Open Access | Research Article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Peritonitis in Children: Experience in a Tertiary Hospital in Enugu, Nigeria
*Corresponding author: Chukwubuike Kevin Emeka
Mailing address: Department of Surgery, Enugu State University
Teaching Hospital, Enugu, Nigeria.
Email: chukwubuikeonline@yahoo.com
Received: 29 June 2020 / Accepted: 29 July 2020
DOI: 10.31491/CSRC.2020.09.056
Abstract
Background: Peritonitis may be associated with significant morbidity and mortality. The aim of this study was
to evaluate our experience with the management of secondary peritonitis in children.
Methods: This was a retrospective study of children who had undergone laparotomy for peritonitis in the pediatric surgery unit of Enugu State University Teaching Hospital (ESUTH) in Enugu, Nigeria over a five-year
period.
Results: There were 52 cases of laparotomies for peritonitis, with an age range of two weeks to 14 years (median: nine years) and a male to female ratio of 3.3:1. The etiologies of peritonitis were typhoid intestinal perforation in 25 cases (48%), ruptured appendix in nine cases (17.3%), perforated intussusception in eight cases
(15.4%), perforated external hernia in three cases (5.8%), perforation due to adhesive intestinal obstruction
in three cases (5.8%), perforated necrotizing enterocolitis in three cases (5.8%), and bowel perforation due to
trauma in one case (1.9%). The following definitive surgical procedures were performed: closure of bowel perforation in 26 cases (50%), appendectomy plus abscess drainage in nine cases (17.3%), right hemicolectomy
with ileotransverse anastomosis in eight cases (15.4%), segmental bowel resection in six cases (11.5%), and
insertion of peritoneal drains in three cases (5.8%). The median duration of symptoms prior to presentation
and the median duration from presentation to surgery were four days and two days, respectively. Twenty-four
patients (46.2%) developed complications that included surgical site infection in 12 cases (23.1%), enterocutanous fistula in five cases (9.6%), intra-abdominal abscess in four cases (7.7%), and wound dehiscence in
three cases (5.8%). There were seven deaths, accounting for 13.5% of the patients.
Conclusion: Typhoid intestinal perforation was the most common cause of peritonitis in the present study.
Keywords
Children; peritonitis; developing country; single center
Introduction
Peritonitis can be defined as inflammation of the
peritoneum regardless of its etiology, and it is a potentially life-threatening pathology [1]. Other terms
synonymously used for peritonitis, but which are not
exactly the same, include intra-abdominal infection or intra-abdominal sepsis [1]. Peritonitis may be caused by
perforation of the bowel or hollow viscus, as can occur
with a ruptured appendix. Other causes of peritonitis
include but are not limited to anastomotic leak and
translocation of bacteria [1]. Peritonitis may be classified into primary, secondary, and tertiary peritonitis
based on the source and nature of the microbial contamination [2]. Peritonitis may also be classified into
localized or diffuse peritonitis.
In 1926, Kirschner demonstrated that by following
strict surgical principles, the mortality rate of peritonitis could be reduced from 80% to about 60% [3]. Subsequently, the development of new operative techniques,
the provision of potent antibiotics, and the availability
of intensive care treatment have reduced the mortality of peritonitis to an average of 30% to 40% [4]. The factors that affect the outcome of peritonitis are related
to the patient, the disease, and the intervention [5]. The
goal of this study was to evaluate the profiles and management outcomes of children treated for secondary
peritonitis at a tertiary hospital in Enugu, Nigeria.
Methods
This was a retrospective study of children aged 15
years and below who were managed for peritonitis
between January 2014 and December 2018 in the pediatric surgery unit of Enugu State University Teaching
Hospital (ESUTH) in Enugu, Nigeria. Patients who had
surgery for peritonitis at a peripheral hospital before
referral to ESUTH for reoperation were excluded from
the study, as were patients with primary peritonitis.
ESUTH is a tertiary hospital located in Enugu, South
East Nigeria. The hospital serves the entirety of Enugu
State, which, according to the 2016 estimates of the
National Population Commission and the Nigerian National Bureau of Statistics, has a population of about
four million and a population density of 616.0/km2.
The hospital also receives referrals from its neighboring states.
Information was extracted from the case notes, operation notes, operation register, and admission-discharge
records. The information extracted included age, gender, presenting symptoms, duration of symptoms before presentation, time interval between presentation
and intervention, intra-operative finding, definitive operative procedure performed, complications of treatment, duration of hospital stay, and outcome of treatment. The diagnoses of peritonitis were made based
on clinical and radiological findings. The follow-up
period was 12 months. Ethical approval was obtained
from the ethics and research committee of ESUTH,
and informed consent was obtained from the patients’
caregivers. Statistical Package for Social Science (SPSS)
version 21 (manufactured by IBM Corporation, Chicago, Illinois) was used for data entry and analysis. Data
were expressed as percentages, medians, means, and
ranges.
Results
Patients’ demographics
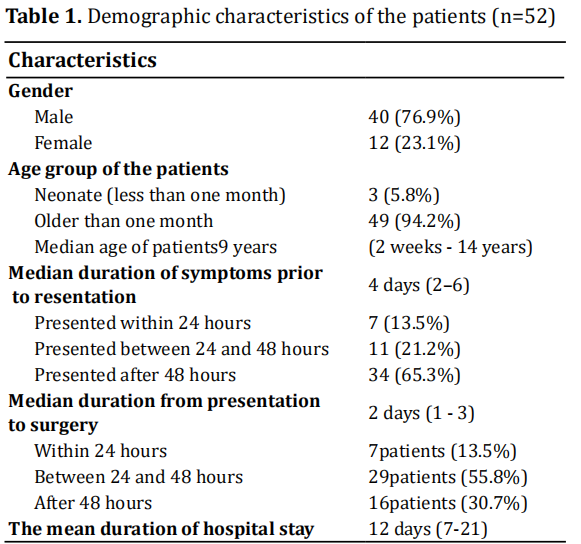
Sixty-two laparotomies were performed for peritonitis during the study period, but only 52 cases had complete case records; these formed the basis of this report. There were 40 males (76.9%) and 12 females (23.1%), which corresponds to a male to female ratio of 3.3:1. Details are depicted in Table 1.
Clinical features
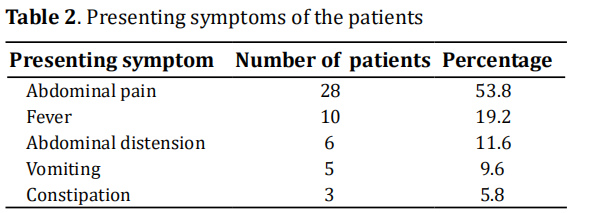
Presenting symptoms Presenting symptoms are shown in Table 2.
Clinical signs Fifty-two patients (96.2%) had generalized abdominal tenderness, and 48 patients (92.3%) had abdominal rigidity with guarding. On digital rectal examination, 26 patients (50%) had collections in the rectovesical pouch.
Radiological findings
All the patients had plain abdominal radiographs; the radiographs were diagnostic in five patients (9.6%). Forty-seven patients (90.4%) had abdominal ultrasound, out of which 26 (55.3%) showed echo-rich peritoneal fluid. Computed tomography scans were not performed as they were not available at the facility.
Etiology of peritonitis
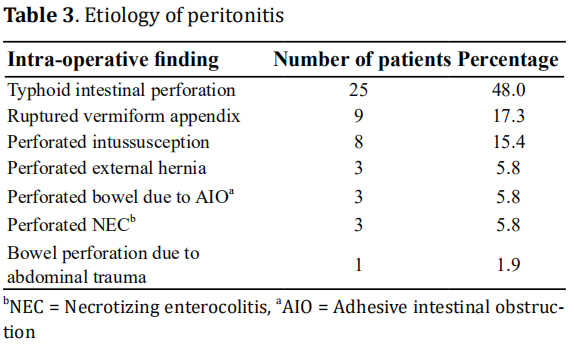
Based on the intra-operative findings, the most common etiology causing peritonitis was typhoid intestinal perforation. Others are shown in Table3.
Definitive operation performed
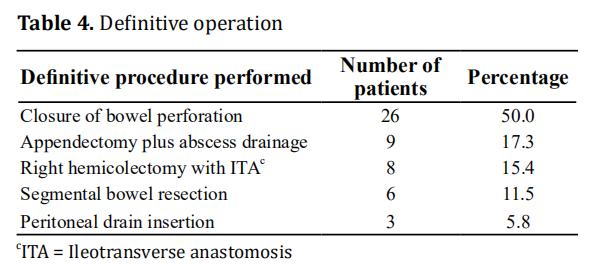
The definitive surgeries are shown in Table 4.
Post-operative complications
Twenty-eight patients (53.8%) did not develop any complications. Surgical site infection occurred in 12 patients (23.1%), and this was the most common complication recorded for the patients. Other complications included enterocutanous fistula in five cases (9.6%), intra-abdominal abscess in four cases (7.7%), and wound dehiscence in three cases (5.8%).
Outcome
Forty-two patients (80.8%) recovered well and were discharged. Two patients (3.8%) were signed out against medical advice. Mortality was recorded in seven patients (13.5%). Most mortality occurred among the neonates.
Follow-up
During the 12-month follow-up period, two patients (3.8%) developed adhesive bowel obstruction. These two patients recovered upon non-operative treatment of their adhesive bowel obstruction.
Discussion
Secondary peritonitis is a common emergency surgical
condition managed by surgeons all over the world, and
it represents a major cause of morbidity and mortality [6]. Secondary peritonitis results from the loss of integrity of the gastrointestinal tract, which leads to
contamination of the peritoneal cavity by endogenous
microflora [6]. Despite antimicrobial therapy, surgical
intervention is the cornerstone of treatment for secondary peritonitis [7].
In the present study, the male dominance of cases is
consistent with the reports of other studies on secondary peritonitis [8, 9, 10]. However, Fowler reported
a female dominance with regards to primary peritonitis [11]. The reason for this gender difference is not
known. The median age of our patients of nine years
is also similar to the reports of other studies [12, 13]. The
published median ages of patients with peritonitis
vary from five to 11.8 years [10, 14, 15]. The median age
of patients with peritonitis may be dependent on the
predominant pathology in a particular setting. For instance, typhoid intestinal perforation occurs more in
older children and intussusception is more common in
infants. Further, for the patients in this study, there was
a four-day median period before presentation to the
hospital, and this finding is consistent with the reports
of other studies [16, 17, 18]. This late presentation could
be due to the poverty and ignorance that is prevalent
in developing countries. Delays in investigating the
patients and a paucity of funds may have accounted for
the 48-hour lag period before surgery. The length of
hospital stay of our patients was similar to that in the
study conducted by Osifo et al. [10]. However, Obinwa
reported a median hospitalization period of six days [12].
The length of hospital stay may be determined by the
etiology of the peritonitis and the age of the patients.
For instance, neonates who have peritonitis generally
have longer hospital stays than older children [10].
Abdominal pain, which was the predominant symptom in the present study, was also the most common
symptom in other studies [9, 17, 18]. The symptoms of
abdominal pain, fever, abdominal distension, vomiting, and constipation seen in our patients are similar
to those reported by Nuhu et al. [17]. Typhoid intestinal
perforation is one of the most dreaded and common
complications of typhoid fever [19]. Typhoid intestinal
perforation is observed in 0.8% to 39% of cases of
typhoid fever [20], and it is the most common cause of
peritonitis, especially in developing countries [17]. The
findings of the present study are consistent with this
fact. However, other studies have reported that a ruptured appendix is the most common cause of secondary peritonitis in children [10, 12].
The definitive procedure performed on our patients
was dependent on the etiology of the peritonitis. Excision of the edge of the intestinal perforation and
simple transverse closure in two layers was the most
common procedure in our patients. A study conducted
in Tanzania also adopted this method of treatment for
typhoid intestinal perforation [21]. However, segmental
ileal resection with primary end-to-end anastomosis
for typhoid intestinal perforation is another option for
treatment [22, 23]. Laparotomy following peritonitis is
froth with many post-operative complications. Surgical
site infection, which we recorded as the most common
complication, has also been consistently observed by
other researchers [5, 9, 17]. Enterocutanous fistula is a
potentially catastrophic post-operative complication
and was recorded in about one tenth of our patients.
This is similar to the findings reported by Nuhu et al. [17].
However, a study conducted in Benin, Nigeria reported
no incidence of enterocutanous fistula following surgery for peritonitis [10]. Thus, the development of an
enterocutanous fistula after laparotomy may depend
on the primary pathology or modality of treatment.
The mortality rate of 13.5% in the present study is
comparable to the rates reported by other researchers [5, 9, 18]. However, the published mortality rates of
secondary peritonitis range from 8.8% to 26.1% [5]. In
the present study, the most common cause of mortality
was overwhelming sepsis due to late presentation and
complications arising from the surgery itself. The age
of the patient, degree of peritoneal contamination, and
duration of surgery are some factors that may affect
mortality in children who have peritonitis [5].
Strength of the study
Treatment of peritonitis in children that developed from a wide range of causes was discussed in this study. Data on pediatric peritonitis, unlike adult peritonitis, is not readily available, especially in developing countries.
Weakness/limitations of the study
This was a retrospective study; a prospective study would have provided more information for analysis. The generalizability of this study was also limited by the small number of cases that was considered. Further, this was a single institution experience that may not be generalizable to other institutions.
Conclusion
In the present study, the demographics, clinical features, radiological features, etiologies, surgical procedures performed, post-operative complications, and management outcomes of children with peritonitis were evaluated. Typhoid intestinal perforation was the most common etiology of peritonitis, and closure of bowel perforation was the most frequently performed surgical procedure. The current state of late presentation and poor outcome should be improved upon.
Declarations
Authors’ contributions
The author contributed solely to this article.
Availability of Data and Materials
Data is available with the author and can be provided on request.
Conflicts of interest
The author declares that there is no conflict of interest.
Ethical approval
Ethical approval was obtained from the hospital ethics committee.
References
1. Tochie, J. N., Agbor, N. V., Frank, T. L., Mbonda, A., Aji, D. A.,
& Danwang, C. (2020). Global epidemiology of acute generalised peritonitis: a protocol for a systematic review
and meta-analysis. BMJ open, 10(1), e034326-e034326.
2. Ross, J. T., Matthay, M. A., & Harris, H. W. (2018). Secondary peritonitis: principles of diagnosis and intervention.
BMJ (Clinical Research ed.), 361, k1407-k1407.
3. Jaiswal, S., & Sharma, S. C. (2020). Role of peritoneal
drainage in moribund patients of perforation peritonitis.
International Surgery Journal, 7(5), 1357-1360.
4. Holzheimer, R. G. (2001). Management of secondary
peritonitis. In Surgical Treatment: Evidence-Based and
Problem-Oriented. Zuckschwerdt.
5. Ayandipo, O. O., Afuwape, O. O., Irabor, D. O., Abdurrazzaaq, A. I., & Nwafulume, N. A. (2016). Outcome of
laparotomy for peritonitis in 302 consecutive patients
in Ibadan, Nigeria. Annals of Ibadan postgraduate medicine, 14(1), 30-34.
6. Sartelli, M., Catena, F., Abu-Zidan, F. M., Ansaloni, L., Biffl,
W. L., Boermeester, M. A., ... & Di Saverio, S. (2017). Management of intra-abdominal infections: recommendations by the WSES 2016 consensus conference. World
Journal of Emergency Surgery, 12(1), 1-31.
7. Van Ruler, O., & Boermeester, M. A. (2016). Surgical treatment of secondary peritonitis: A continuing problem.
German version. Der Chirurg; Zeitschrift fur alle Gebiete
der operativen Medizen, 87(1), 13.
8. Axler, J. P., Toussaint, S., & Alouidor, J. (2020). Descriptive
and correlational study of of peritonitis in the surgical department of the State University Hospital of Haïti
(HUEH): A cross sectional study. International Journal of
Surgery Open,24,105-111.
9. Mabewa, A., Seni, J., Chalya, P. L., Mshana, S. E., & Gilyoma,
J. M. (2015). Etiology, treatment outcome and prognostic
factors among patients with secondary peritonitis at Bugando Medical Centre, Mwanza, Tanzania. World Journal
of Emergency Surgery, 10(1), 47.
10. Meena, L. N., Jain, S., & Bajiya, P. (2017). Gastrointestinal
perforation peritonitis in India: A study of 442 cases.
Saudi Surgical Journal, 5(3), 116.
11. Khilji, M. F. (2015). Primary Peritonitis—A Forgotten Entity. European journal of pediatric surgery reports, 3(1),
27.
12. Obinwa, O., Casidy, M., & Flynn, J. (2014). The microbiology of bacterial peritonitis due to appendicitis in children. Irish Journal of Medical Science (1971-), 183(4),
585-591.
13. Sethna, C. B., Bryant, K., Munshi, R., Warady, B. A., Richardson, T., Lawlor, J., ... & Neu, A. (2016). Risk factors
for and outcomes of catheter-associated peritonitis in
children: the SCOPE collaborative. Clinical Journal of the
American Society of Nephrology, 11(9), 1590-1596.
14. Chinchilla, J., Sebastián, K., Meléndez, R., Ramay, B., &
Lou-Meda, R. (2016). Risk Factors for Peritonitis in a Pediatric Dialysis Program in Guatemala, 2011–2014.
15. Sutherland, S. M., Alexander, S. R., Feneberg, R., Schaefer,
F., Warady, B. A., & International Pediatric Peritonitis
Registry (IPPR). (2010). Enterococcal peritonitis in children receiving chronic peritoneal dialysis. Nephrology
Dialysis Transplantation, 25(12), 4048-4054.
16. Doklestić, S. K., Bajec, D. D., Djukić, R. V., Bumbaširević,
V., Detanac, A. D., Detanac, S. D., ... & Karamarković, R. A.
(2014). Secondary peritonitis-evaluation of 204 cases
and literature review. Journal of medicine and life, 7(2),
132-138.
17. Ali, N., & Gali, B. M. (2010). Causes and treatment outcome of perforation peritonitis in north eastern Nigeria.
Surgical practice, 14(3), 92-96.
18. Chichom-Mefire, A., Fon, T. A., & Ngowe-Ngowe, M.
(2016). Which cause of diffuse peritonitis is the deadliest in the tropics? A retrospective analysis of 305 cases
from the South-West Region of Cameroon. World Journal
of Emergency Surgery, 11(1), 14.
19. Sharma, A. K., Sharma, R. K., Sharma, S. K., Sharma, A., &
Soni, D. (2013). Typhoid intestinal perforation: 24 perforations in one patient. Annals of medical and health
sciences research, 3(1a), 41-43.
20. Contini, S. (2017). Typhoid intestinal perforation in
developing countries: Still unavoidable deaths?. World
Journal of Gastroenterology, 23(11), 1925.
21. Chalya, P. L., Mabula, J. B., Koy, M., Kataraihya, J. B., Jaka,
H., Mshana, S. E., ... & Gilyoma, J. M. (2012). Typhoid intestinal perforations at a University teaching hospital
in Northwestern Tanzania: A surgical experience of 104
cases in a resource-limited setting. World journal of
emergency surgery, 7(1), 4.
22. Sheshe, A. A., Anyanwu, L. J. C., Mohammad, A. M., Muhammad, A. B., & Obaro, S. K. (2018). Typhoid intestinal
perforation: Analysis of the outcome of surgical treatment in Kano, Nigeria. Archives of Medicine and Health
Sciences, 6(1), 59.
23. Patel, A., Kelly, P., & Mulenga, M. (2019). Surgical management of typhoid ileum perforations: a systematic
review. Medical Journal of Zambia, 46(4), 349-356.