Open Access | Review
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Onlay versus sublay mesh repair of open ventral incisional hernia: A meta-analysis of randomized controlled trials
*Corresponding author: Mohamed Ali Chaouch
Mailing address: Department B of surgery, Charles Nicolle
Hospital, University Tunis El Manar, Tunis, Tunisia.
Email: Docmedalichaouch@gmail.com
Received: 07 March 2020 Accepted: 09 Apirl 2020
DOI: 10.31491/CSRC.2020.06.049
Abstract
Background: Incisional hernia treatment remains a major issue in abdominal wall surgery. Open onlay and
sublay mesh repair are the most frequently used procedures. This meta-analysis aimed to compare the two
techniques for open ventral incisional hernia repair in terms of wound infection, hematoma, seroma, and
recurrence.
Methods: A search in electronic databases for randomized controlled trials (RCTs) published up to September
30, 2019 was performed. Review Manager Version 5.3 was used for pooled estimates. The eligibility criteria
were as follows: RCTs comparing onlay mesh repairs performed according to Cheverel with sublay mesh
repairs performed according to Rives-Stoppa and Schumpelick and including patients aged 18 or older.
Results: Of 22 relevant articles, 7 RCTs involving a total of 954 patients (487 onlay and 466 sublay mesh
repairs) met the eligibility criteria. Sublay mesh repairs were found to require better results in terms of wound
infection (odds ratio [OR]: 2.33, 95% CI: 1.09–4.94, p = 0.03) and seroma (OR: 3.71, 95% CI: 2.26–6.09, p <
0.001). There was no significant difference between the two techniques in terms of hematoma (OR: 2.53, 95%
CI: 0.90–7.11, p = 0.08). Regarding recurrence, the forest plot showed no statistical difference (OR: 1.75, 95%
CI: 0.55–5.55, I2 = 54%, p = 0.34); however, heterogeneity was high (I2 = 54%), and meta-regression showed a
statistically significant difference in favor of sublay mesh repair.
Conclusions: This meta-analysis of RCTs shows that sublay mesh repair of open ventral incisional hernias is
superior to onlay repair. Sublay mesh repair should probably be the first choice, and onlay repair should be
reserved for more difficult cases, where sublay repair is not possible.
Keywords
Incisional hernia; onlay; sublay; recurrence; surgical site infection; wound complications; metaregression
Introduction
An incisional hernia may occur within two years of a
midline incision, with a rate ranging between 10% and
20% [1,2]. Incisional hernias are mainly caused by surgical errors during the closure of the abdominal wall. The
incidence is higher in patients with risk factors such as
obesity and steroid use [3]. Incisional hernias can impair patients’ quality of life and can be life-threatening in case
of strangulation. Mesh repair reduces the likelihood of
incisional hernia recurrence [4,5]. The two most frequently used procedures are onlay and sublay mesh repair [6].
These procedures have advantages such as significantly
reducing the likelihood of recurrence but also disadvantages such as chronic pain [6,7].
Some surgeons prefer onlay mesh repair to avoid extensive abdominal wall dissection, while others insist that
sublay repair remains the best mesh placement even for
incisional hernias. Onlay repair is known to be easier
and faster but has a slightly higher wound complication
rate [8]. Sublay repair is believed by many to carry a lower
recurrence risk. Incisional hernia recurrence and postoperative wound complications depend on the abdominal wall mesh site. Then, the best mesh location is still
debated among surgeons [9–11].
This meta-analysis aimed to compare open onlay with
sublay mesh repair of ventral incisional hernias in terms
of wound infection, hematoma, seroma, and recurrence.
Medthods
Electronic database searches
An extensive electronic search of the relevant literature, with no language restrictions, was performed on September 30, 2019, using the following databases: the Cochrane Library’s Controlled Trials Registry and Database of Systematic Reviews, PubMed/MEDLINE of the United States National Library of Medicine, National Institutes of Health, Excerpta Medica Database (Embase), Scopus, and Google Scholar. The keywords used were “onlay,” “sublay,” “retromuscular,” “preperitoneal,” “open,” “surgery,” “incisional hernia,” “abdominal wall,” “repair,” “retrorectus,” “prefascial,” “retrofascial,” “Rives-Stoppa,” and “mesh placement.” This meta-analysis was performed in accordance with the 2010 Preferred Reporting Items for Systematic Review and Meta-analysis guidelines [12].
Eligibility criteria
Studies. All randomized controlled trials (RCTs) reporting comparisons between onlay and sublay mesh repairs of ventral incisional hernias published in peer-reviewed journals were considered for the analysis. Non-randomized trials, non-comparative studies, editorials, letters to editors, review articles and case series (fewer than ten cases) were excluded. Participants. Adults (aged 18 or older) of either gender undergoing open onlay or sublay mesh repair of ventral incisional hernia were included. Interventions. The following surgical procedures were included: (1) Sublay mesh repair according to Rives-Stoppa [13] and Schumpelick [14], with the mesh placed in the retrorectus muscles (prefascial or preperitoneal and retrofascial space). (2) Onlay mesh repair according to Cheverel [15], with the mesh placed in the anterior rectus fascial after dissection of the fascia from the subcutaneous plane.
Outcome measures
The main outcome measure was recurrence. Secondary outcome measures were wound infection, seroma, and hematoma.
Data collection and analysis
Study selection. Two authors (MAC and MWD) independently reviewed all abstracts. The full texts of all
studies that met the inclusion criteria were retrieved.
Disagreements were resolved by discussion after consulting a third member of the review team (IB).
Assessment of the studies’ quality. All studies that met
the selection criteria were independently appraised by
two authors (MAC and MAD) according to the CONSORT
Statement [16].
Data extraction. Each author independently extracted
the data from each study. Disparities were settled after
discussion with two senior authors (MWD and CD).
Assessment of heterogeneity. We used Cochran’s Q test
to assess heterogeneity and the I² statistic to estimate
the degree of heterogeneity [17]. We used the Cochrane
Chi² test (Q-test) to assess heterogeneity and we calculated the variance TAU2, between studies and the I². An
I² between 0% and 50% was considered a low level and
between 51% and 100% a high level of heterogeneity [18]. Funnel plots were used to identify the studies responsible for heterogeneity.
Evaluation of effect size. For the meta-analysis, we
used Cochrane’s Review Manager statistical package
version 5.3.5 [19]. We selected the mean difference (MD)
as an effective measure for continuous data. For dichotomous variables, we calculated odds ratios (OR) with
95% confidence intervals (CI). We used the random-effects model and set the threshold of statistical significance at 0.05. When I2 was between 51% and 100%,
we tested for interactions between relevant factors and
effect size estimates. We performed meta-regression using the natural log (OR) as the dependent variable and
the explored factor as the independent variable [17], as
determined by the Comprehensive Meta-Analysis software. Meta-regression concerned interactions between
treatment effects and the main outcome measure of
recurrence. The covariate used was the global rate of
recurrence.
Results
Literature search results
We retrieved seven potentially relevant articles (Figure 1). They were published between 2010 and 2018 [8,20–25]. Sixteen studies were excluded for the following reasons: one study [26] was a prospective non-randomized trial, two [27,28] were descriptive studies, one was a meta-analysis [29], and twelve concerned onlay and sublay mesh repair of abdominal ventral hernias or included abdominal ventral hernias and abdominal ventral incisional hernias without subgroup analysis [30–41].
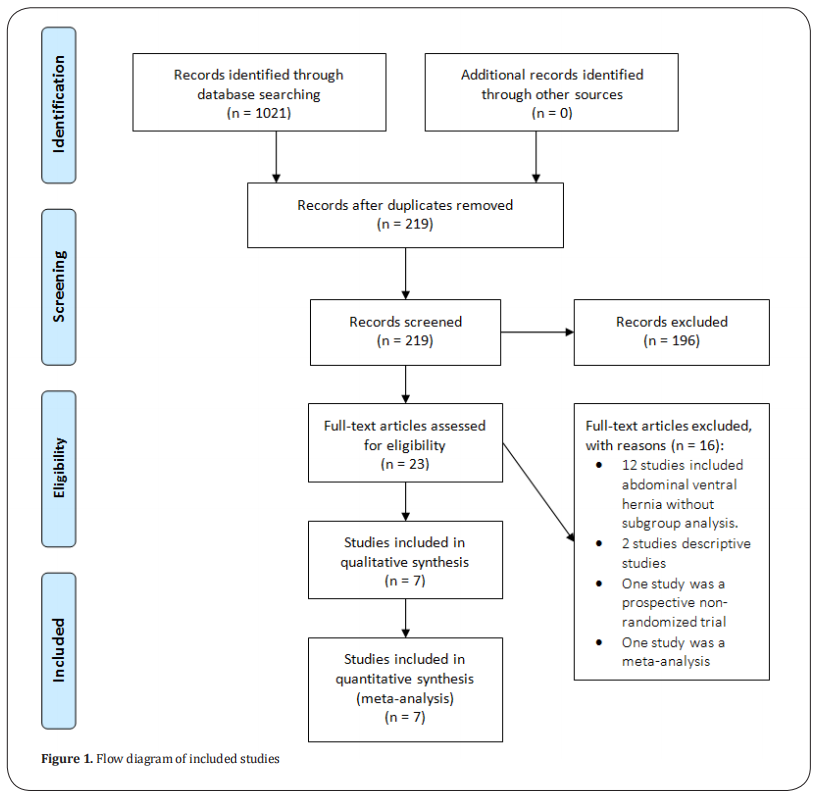
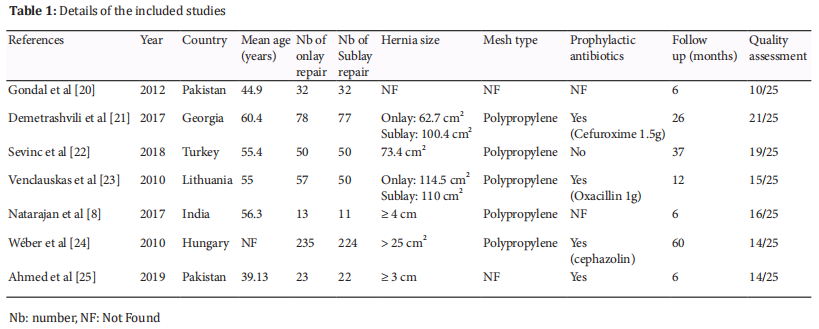
The seven identified studies involved a total of 954 patients (487 onlay and 466 sublay mesh repairs). They were fully matched in terms of year of publication, country, mean age, hernia size, mesh type, numbers of patients undergoing sublay and onlay mesh repairs, prophylactic antibiotic use, and follow-up duration. Six studies were published in English [8,20–23,25]and one in Hungarian [24]. The quality assessment and details of the included studies are summarized in Table 1.
Outcome measures
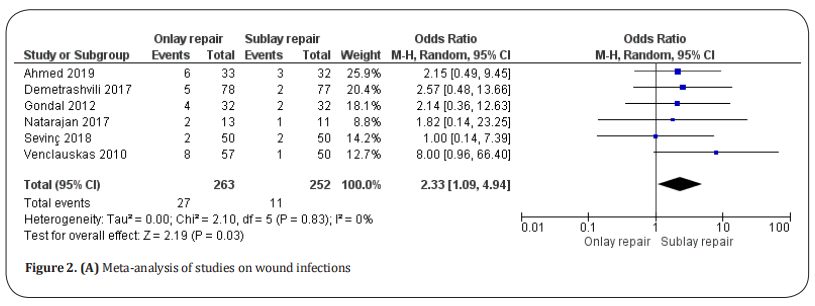
Wound infection. Wound infections were reported in six studies [8,20–23,25] (Figure 2.A), which included a total of 515 patients. They were detected in 27 of 263 patients undergoing onlay repair and 11 of 252 patients undergoing sublay repair. There was a significantly lower rate of wound infections in sublay repair patients (OR: 2.33, 95% CI: 1.09–4.94, p = 0.03] with no heterogeneity among the studies (Tau2 =0 and I2= 0%).
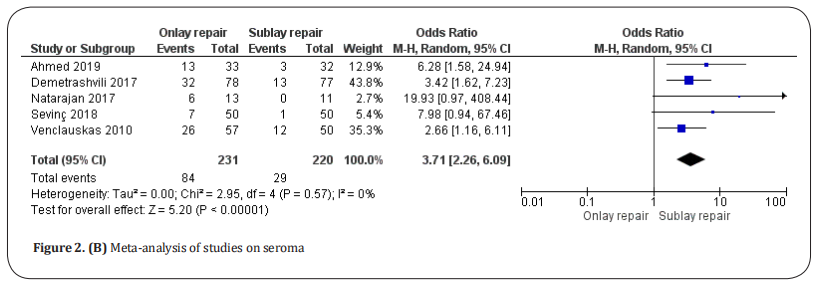
Seroma. Seromas were reported in five studies [8,21–23,25]
(Figure 2.B), which included a total of 451 patients. They
were detected in 84 of 231 patients undergoing onlay
repair and 29 of 220 patients undergoing sublay repair.
There was a significantly lower seroma rate in sublay repair patients (OR: 3.71, 95% CI: 2.26–6.09, p < 0.00001)
with no heterogeneity among the studies (Tau2 =0 and
I2 = 0%).
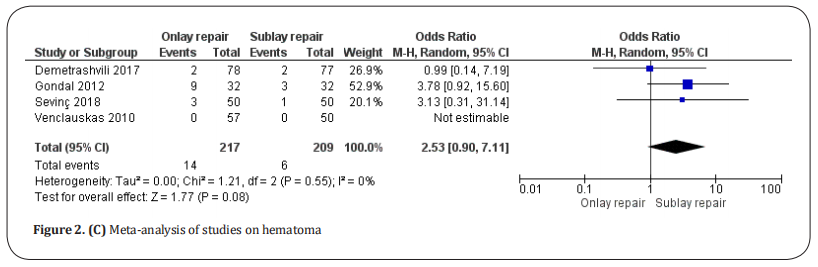
Hematoma. Hematomas were reported in four studies
[20–23], which included a total of 426 patients (Figure 2.C).
They were detected in 14 of 217 patients undergoing
onlay repair and 6 of 209 patients undergoing sublay repair. There was no statistical difference between the two
techniques (OR: 2.53, 95% CI: 0.90–7.11, p = 0.08) with
no heterogeneity among the studies (Tau2 =0 and I2 = 0%).
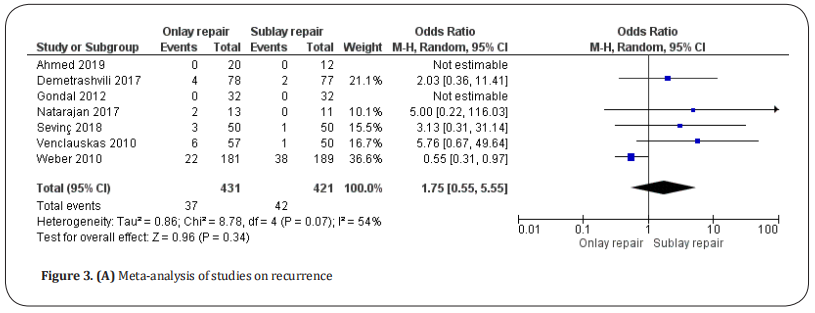
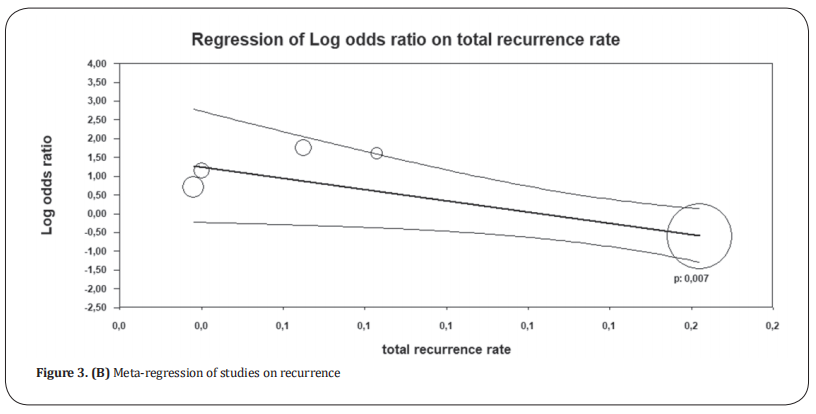
Recurrence. Recurrence was reported in seven studies [8,20–25]. After excluding patients lost of follow-up in these studies, we found a total of 852 patients (Figure 3.A). It was reported in 37 of 431 patients undergoing onlay repair and 42 of 421 patients undergoing sublay repair. There was no statistical difference between the two groups (OR: 1.75, 95% CI: 0.55–5.55, p = 0.34). There was a high level of heterogeneity between the studies (Tau2 = 0.86 and I2 = 54%). Random-effects meta-regression (Figure 3.B) favored sublay repair (p = 0.007).
Discuss
This is the first meta-analysis of RCTs comparing onlay
and sublay mesh repair of incisional hernias. Our results
show that sublay mesh repair yields better results than
onlay repair in terms of wound infection and seroma. We found no significant difference between the two
techniques in terms of hematoma. Regarding the recurrence rate, meta-regression favored sublay repair. We
conclude that sublay mesh repair should probably be the
first choice, and onlay mesh repair should be reserved
for more difficult cases, where sublay is not possible.
Mesh placement affects tissue incorporation, tissue
reaction, and tensile strength of the abdominal wall
[11,42–44]. In the case of incisional hernia, mesh bedding
dissection is challenging, especially in cases of previous
wound infection, hostile abdomen, multiple retromuscular repairs, and adhesions. A wide dissection with a
large mesh overlap is preferable in terms of tissue incorporation. However, this could be associated with an
increased risk of postoperative wound complications
and recurrence.
Wound complications present a problem following mesh
repair of incisional hernia and pose a higher risk of secondary recurrence [45]. Many studies have recommended sublay mesh repair for incisional hernias [44,46,47]. The
placement of the mesh on the posterior rectus fascia
benefits from a more vascularized area compared with
the onlay position [46]. Moreover, it is widely recognized
that dissection of subcutaneous suprafascial space for
onlay mesh placement promotes wound infection and
seroma [47].
Regarding wound infection, our results favor sublay
mesh repair. This does not seem to be directly related
to the mesh or to hernioplasty, but rather to poor skin
antisepsis [46,47]. Adequate sterilization of the skin before
the procedure is therefore essential. Some studies have
attributed the higher rate of mesh infections in patients
undergoing onlay repair to the more superficial position
of the mesh, which leaves it more exposed to bacterial colonization [29,48]. In contrast, in sublay mesh repair,
the placement of the mesh on the retrorectus prefascial
space offers the body’s immune system a better chance
of fighting infections [11,49]. Mesh infections occur in 5%
to 10% of mesh repairs [50,51]. Their management is complicated due to several factors, such as medical history,
causal germs, and type and location of the prosthesis in
the abdominal wall [52].
Seroma is related to a tight contact of any subcutaneous
foreign body (mesh). A meta-analysis of Timmermans et
al. [29] found no statistical difference between the onlay
and sublay techniques in terms of seroma frequency.
Other studies have reported a higher frequency associated with the onlay technique [53,54]. Our results also
show a higher seroma rate in onlay mesh repair. This
complication could be reduced by using low-thrombin
fibrin sealant, as well as by wearing an abdominal binder
postoperatively [55,56]. Overall, the postoperative complication rate (seroma, hematoma, and wound infection)
has been reported to be higher after onlay mesh repair
[49,57].
Regarding recurrence, many factors, such as wound complications, tensile strength of the abdominal wall, and
mesh shrinkage, can affect this outcome [43,45,58]. In sublay repair, the hernia sac is introduced to the abdominal
cavity. The wall defect is closed, and the mesh prevents
a new displacement. In onlay repair, the hernia defect
is not closed, and the mesh recovers the hernia. Nevertheless, it is only justified when the surgeon lacks of
skills or assistance from an experienced surgeon. Many
studies have reported contradictory results [23,24,29,53,59,60].
Some have reported a lower recurrence rate after the
sublay technique [53,61], whereas Wéber et al [54] found a
lower rate after the onlay method. Other studies have
reported similar rates associated with both procedures
[23,60]. However, other factors were not taken into consideration in the included studies, such as mesh overlap,
mesh fixation, and the surgeon’s experience are missed.
Moreover, this high degree of heterogeneity can be explained to some extent by the small number of patients
and the different follow-up periods included in these
studies. Surgical care of patients with recurrent hernias
may best be provided in referral centers with expertise
in the management of complex abdominal hernias [62].
All the studies included in this meta-analysis had comparable study populations and similar interventions. Our
main result concerning incisional hernia recurrence is
worthy of special attention. This outcome is characterized by a high level of heterogeneity. In the forest plot,
Wéber et al’s study [24], which included almost half of
all patients (370 of 852), was the only study to report a
lower recurrence rate after onlay mesh repair and was
thus a source of asymmetry and heterogeneity. Furthermore, the study was judged as of mediocre quality and
as potentially subject to location bias by Timmermans
et al [29]. This study did differ somewhat from the other
studies in that it only included larger hernias, which explains the heterogeneity. To compensate for heterogeneity, we used meta-regression, which is an extension
of subgroup analysis (Figure 3.B). When this study was
removed, the heterogeneity (I2) was reduced to 0%, and
the results became statistically significant in favor of
sublay repair. However, this uncertainty regarding the
recurrence rates makes it difficult to draw solid conclusions. Therefore, more multi-center RCTs with longer
follow-ups are recommended.
This meta-analysis has several limitations. We did
not assess hospital stay durations, postoperative pain
scores, chronic pain, long-term discomfort, and the time
of returning to everyday activities. These criteria were
not clearly defined in the included studies. Moreover,
the reference articles provided no data as to the types
of ventral incisional hernias and surgical wound characterizations, such as recurrent, infected, reoperated, and
previous mesh. The heterogeneity caused by Wéber et
al’s study [24] represents another limitation.
In summary, the available literature suggests that the
sublay technique for open ventral incisional hernia repair is superior to the onlay technique in terms of wound
complications and recurrence rate. Sublay mesh repair
should probably be the first choice for open incisional
hernia repair, and onlay repair should be reserved for
more difficult cases, where sublay is not possible.
Declaration
Conflicts of interest
Te authors declare that they have no conflict of interest.
References
1. Bosanquet, D. C., Ansell, J., Abdelrahman, T., Cornish, J.,
Harries, R., Stimpson, A., ... & Russell, D. (2015). Systematic
review and meta-regression of factors affecting midline
incisional hernia rates: analysis of 14 618 patients. PLoS
One, 10(9).
2. Paajanen, H., & Hermunen, H. (2004). Long-term pain and
recurrence after repair of ventral incisional hernias by
open mesh: clinical and MRI study. Langenbeck's archives
of surgery, 389(5), 366-370.
3. Sugerman, H. J., Kellum Jr, J. M., Reines, H. D., DeMaria,
E. J., Newsome, H. H., & Lowry, J. W. (1996). Greater
risk of incisional hernia with morbidly obese than
steroid-dependent patients and low recurrence with
prefascial polypropylene mesh. The American journal of
surgery, 171(1), 80-84.
4. Burger, J. W., Luijendijk, R. W., Hop, W. C., Halm, J. A.,
Verdaasdonk, E. G., & Jeekel, J. (2004). Long-term followup of a randomized controlled trial of suture versus mesh
repair of incisional hernia. Annals of surgery, 240(4), 578.
5. Kokotovic, D., Bisgaard, T., & Helgstrand, F. (2016). Longterm recurrence and complications associated with
elective incisional hernia repair. Jama, 316(15), 1575-
1582.
6. Den Hartog, D., Dur, A. H., Tuinebreijer, W. E., & Kreis,
R. W. (2008). Open surgical procedures for incisional
hernias. Cochrane Database of Systematic Reviews, (3),
CD006438.
7. Mathes, T., Walgenbach, M., & Siegel, R. (2016). Suture
versus mesh repair in primary and incisional ventral
hernias: a systematic review and meta-analysis. World
journal of surgery, 40(4), 826-835.
8. Natarajan, S., Meenaa, S., & Thimmaiah, K. A. (2017). A
randomised prospective study to evaluate preperitoneal
mesh repair versus onlay mesh repair and laparoscopic
IPOM in incisional hernia surgery. Indian Journal of
Surgery, 79(2), 96-100.
9. Korenkov, M., Sauerland, S., Arndt, M., Bograd, L.,
Neugebauer, E. A. M., & Troidl, H. (2002). Randomized
clinical trial of suture repair, polypropylene mesh or
autodermal hernioplasty for incisional hernia. British
Journal of Surgery, 89(1), 50-56.
10. Langer, C., Schaper, A., Liersch, T., Kulle, B., Flosman, M.,
Füzesi, L., & Becker, H. (2005). Prognosis factors in incisional
hernia surgery: 25 years of experience. Hernia, 9(1), 16-
21.
11. Dougaz, M.W., Chaouch, M.A., Cherni, S. et al. Preperitoneal
Versus Retromuscular Mesh Repair for Ventral Abdominal
Hernias: A Propensity Matched Analysis. Indian J Surg
(2020). https://doi.org/10.1007/s12262-020-02153-7
12. Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2010).
Preferred reporting items for systematic reviews and
meta-analyses: the PRISMA statement. Int J Surg, 8(5),
336-341.
13. Stoppa, R. E. (1989). The treatment of complicated groin
and incisional hernias. World journal of surgery, 13(5),
545-554.
14. Schumpelick, V., Klinge, U., Junge, K., & Stumpf, M.
(2004). Incisional abdominal hernia: the open mesh
repair. Langenbeck's archives of surgery, 389(1), 1-5.
15. Chevrel, J. P. (1979). Traitement des grandes éventrations
médianes par plastie en paletot et prothèse.
16. Begg, C., Cho, M., Eastwood, S., Horton, R., Moher, D.,
Olkin, I., ... & Stroup, D. F. (1996). Improving the quality of
reporting of randomized controlled trials: the CONSORT
statement. Jama, 276(8), 637-639.
17. Higgins, J. P., Thompson, S. G., Deeks, J. J., & Altman,
D. G. (2003). Measuring inconsistency in metaanalyses. Bmj, 327(7414), 557-560.
18. Higgins, J. P., & Green, S. (Eds.). (2011).Cochrane handbook
for systematic reviews of interventions (Vol. 4). John Wiley
& Sons.
19. Higgins, J. P., Green, S., & Collaboration, C. (2008). Cochrane
handbook for systematic reviews of interventions: Wiley
Online Library.
20. Gondal, S. H., & Anjum, I. H. (2012). Sutureless Sublay
verses Onlay Mesh Hernioplsty in Incisional Hernia Repair:
A comparative study at Teaching Hospital, Lahore. Pak J
Med Health Sci, 6(1), 238-41.
21. Demetrashvili, Z., Pipia, I., Loladze, D., Metreveli, T.,
Ekaladze, E., Kenchadze, G., & Khutsishvili, K. (2017).
Open retromuscular mesh repair versus onlay
technique of incisional hernia: A randomized controlled trial. International Journal of Surgery, 37, 65-70.
22. Sevinç, B., Okuş, A., Ay, S., Aksoy, N., & Karahan, Ö. (2018).
Randomized prospective comparison of long-term results
of onlay and sublay mesh repair techniques for incisional
hernia. Turkish journal of surgery, 34(1), 17.
23. Venclauskas, L., Maleckas, A., & Kiudelis, M. (2010). Oneyear follow-up after incisional hernia treatment: results of
a prospective randomized study. Hernia, 14(6), 575-582.
24. Wéber, G., Baracs, J., & Horváth, Ö. P. (2010). Kedvezőbb
műtéti eredmények „onlay” hálóval, mint „sublay”
helyzetben beültetettel. Magyar Sebészet, 63(5), 302-311.
25. Ahmed, M., & Mehboob, M. (2019). Comparisons of
Onlay versus Sublay Mesh Fixation Technique in Ventral
Abdominal Wall Incisional Hernia Repair. Journal of the
College of Physicians and Surgeons Pakistan, 29(9), 819-
822.
26. Leithy, M., Loulah, M., Greida, H. A., Baker, F. A., & Hayes, A.
M. (2014). Sublay hernioplasty versus onlay hernioplasty
in incisional hernia in diabetic patients. Menoufia Medical
Journal, 27(2), 353.
27. Cobb, W. S., Harris, J. B., Lokey, J. S., McGill, E. S., & Klove, K.
L. (2003). Incisional herniorrhaphy with intraperitoneal
composite mesh: a report of 95 cases. American
Surgeon, 69(9), 784-787.
28. Arer, I. M., Yabanoglu, H., Aytac, H. O., Ezer, A., & Caliskan, K.
(2017). Long-term results of retromuscular hernia repair:
a single center experience. The Pan African medical
journal, 27.
29. Timmermans, L., de Goede, B., van Dijk, S. M., Kleinrensink,
G. J., Jeekel, J., & Lange, J. F. (2014). Meta-analysis of sublay
versus onlay mesh repair in incisional hernia surgery. The
American Journal of Surgery, 207(6), 980-988.
30. Dhaigude, B. D., Sugunan, A., Pancbhai, S. V., Francis, M.,
Patel, K., & Metta, V. (2017). Comparative evaluation of
sublay versus onlay meshplasty in incisional and ventral
hernias. International Surgery Journal, 5(1), 187-192.
31. Ali, A. M., & Khalil, M. (2017). Ventral hernias meshplasty:
does mesh-implantation site affect the outcome?. The
Egyptian Journal of Surgery, 36(1), 69.
32. Dhanbhar R, Dash N. (2018). Comparative Study of Onlay
and Pre-Peritoneal Mesh Repair in the Management of
Ventral Hernias. Journal of Medical Science And clinical
Research, 06(03),391-395.
33. Afridi, S. P., Siddiqui, R. A., & Rajput, A. (2015).
Complications of Onlay and Sublay Mesh Plasty in Ventral
Abdominal Hernia Repair. Journal of Surgery Pakistan
(International), 20, 2.
34. Naz A, Abid K, Syed AA, Baig NN, Umer MF, Mehdi H.
Comparative evaluation of sublay versus onlay mesh
repair for ventral hernia. J Pak Med Assoc. 2018;68(5):4.
35. Shehryar, H. A., Shahka, M. A., & Javed, M. U. (2018).
Comparison of Sublay versus Onlay Mesh Technique of
Ventral Hernia Repair. PAKISTAN JOURNAL OF MEDICAL
& HEALTH SCIENCES, 12(1), 57-59.
36. SABER, Aly; EMAD, K. Bayumi. Onlay versus sublay mesh
repair for ventral hernia. J Surg, 2015, 4.1-1: 1-4.
37. Bessa, S. S., El-Gendi, A. M., Ghazal, A. H., & Al-Fayoumi,
T. A. (2015). Comparison between the short-term results
of onlay and sublay mesh placement in the management
of uncomplicated para-umbilical hernia: a prospective
randomized study. Hernia, 19(1), 141-146.
38. Abo-Ryia, M. H., El-Khadrawy, O. H., Moussa, G. I., &
Saleh, A. M. (2015). Prospective randomized evaluation
of open preperitoneal versus preaponeurotic primary
elective mesh repair for paraumbilical hernias. Surgery
today, 45(4), 429-433.
39. Ali, Q. (2013). Onlay versus sublay technique of repairing
ventral abdominal hernia. Journal of Rawalpindi Medical
College, 17(2), 192-194.
40. Choudhry, E. A., Sheth, J. Y., & Darshan, J. R. (2018). A
systemic analysis of patients undergoing open ventral
hernia repair (2011-2017). International Surgery
Journal, 5(7), 2567-2573.
41. Weber, G., & Horvath, O. P. (2002). Results of ventral hernia
repair: comparison of suture repair with mesh implantation
(onlay vs sublay) using open and laparoscopic approach-
-prospective, randomized, multicenter study. Magyar
sebeszet, 55(5), 285-289.
42. Johansson, M., Gunnarsson, U., & Strigård, K. (2011).
Different techniques for mesh application give the same
abdominal muscle strength. Hernia, 15(1), 65-68.
43. Binnebösel, M., Klink, C. D., Otto, J., Conze, J., Jansen,
P. L., Anurov, M., ... & Junge, K. (2010). Impact of mesh
positioning on foreign body reaction and collagenous
ingrowth in a rabbit model of open incisional hernia
repair. Hernia, 14(1), 71-77.
44. Nacef, K., Chaouch, M. A., Chaouch, A., Khalifa, M. B.,
Ghannouchi, M., & Boudokhane, M. (2018). Trocar site
post incisional hernia: about 19 cases. The Pan African
medical journal, 29.
45. Basoglu, M., Yildirgan, M. I., Yilmaz, I., Balik, A., Celebi, F.,
Atamanalp, S. S., ... & Oren, D. (2004). Late complications of
incisional hernias following prosthetic mesh repair. Acta
Chirurgica Belgica, 104(4), 425-448.
46. Cobb, W. S., Warren, J. A., Ewing, J. A., Burnikel, A., Merchant,
M., & Carbonell, A. M. (2015). Open retromuscular mesh
repair of complex incisional hernia: predictors of wound
events and recurrence. Journal of the American College of
Surgeons, 220(4), 606-613.
47. White, T. J., Santos, M. C., & Thompson, J. S. (1998).
Factors affecting wound complications in repair of ventral
hernias. The American Surgeon, 64(3), 276.
48. Deerenberg, E. B., Timmermans, L., Hogerzeil, D. P.,
Slieker, J. C., Eilers, P. H. C., Jeekel, J., & Lange, J. F. (2015).
A systematic review of the surgical treatment of large
incisional hernia. Hernia, 19(1), 89-101.
49. Köckerling, F. (2018). Onlay Technique in Incisional Hernia
Repair—A Systematic Review. Frontiers in surgery, 5, 71.
50. Carlson, M. A., Frantzides, C. T., Shostrom, V. K., & Laguna,
L. E. (2008). Minimally invasive ventral herniorrhaphy:
an analysis of 6,266 published cases. Hernia, 12(1), 9-22.
51. Sanchez, V. M., Abi-Haidar, Y. E., & Itani, K. M. (2011).
Mesh infection in ventral incisional hernia repair:
incidence, contributing factors, and treatment. Surgical
infections, 12(3), 205-210.
52. Stremitzer, S., Bachleitner-Hofmann, T., Gradl, B.,
Gruenbeck, M., Bachleitner-Hofmann, B., Mittlboeck, M.,
& Bergmann, M. (2010). Mesh graft infection following
abdominal hernia repair: risk factor evaluation and
strategies of mesh graft preservation. A retrospective
analysis of 476 operations.World journal of surgery,34(7),
1702-1709.
53. Israelsson, L. A., Smedberg, S., Montgomery, A., Nordin, P.,
& Spangen, L. (2006). Incisional hernia repair in Sweden
2002. Hernia, 10(3), 258-261.
54. Weber, G., Baracs, J., & Horvath, O. P. (2010). " Onlay"
mesh provides significantly better results than" sublay"
reconstruction. Prospective randomized multicenter
study of abdominal wall reconstruction with sutures
only, or with surgical mesh--results of a five-years followup. Magyar sebeszet, 63(5), 302-311.
55. Rothman, J. P., Gunnarsson, U., & Bisgaard, T. (1966).
Abdominal binders may reduce pain and improve physical
function after major abdominal surgery–a systematic
review. database, 2013.
56. Köhler, G., Koch, O. O., Antoniou, S. A., Lechner, M., Mayer,
F., & Emmanuel, K. (2014). Prevention of subcutaneous
seroma formation in open ventral hernia repair using
a new low-thrombin fibrin sealant. World journal of
surgery, 38(11), 2797-2803.
57. Holihan, J. L., Nguyen, D. H., Nguyen, M. T., Mo, J., Kao, L.
S., & Liang, M. K. (2016). Mesh location in open ventral
hernia repair: a systematic review and network metaanalysis. World journal of surgery, 40(1), 89-99.
58. García-Ureña, M. Á., Ruiz, V. V., Godoy, A. D., Perea, J. M. B.,
Gómez, L. M. M., Hernández, F. J. C., & García, M. Á. V. (2007).
Differences in polypropylene shrinkage depending on
mesh position in an experimental study. The American
journal of surgery, 193(4), 538-542.
59. Gleysteen, J. J. (2009). Mesh-reinforced ventral hernia
repair: preference for 2 techniques. Archives of
Surgery, 144(8), 740-745.
60. de Vries Reilingh, T. S., van Geldere, D., Langenhorst, B. L.,
de Jong, D., van der Wilt, G. J., van Goor, H., & Bleichrodt,
R. P. (2004). Repair of large midline incisional hernias
with polypropylene mesh: comparison of three operative
techniques. Hernia, 8(1), 56-59.
61. Gleysteen, J. J. (2009). Mesh-reinforced ventral hernia
repair: preference for 2 techniques. Archives of
Surgery, 144(8), 740-745.
62. Novitsky, Y. W., Porter, J. R., Rucho, Z. C., Getz, S. B., Pratt, B. L.,
Kercher, K. W., & Heniford, B. T. (2006). Open preperitoneal
retrofascial mesh repair for multiply recurrent ventral
incisional hernias. Journal of the American College of
Surgeons, 203(3), 283-289.