Open Access | Letter to Editor
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Transjugular intrahepatic portosystemic shunt in Budd-Chiari syndrome
*Corresponding author: Sajad Ahmad Salat
Mailing address: Associate Professor of Surgery, The Unaizah
College of Medicine and Applied Medical Sciences, Qassim University, KSA.
Email: docsajad@yahoo.co.in
Received: 20 July 2020 / Accepted: 26 August 2020
DOI: 10.31491/CSRC.2020.09.061
Dear Sir
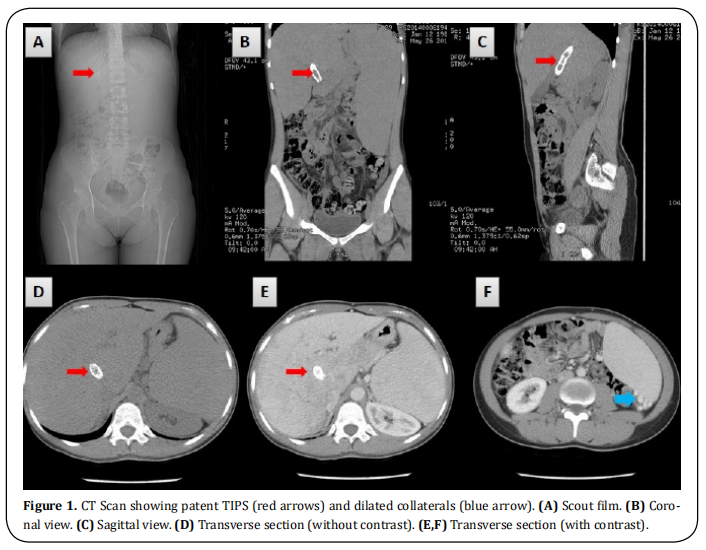
A 29-year-old female who was a known case of primary Budd–Chiari Syndrome (BCS) reported with nonspecific abdominal discomfort. She had a history of multiple variceal bleeds and had undergone placement of a transjugular intrahepatic porto-systemic shunt (TIPS) three months before this episode. She was on a follow-up regimen at a regional tertiary care center for hepatic disorders. The patient was managed conservatively because the hemodynamic and laboratory parameters were within acceptable limits. Imaging was conducted to study the status and patency of the shunt. A multiaxial CT scan of the abdomen and pelvis with oral and intravenous contrast (Figure 1: A–F) showed a heterogeneous liver and a patent TIPS stent communicating the porto-venous and systemic system. The portal vein was distended with multiple collater als. There was neither ascites nor splenomegaly (spleen size: 26 cm). The rest of the study was unremarkable.
Budd–Chiari syndrome (BCS) is a very rare condition,
affecting one in one million adults. BCS is named after
George Budd, a British internist, and Hans Chiari, an
Austrian pathologist. BCS affects younger to middleaged patients with a mean age of 40 years. The condition is caused by an occlusion of the hepatic venous
outflow at any level from the small hepatic veins to the
atriocaval junction [1]. The obstruction may be thrombotic or non-thrombotic. BCS is classified as primary
(75%) or secondary (25%) depending on the origin
of the obstructive lesion. If the obstruction results
from endoluminal venous lesion-like thrombosis, it is
termed primary BCS. However, if the cause originates
from neighboring structures, such as extrinsic compression or tumor invasion, it is referred to as secondary BCS [2].
Two of the hepatic veins must be blocked to cause
clinically evident disease that presents with a classical triad of abdominal pain, ascites, and liver enlargement. The syndrome can be fulminant, acute, subacute,
chronic, or asymptomatic. Acute or sub-acute variants with diffuse occlusion of the hepatic veins still
have a high mortality rate and remain challenging to
treat clinically. The transjugular intrahepatic portosystemic shunt (TIPS) has been used in recent times
successfully and safely in selected patients of BCS as
a definitive treatment or as successful bridge to liver
transplant [3, 4]. The most common indications for TIPS
in BCS patients include progressive liver failure, refractory ascites, recurrent variceal bleeding, and diffuse
hepatic vein thrombosis, and successful TIPS insertion
has been found to improve hemodynamic and clinical
parameters [5].
Insertion of a TIPS involves a technique that starts with
insertion of a 5 F multipurpose catheter into the hepatic vein. Angiography is performed, and the occlusion is
identified. A puncture needle is advanced into the portal vein through the liver parenchyma from the inferior
vena cava (IVC), and then the guide wire is placed into
the portal vein (PV) through the 10 F sheath. Portal
vein angiography is performed, and the portal vein
pressure and right atrium pressure are measured to
calculate the porto-systemic pressure gradient (PSG).
The TIPS shunt is dilated with an angioplasty balloon
of 8 or 10 mm in diameter, and then a covered stent
with a diameter of 8 or 10 mm is deployed [6]. In a recent study, Qi X. documented procedure-related complications in up to 56% of cases after TIPS insertion
and shunt dysfunction in 18–100% of cases. The shortand long-term prognosis of BCS-TIPS patients has
been found to be excellent, with a one-year cumulative
survival rate of 80–100% and a five-year cumulative
survival rate of 74–78% [5].
References
1. Horton, J. D. , Miguel, F. L. S. , & Ortiz, J. A. . (2010). Budd–
chiari syndrome: illustrated review of current management. Liver International, 28(4), 455-466.
2. Aydinli, M. , & Bayraktar, Y. . (2007). Budd-chiari syndrome: etiology, pathogenesis and diagnosis. World J
Gastroenterol, 13(19), 2693.
3. Fox, M. A., Fox, J. A., & Davies, M. H. (2011). Budd-Chiari
syndrome--a review of the diagnosis and management.
Acute Medicine, 10(1), 5-9.
4. Olliff, S. P. (2006). Transjugular intrahepatic portosystemic shunt in the management of Budd Chiari syndrome. European journal of gastroenterology & hepatology, 18(11), 1151-1154.
5. Qi, X., Yang, M., Fan, D., & Han, G. (2013). Transjugular
intrahepatic portosystemic shunt in the treatment of
Budd–Chiari syndrome: a critical review of literatures.
Scandinavian journal of gastroenterology, 48(7), 771-
784.
6. He, F., Zhao, H., Dai, S., Wu, Y., Wang, L., Huang, H., ... &
Liu, F. (2016). Transjugular intrahepatic portosystemic
shunt for Budd–Chiari syndrome with diffuse occlusion
of hepatic veins. Scientific Reports, 6, 36380.