCa, with
isolated cerebral metastases, with relatively low PSA
levels, may remain undiagnosed, unless resection or
biopsy of the brain lesion is performed.
The spectrum of PCa behaviour is widely variable,
ranging from asymptomatic, microscopic tumour to
much rarer, symptomatic high-grade cancer that causes
distant metastases, significant morbidity and death.
A recent Surveillance, Epidemiology and End Results
(SEER) program report from the National Cancer Institute (NCI) in the United States found that at the time
of diagnosis, 6% of all PCa patients have evidence of
distant metastases [7]. A population-based analysis of
distribution of metastatic sites in 74,826 patients with
PCa recorded that the most common metastatic sites
were bone (84%), distant lymph nodes (10.6%), liver
(10.2%), thorax (9.1%), brain (3.1%), and digestive
system (2.7%). Of all patients with a single metastatic
site involved (n= 61,095), bony metastases were the
most common (83%). Isolated brain metastases were
observed in only 1.0% of patients in this cohort. [8]
Specifically, common intracranial sites for PCa spread
include the leptomeninges, cerebrum and cerebellum,
in order of frequency [9]. It needs to be emphasised that
it may still represent a significant number, given the
high incidence of PCa [1, 2]. Isolated cerebral metastases
from undiagnosed PCa are considered very rare, only
a few case reports are present [10, 11]. It has been highlighted that isolated cerebral metastases may have low
or only slightly high PSA levels, since PSA levels are
often the highest with increased disease burden, particularly with skeletal metastases. The previous case
reports have not specified if any of those patients were
also on 5-ARI, which is further expected to reduce
PSA levels by about 50%. As in our patient, PSA levels
were relatively low and only slightly high even after
“adjustment”, while this should still have been an indication for MRI as per newer guidelines as discussed
below, this is still a message being absorbed by the
non- urologists, resulting in inability to diagnose preoperatively.
Traditional approach to diagnose PCa was, till recently, by using transrectal ultrasound-guided biopsy
(TRUSB). However, it is known to miss clinically significant cancers and to overdiagnose non-significant
disease leading to overtreatment. More recently, there
has been a fundamental change in this approach and
the new approach is to use mpMRI as a primary tool in
patients clinically suspected or at risk of having prostate cancer [6]. This is also reflected in recent changes
in NICE guidelines recommending upfront mpMRI in
the PCa diagnosis and management [12].
As noted from our case, the primary site of the suspected cerebral metastasis was investigated extensively with CT CAP, PET-CT, PSA levels and DRE. Almost
all of these were non contributory; however, PSA was
slightly raised (adjusted level of 13.6ng/ml), considering a normal level of upto 6.5ng/ml. Given that the
patient presented to neurosurgery, it was only after
the cerebral lesion was resected that a diagnosis was
made, an mpMRI was only performed later, subsequent
to urology referral. The resection itself was also suboptimal, since a satellite lesion was left, due to presence
in eloquent area, subsequently treated successfully
with radiotherapy. We argue that mpMRI, if performed
pre-operatively, may have led to earlier diagnosis and
SRT to brain metastasis could have been given at the
time of initial treatment, hence avoiding unnecessary
craniotomy, particularly in a disease where combination of hormones and radiotherapy are known to have
significant advantages. However, it could also be argued that an isolated.
Brain metastasis from this cancer being very rare, the
first hypothesis would still have been an occult pulmonary origin lesion such as large cell neuroendocrine
carcinomas, justifying the resection of the cerebral lesion, although the resection here was suboptimal due
to presence on eloquent area. Nonetheless, this case
highlights and reaffirms the importance of performing
mpMRI in such patients with potential for an early diagnosis.
We therefore suggest, that given the recent expansion of scope of mpMRI for diagnosis of PCa, and due
to its non invasive nature, mpMRI of prostate may be
included in the protocol for assessment of cerebral
metastasis from unknown primary in select group of
males, if CT CAP and/or PET-CT is non contributory, DRE is negative and PSA is slightly raised, since it can
make a diagnosis pre-operatively and potentially result
in change in treatment and delivering more appropriate treatment, which can otherwise be limited by presence of lesions in eloquent areas and patient’s clinical
status. As our experience with mpMRI grows due to recent change of practice [13], we may be able to perform
larger trials, use a tailored approach, taking patient
specific issues into account including risk factors with
more specific recommendations. It is also important
that the messaging of change in protocols regarding
mpMRI as the first line modality for suspected prostate
cancer is more widely conveyed, sensitising all clinicians and threshold for requesting it lowered.
Conclusion
We have described a rare case of isolated brain metastases of PCa with negative CT CAP, PET-CT, DRE with slightly raised PSA levels, suppressed by Finasteride use, that was resected, subsequently proven as PCa from histopathology and mpMRI. The lesion recurred due to presence of satellite lesion in eloquent area, subsequently successfully treated by SRT. This case highlights and reaffirms the role of mpMRI in patients with borderline and slightly raised PSA levels and the need to emphasise its increasingly important role in the early diagnosis of prostate cancer.
Declarations
Authors’ contributions
All authors made substantial contributions to merit inclusion as co-authors. Mustafa El Sheikh wrote the first draft, Avinash Kumar Kanodia and Magdalena Szewczyk-Bieda provided radiology contributions, William Gietzmann and Ghulam Nabi provided urology contribution and Heinke Pulhorna provided neurosurgical contributions. All authors participated in the research and approved the final manuscript.
Conflicts of interest
The author declares that there is no conflict of interest.
Ethical approval
Caldicott approval was taken.
Consent for publication
Patient consent obtained.
References
1. Cancer Today. (2019). Retrieved 18 April 2020. Available online: http://gco.iarc.fr/today/fact-sheets-cancers
2. The 10 Most Common Causes of Cancer Death in
Males.(2017). Cancer Research UK. Available online:
https://www.cancerresearchuk.org/health-professional/cancer-statistics/mortality/common-cancerscompared#heading-One
3. Cancer survival by stage at diagnosis for England. (2019).
Office for National Statistics. Available online: https://
www.ons.gov.uk/peoplepopulationandcommunity/
healthandsocialcare/conditionsanddiseases/bulletins/
cancersurvivalinengland/stageatdiagnosisandchildhoodpatientsfollowedupto2018
4. Tremont-Lukats, I. W., Bobustuc, G., Lagos, G. K., Lolas, K.,
Kyritsis, A. P., & Puduvalli, V. K. (2003). Brain metastasis
from prostate carcinoma: The MD Anderson Cancer Center experience. Cancer, 98(2), 363-368.
5. Hatzoglou, V., Patel, G. V., Morris, M. J., Curtis, K., Zhang,
Z., Shi, W., ... & Young, R. J. (2014). Brain metastases from
prostate cancer: an 11-year analysis in the MRI era with
emphasis on imaging characteristics, incidence, and
prognosis. Journal of Neuroimaging, 24(2), 161-166.
6. Faria, R., Soares, M. O., Spackman, E., Ahmed, H. U.,
Brown, L. C., Kaplan, R., ... & Sculpher, M. J. (2018). Optimising the diagnosis of prostate cancer in the era of
multiparametric magnetic resonance imaging: a costeffectiveness analysis based on the Prostate MR Imaging
Study (PROMIS). European urology, 73(1), 23-30.
7. Cancer of the Prostate - Cancer Stat Facts. (2020). Retrieved 18 April 2020. Available online: https://seer.
cancer.gov/statfacts/html/prost.html
8. Gandaglia, G., Abdollah, F., Schiffmann, J., Trudeau, V.,
Shariat, S. F., Kim, S. P., ... & Karakiewicz, P. I. (2014).
Distribution of metastatic sites in patients with prostate
cancer: a population-based analysis. The Prostate, 74(2),
210-216.
9. Sutton, M. A., Watkins, H. L., Green, L. K., & Kadmon, D.
(1996). Intracranial metastases as the first manifestation of prostate cancer. Urology, 48(5), 789-793.
10. Campagna, J. P., & Feia, K. (2018). Isolated brain metastasis of prostate carcinoma in the setting of normal prostate specific antigen. Urology case reports, 21, 67.
11. Hafiz, A., Karim, M. U., Qureshi, B. M., Jabbar, A. A., & Ahmad, Z. (2019). Solitary brain metastasis: A rare initial
presentation of prostate carcinoma. Cureus, 11(6).
12. Prostate cancer: diagnosis and management. (2020). National Institute for Health and Care Excellent. Retrieved
21 April 2020, Available online:https://www.nice.org.
uk/guidance/ng131.
13. Szewczyk-Bieda, M., Wei, C., Coll, K., Gandy, S., Donnan,
P., Ragupathy, S. K. A., ... & Nabi, G. (2019). A multicentre
parallel-group randomised trial assessing multiparametric MRI characterisation and image-guided biopsy
of prostate in men suspected of having prostate cancer:
MULTIPROS study protocol. Trials, 20(1), 638.