Open Access | Research Article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Sternal closure methods in high-risk patients: Should they be specifc to the patient?
*Corresponding author: Metn Onur Beyaz
Mailing address: Department of Cardiovascular Surgery, Faculty of
Medicine, Istanbul Medipol Mega University Hospita, TEM Avrupa
Otoyolu Goztepe Cikisi, No:1, 34214 Bagcilar, Istanbul, Turkey.
Email: metnonurbeyaz@gmail.com
Received: 19 July 2020 / Accepted: 10 September 2020
DOI: 10.31491/CSRC.2020.09.057
Abstract
Background: To analyze and investigate the most effective sternum closure method in high-risk patients
undergoing median sternotomy, we compared a steel wire-titanium hooks combination with a steel wiretitanium plates and screws combination.
Patients and Methods: We examined 67 patients who underwent median sternotomy between October 2018
and January 2020. Patients who needed postoperative chemotherapy or radiotherapy due to malignancy were
excluded from the study. The patients were randomly divided into two groups with similar risk factors. In the
first group, a steel wire–titanium hooks combination was used to close the sternum. A steel wire–titanium
plates and screws combination was used in the second group of patients.
Results: No dehiscence or mediastinitis were observed in either patient group. Superficial wound infection
was seen in four patients from each group and was successfully treated with antibiotic therapy. There was no
significant difference between the two groups regarding the intensive care stay, the duration of hospitalization,
the amount of bleeding or the need for re-exploration (p > 0.05).
Conclusion: The choice between sternal closure techniques in high-risk patients should be mainly based on
the characteristics of the patient. Beyond this, the most cost-effective method in which the surgeon is most
experienced should be preferred.
Keywords
Titanium hooks; titanium plates and screws; tersonalized sternal closure methods
Introduction
Cardiovascular surgeons have not abandoned costeffective steel wire choices for sternum closure [1]. Sternal dehiscence is the riskiest complication that can occur after a median sternotomy [2]. Elderly age, osteoporosis, diabetes mellitus, obesity (BMI> 30), and female gender are risk factors for dehiscence [3]. Techniques such as the Robicsek procedure are available for patients at risk. However, the application of any method involving the use of steel wire is still controversial in high-risk patients [4,5]. With advances in technology, classical sternal closure methods have been replaced by new techniques using titanium plates, titanium hooks [Talon], thermoreactive nitinol clips, flat wire sternal closure systems, plastic materials and titanium cables [6,7]. These new sternal closure methods have high costs compared to steel wire. They also extend the operation time and are difficult to implement. Nevertheless, many surgeons prefer new methods over the use of steel wire in patients at risk of dehiscence [8,9]. We compared a steel wire–titanium hooks combination with a steel wire–titanium plates and screws combination to investigate the most effective sternum closure method in high-risk patients undergoing median sternotomy.
Patients and Methods
Materials and methods
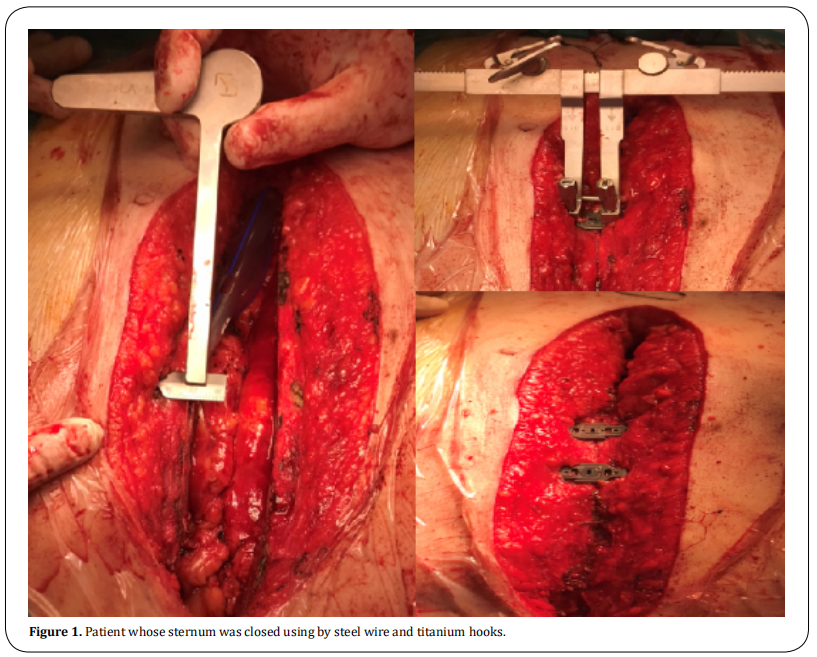
We examined 67 patients due to undergo median sternotomy between October 2018 and January 2020. Patients who needed postoperative chemotherapy or radiotherapy due to malignancy were excluded from the study. The patients were randomly divided into two groups with similar risk factors. In the first group, a steel wire–titanium hooks combination was used to close the sternum. A steel wire–titanium plates and screws combination was used in the second group of patients. Some of the patients included in the study underwent heart valve surgery, while others underwent coronary artery bypass grafting (CABG) surgery. Bilateral internal mammarian artery (IMA) grafting was not used in any of the patients who underwent CABG. We prepared LIMA or RIMA as classic pedicled grafts for patients who required them. The cautery dose did not exceed 20 degrees. We closed the skin with Prolene suture in all patients.
Statistical analysis
Statistical analysis was performed with the SPSS version 24.0 program (SPSS Inc. Chicago IL, USA). The normal distribution of the variables was examined by histogram graphs and the Kolmogorov–Smirnov test. Mean ± standard deviation values were used to present the descriptive analyses. The Pearson’s chi-square and Fisher’s exact tests were compared using 2x2 tables. Since normally distributed (parametric) variables were evaluated in both groups, a Student’s T-test was used. The Mann–Whitney U test was used to evaluate nonparametric variables. Logistic regression tests were performed to obtain the odds ratios. Statistically significant results were determined as P-values below 0.05.
Results
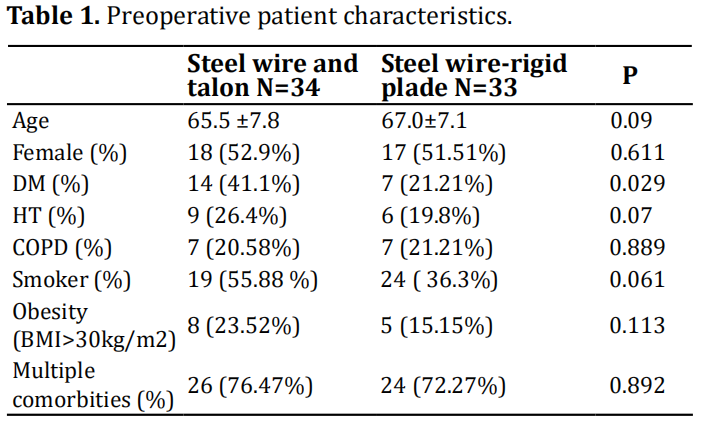
The patients were divided into two groups. In the first
group, the sternum was closed using a steel wire–titanium hooks combination (Yaylamed Inc). The mean age of the patients was 65.5 ±7.8 (min 62–max 73.2),
and 18 of the patients (52.9%) were women. Diabetes
mellitus was present in 14 patients (41.1%) (HbA1c:
7.72±0.9%), hypertension in 9 (26.4%), and chronic
obstructive pulmonary disease (COPD) in 7 (20.58%)
(with FEV1<80% and FEV1/FVC<70% with spirometry); 19 (55.88%) patients were smokers (more than
10 pack-years), 8 (23.52%) were obese (BMI>30 kg/
m2), and 26 (76.47%) had multiple comorbidity included osteoporosis.
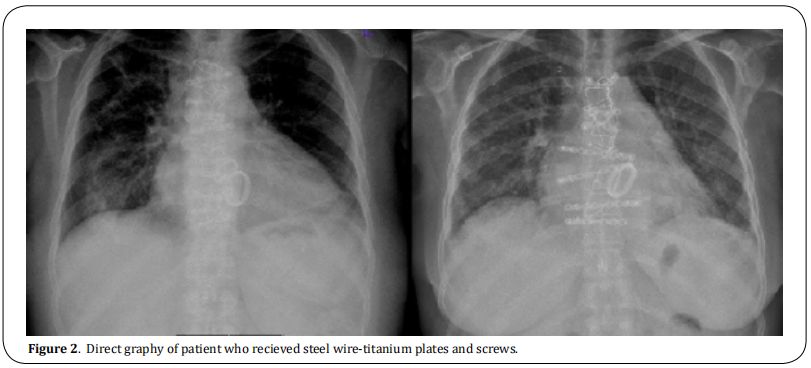
In the second group, the sternum was closed using
steel wires and titanium plates and screws. The average age was recorded as 67 ± 7.1 (min 57–max 74.2),
and 17 (51.51%) of the patients were women. Diabetes
mellitus was present in 7 patients (21.21%) (HbA1c:
7.1±1.3%), hypertension in 6 (19.8%), and COPD in 7
(21.21%) (FEV1<80% and FEV1/FVC<70% with spirometry); 24 (36.3%) patients were smokers (more
than 10 pack-years), 5 (15.15%) were obese (BMI>30
kg/m2), and 24 (72.27%) had multiple comorbidity
included osteoporosis.
All patients underwent standard median sternotomy,
and operations were performed under cardiopulmonary bypass (CPB) with aortic cross-clamp. Cephalosporin was used in all patients for surgical prophylaxis.
The skin, subcutaneous tissue, and sternum were
wiped with povidone-iodine in all patients while sternotomies were closed. A steel wire–titanium hooks
combination was used in the first group, and a steel
wire–sternal plates and screws combination was used
in the second group. In the first group, an appropriate
size device was selected by measuring the sternum
width from the intercostal space. In the second group,
the appropriate size device was selected by measuring
the depth of the sternum. Six to eight steel wires were
applied in both groups. Depending on the sternum
structure, two or three titanium hooks were placed in
the first group, and three or four titanium plates were
placed in the second group. Sternums were stabilized.
Subcutaneous tissues were closed individually with
2/0 vicryl, and skin was closed with 2/0 Prolene sutures.
All patients used a sternal corset for 8 weeks postoperatively. None of the patients had dehiscence or
needed re-exploration.
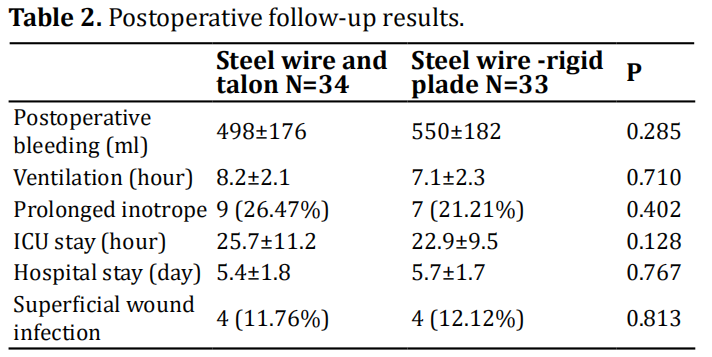
Postoperative drainage was 498±176 (390–830) cc
in the first group and 550±182 (400–800) cc in the
second group. There was no significant difference between the groups in terms of postoperative bleeding
amount (p > 0.05, P = 0.285).
The postoperative mechanical ventilation requirement
of the patients was 8.2±2.1 (3.9–12.1) hours for the
first group and 9.1±2.3 (4.3–11.4) hours for the second
group. There was no significant difference between the two groups (p > 0.05, P = 0.710).
Prolonged inotrope was needed in nine (26.47%)
patients from the first group and in seven (21.21%)
patients from the second group. No significant difference was found between the two groups (p > 0.05, P =
0.402).
The postoperative intensive care hospitalization time
was 25.7±11.2 (22.1–47) hours for the first group and
22.9±9.5 (19–48.5) hours for the second group. No significant difference was found between the two groups
(p > 0.05, P = 0.128).
The average length of hospital stay was 5.4±1.8 (5–8.8)
days for the first group and 5.7±1.7 (5.1–9) days for
the second group. There was no significant difference
between the two groups (p > 0.05, P = 0.767).
Superficial tissue infection appeared in four (11.76%)
patients from the first group and in four (12.12%)
patients from the second group. There was no significant difference between the two groups (p > 0.05, P =
0.813). Staphylococcus aureus was considered to be
the cause of the superficial tissue infections; empirical antibiotic therapy was applied, and wounds were
treated. No active microorganisms were found in the
control swab cultures. Neither sternal dehiscence nor
mediastinitis was observed in either group. Neither
aseptic dehiscence nor allergic reaction to the materials used developed in either group.
Discussion
The risk of dehiscence, which is 2.5% on average,
increases gradually due to increasing age, deterioration in eating habits, obesity, chronic lung diseases
and malignancies [3]. With technological advances,
new materials and techniques for sternal closure have
been developed to prevent dehiscence in patients with
these increased risks [10]. High-cost, difficult-to-apply,
but highly durable systems have been developed using materials such as titanium plates, titanium hooks,
thermoreactive nitinol clips, flat wire sternal closure systems, kryptonite bone glues, plastics, and titanium
cables [11].
Cardiovascular surgeons have to fight for different reasons in almost every patient have risk of dehiscence.
Sternal dehiscence may develop due to advanced age,
female gender, obesity, or osteoporotic bone structure [12]. Sudden cough crises increase intrathoracic
pressure in smokers and those with COPD. Increased
pressure may lead to the breaking of sternal bone
structures and the formation of dehiscence in patients
whose sternums are closed with traditional steel methods [13]. In our study, female sex was dominant in both
groups. In addition to gender, smoking, and diabetes
were common risk factors in the first group. In the second group, COPD was found at a rate equal to that of
diabetes.
The use of titanium plates is still controversial in the
presence of osteoporosis [14]. One study reported that
titanium hooks can be used, especially in patients at
risk of dehiscence. However, the possibility of intercostal arterial injury should be considered [15,16]. In our
study, no complication due to osteoporosis arose during screwing in the patient group in which steel wire
and titanium plates were combined. No dehiscence or
need for re-exploration were found in these patients.
A similar amount of drainage was required in both
groups. There was no need for revision due to bleeding, dehiscence, or mediastinitis in any patient in the
group where steel wire and titanium hooks were used.
Another cause of sternal dehiscence is metal susceptibility caused by hypersensitivity and allergic reaction
without exposure to microbial pathogens. Metal hypersensitivity reactions to nickel have been frequently
reported [17]. In our study, no material other than titanium and steel were used, and no allergic reaction was
observed in either group.
Limitation
Randomized studies in which all risk factors are evaluated are required to determine the best routine surgical technique to avoid sternal dehiscence.
Conclusion
The choice between sternal closure techniques in highrisk patients should be based mainly on the characteristics of the patient. Beyond this, the most cost-effective method in which the surgeon is most experienced should be preferred.
Declarations
Authors’ contributions
Made substantial contributions to conception and design of the study and performed data analysis and interpretation: Beyaz MO, Demir I, Erkanlı K. Performed data acquisition, as well as provided administrative, technical, and material support: Karakaya A, Ulukan MO.
Availability of Data and Materials
All data of the patients are stored at Medipol University where the operations are performed.
Conflicts of interest
The author declares that there is no conflict of interest.
Ethical disclosure
We studied in accordance with the ethical guidelines set by the Helsinki Declaration and the International Association of Heart and Lung Transplantation (ISHLT). A retrospective study was made by obtaining signed documents and approvals from all patients for procedures, including the approval of the use of patient data in future retrospective studies. 10840098-604.01.01- E.19387 numbered, 03/07/2020 dated ethics committee permission from Istanbul Medipol University is available for this study.
References
1. Losanoff, J. E., Jones, J. W., & Richman, B. W. (2002). Primary closure of median sternotomy: techniques and
principles. Cardiovascular Surgery, 10(2), 102-110.
2. Kamiya, H., Al-maisary, S. S., Akhyari, P., Ruhparwar, A.,
Kallenbach, K., Lichtenberg, A., & Karck, M. (2012). The
number of wires for sternal closure has a significant
influence on sternal complications in high-risk patients.
Interactive cardiovascular and thoracic surgery, 15(4),
665-670.
3. Molina, J. E., Lew, R. S. L., & Hyland, K. J. (2004). Postoperative sternal dehiscence in obese patients: incidence
and prevention. The Annals of thoracic surgery, 78(3),
912-917.
4. Robicsek, F., Daugherty, H. K., & Cook, J. W. (1977). The
prevention and treatment of sternum separation following open-heart surgery. The Journal of thoracic and cardiovascular surgery, 73(2), 267-268.
5. Takazawa K, Ishikawa N, Miyagawa H, Yamamoto T, &
Hariya. A. (2003). Artif Organları, 6 (1): 71-72.
6. Sharma, R., Puri, D., Panigrahi, B. P., & Virdi, I. S. (2004). A
modified parasternal wire technique for prevention and treatment of sternal dehiscence. The Annals of thoracic
surgery, 77(1), 210-213.
7. Cataneo, D. C., Dos Reis, T. A., Felisberto Jr, G., Rodrigues,
O. R., & Cataneo, A. J. (2019). New sternal closure methods versus the standard closure method: systematic review and meta-analysis. Interactive cardiovascular and
thoracic surgery, 28(3), 432-440.
8. Pai, S., Gunja, N. J., Dupak, E. L., McMahon, N. L., Coburn,
J. C., Lalikos, J. F., ... & Billiar, K. L. (2007). A mechanical
study of rigid plate configurations for sternal fixation.
Annals of Biomedical Engineering, 35(5), 808-816.
9. Snyder, C. W., Graham, L. A., Byers, R. E., & Holman, W.
L. (2009). Primary sternal plating to prevent sternal
wound complications after cardiac surgery: early experience and patterns of failure. Interactive cardiovascular
and thoracic surgery, 9(5), 763-766.
10. Raman, J., Lehmann, S., Zehr, K., De Guzman, B. J., Aklog,
L., Garrett, H. E., ... & Wong, M. S. (2012). Sternal closure
with rigid plate fixation versus wire closure: a randomized controlled multicenter trial. The Annals of thoracic
surgery, 94(6), 1854-1861.
11. Tewarie, L. S., Menon, A. K., Hatam, N., Amerini, A., Moza,
A. K., Autschbach, R., & Goetzenich, A. (2012). Prevention of sternal dehiscence with the Sternum External
Fixation (Stern-E-Fix) corset–a randomized trial in 750
patients. Journal of cardiothoracic surgery, 7(1), 1-8.
12. Schimmer, C., Reents, W., & Elert, O. (2006). Primary
closure of median sternotomy: a survey of all German
surgical heart centers and a review of the literature
concerning sternal closure technique. The Thoracic and
cardiovascular surgeon, 54(06), 408-413.
13. Celik, S., Kirbas, A., Gurer, O., Yildiz, Y., & Isik, O. (2011).
Sternal dehiscence in patients with moderate and severe
chronic obstructive pulmonary disease undergoing cardiac surgery: the value of supportive thorax vests. The
Journal of Thoracic and Cardiovascular Surgery, 141(6),
1398-1402.
14. Lazar, H. L., Salm, T. V., Engelman, R., Orgill, D., & Gordon,
S. (2016). Prevention and management of sternal wound
infections. The Journal of thoracic and cardiovascular
surgery, 152(4), 962.
15. Bennett-Guerrero, E., Phillips-Bute, B., Waweru, P. M.,
Gaca, J. G., Spann, J. C., & Milano, C. A. (2011). Pilot study
of sternal plating for primary closure of the sternum in
cardiac surgical patients. Innovations, 6(6), 382-388.
16. Savage, E. B. (2017). Is rigid sternal fixation really better? Was the correct control group used?. The Journal
of Thoracic and Cardiovascular Surgery, 154(6), 2003-
2004.
17. ATA, E. C., & BOYLU, B. B. (2018). Sternal Steel Wire
Induced Persistant Intermittan Mediastinal Wound
Drainage After CABG. Türkiye Klinikleri Journal of Case
Reports, 26(2), 98-101.