Open Access | Research Article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Evaluation of Subclavian, Thoracic Aorta, and Innominate Artery Injuries in Blunt Trauma Mechanisms: A Systematic Review of Case Reports and Case Series
*Corresponding author: Segni Kejela
Mailing address: Department of surgery, Tikur Anbessa Specialized Hospital, Addis Ababa University, College of Health Sciences, Ethiopia.
Email: segnikejo@gmail.com
Received: 31 October 2019 Accepted: 05 December 2019
DOI: 10.31491/CSRC.2019.12.039
Abstract
Background: Blunt thoracic arterial injuries are among the rare causes for presentation at trauma centers. Most of the literature on these injuries is in the form of case reports and case series, with no significantly consolidated data available.
Methods: A systematic review of English language case reports and case series from 2000 to 2019 was carried out using the PubMed and Google Scholar search engines.
Results: The mean patient ages were 35.9, 36.4, and 44.3 years for thoracic aorta, innominate, and subclavian artery injuries, respectively. Of the innominate artery injury patients, 89.7% were male. Motor vehicle-related injuries contributed to 50.9% of thoracic aortic injuries. A blood pressure/pulse deficit was recorded in 34.8% and 20.7% of patients with subclavian and innominate artery injuries, respectively, and chest pain and hemodynamic instability were found in 23.5% and 20.5% of aortic injury patients, respectively. Clavicular fracture was the most common associated finding in subclavian artery injury patients at 42%. Computed tomography was performed in 21.7%, 47.1%, and 27.6% of patients with subclavian artery, thoracic aorta, and innominate artery injuries, respectively. An endovascular intervention was performed in 44.1% of patients with subclavian artery injuries.
Conclusion: Injury to the subclavian artery is relatively common among the older population. Blood pressure or pulse discrepancies could point to either subclavian or innominate artery injury. An endovascular intervention can be considered in all patients but must be individualized based on patient and facility factors.
Keywords
Aortic rupture; clavicular fracture; traumatic pseudoaneurysm; endovascular repair; cerebrovascular accident
Introduction
Trauma is the most common cause of mortality in
children and adults under 44 years of age [1]. Blunt
trauma is the leading mechanism affecting patients in
most civilian trauma centers [2, 3]. Furthermore, motor
vehicle accidents are the principal cause of blunt trauma, accounting for 1.3 million deaths, 20s–50 million
non-fatal injuries, and 29% of all trauma cases annually [4, 5]. The overall incidence of vascular trauma is
5%, with a larger fraction contributed by penetrating
trauma mechanisms [6, 7]. In fact, trauma centers report
that only 5% of vascular trauma cases are caused by blunt mechanisms [8]. However, this may be an underestimation because many blunt trauma patients with
major vascular injuries do not survive long enough to
reach a healthcare facility. The findings of postmortem
examinations of prehospital trauma deaths support
this notion, placing blunt major vascular trauma as the
second most common cause of death, after head injury
[9, 10].
The paucity of blunt vascular injuries in trauma centers
is reflected in the literature; most of the relevant publications are case reports and case series [11].
This review is intended to integrate the experiences of
centers around the world through the analysis of case
reports and case series concerning this issue and hopefully fill the knowledge gaps surrounding the epidemiological changes, investigative modality advancements,
and management innovations for blunt vascular trauma.
Methods
Data source and search strategy
PubMed and Google Scholar were utilized to search for publications between January 2000 and September 2019 posing no language restrictions to the authors. The following key statements were utilized to initiate the search process: “case report/case series, subclavian artery injury,” “case report/case series, thoracic aorta injury,” and “case report/case series, innominate artery injury.”
Inclusion criteria
All case reports and case series on subclavian, thoracic aorta, and innominate artery injuries arising from blunt mechanisms with no missing publication segments and published in English were included. Only publications from January 2000 to September 2019 were included.
Exclusion criteria
The exclusion criteria were as follows: any blunt vascular injuries not involving the subclavian artery, thoracic
aorta, or innominate artery.
All reports of vascular injury with a penetrating mechanism of trauma were excluded.
Publications that are primarily produced in a language
other than English were excluded.
Data extraction and handling
From each patient report, the following information was retrieved: year of reported case, age at presentation, sex, mechanism of injury, general complaint/clinical presentations, associated injuries, specific vertebral injury, intracranial injury, associated vascular injuries (in addition to the injured vessels under study), chest wall injuries, pulmonary injuries, facial injuries, limb injuries, abdominal injuries, specific type of vascular injury for the main thoracic arterial injuries under question, diagnostic modality utilized, treatment provided, type of open surgical treatment provided, and outcome with specific complications pertaining to the vascular injury and mortality. No effort was made to communicate with authors concerning missing data from the publications.
Data synthesis and analysis
The generated data was entered into SPSS version 23
in the categories mentioned above, and the accuracy of
the data was evaluated and ascertained.
After the data entry and cleanup were complete, the
data analysis was conducted using the same software:
SPSS version 23.
Results
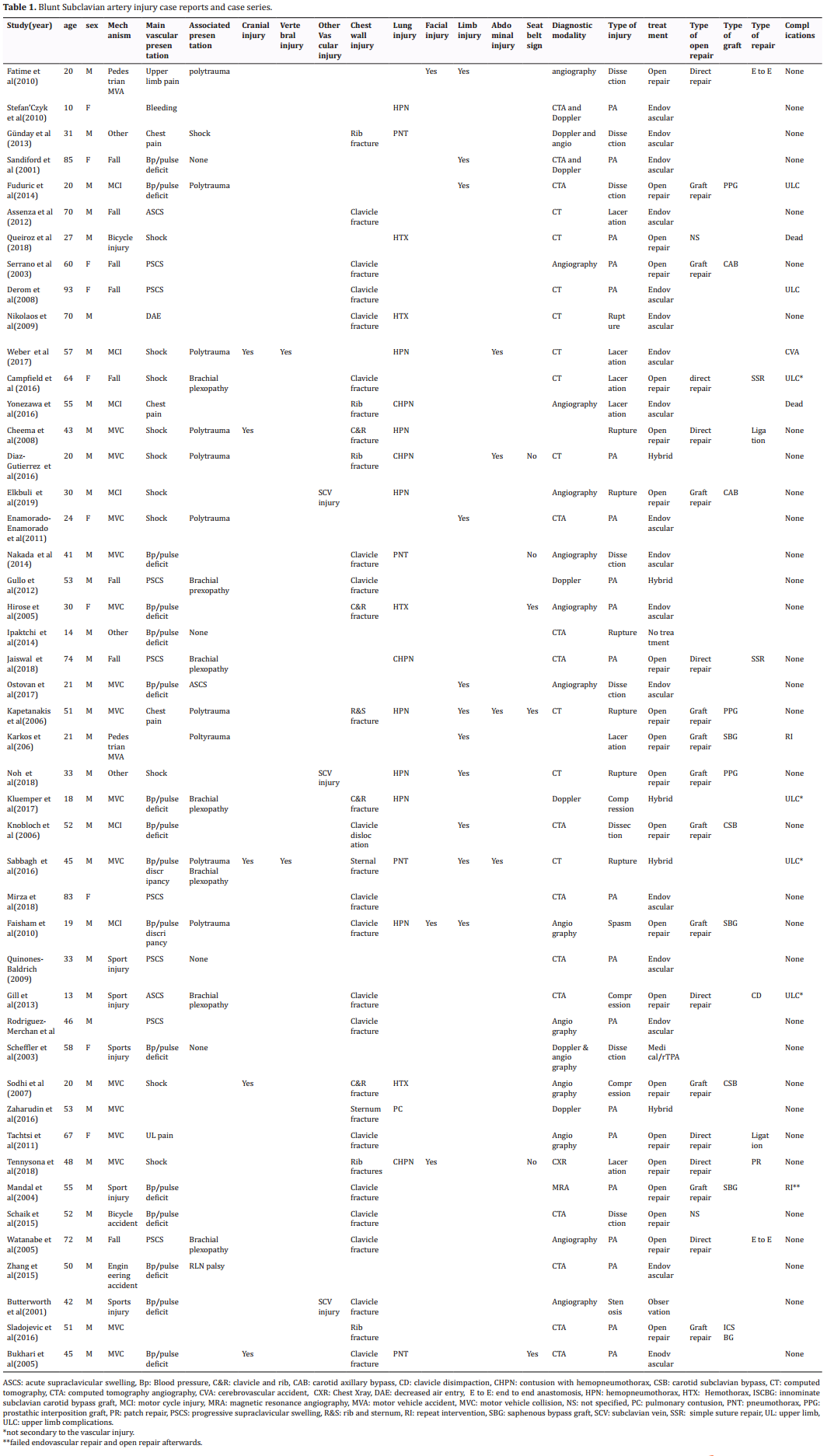
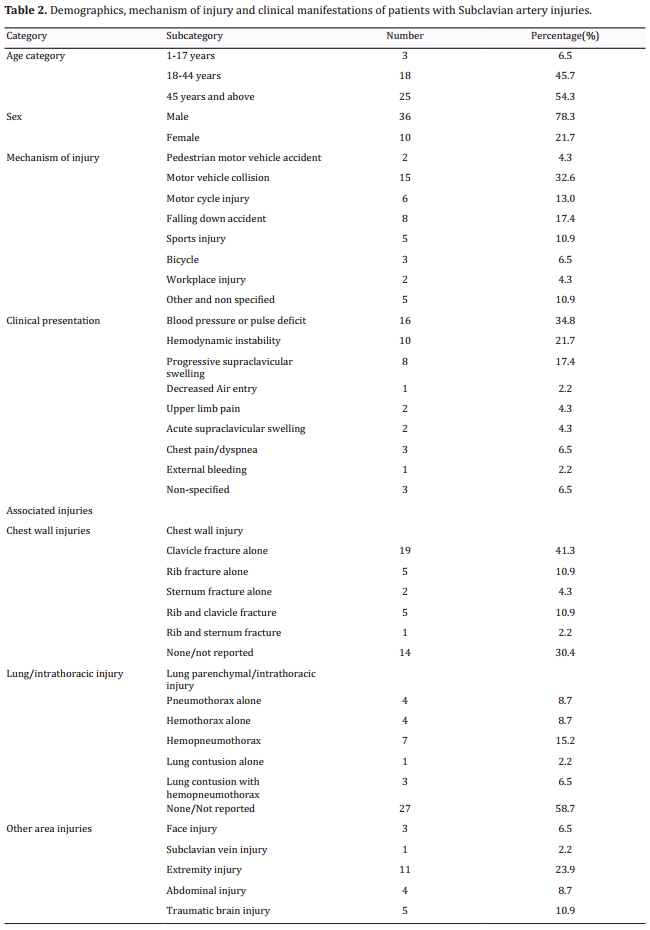
Subclavian artery injury
The cases of a total of 46 patients with subclavian artery injuries were reviewed (Table 1). The mean age of
the patients was 44.33±21.11 years, and 73.8% were
male. Motor vehicle collisions were involved in 32.6%
of the cases. Motor vehicle-related injuries were reported in 13 (65%) patients younger than 45 years of
age. Patients older than 45 years of age presented due
to a falling accident in 36.4% of the reported cases. Of
the female patients with subclavian artery injuries, half
presented due to a falling accident.
Hemodynamic instability was recorded in 21.7% of the
patients as a main clinical presenting sign/symptom,
and polytrauma was reported in 10 (21.7%) of the
patients. The most common clinical manifestations of
motor vehicle-related subclavian artery injuries were
blood pressure/pulse deficit (9 patients, 45%) and hemodynamic instability (7 patients, 35%). Patients presenting with subclavian artery injury after falling accidents reported progressive supraclavicular swelling in
5 (63.5%) cases. Three out of the 5 patients presenting
with sports-related injuries presented with a blood
pressure/pulse deficit.
Concerning associated injuries, clavicular fracture was
reported in 24 (52.2%) cases. Of the patients with subclavian artery injuries and clavicular fractures, 62.5%
were 45 years of age or older. Four (8.7%) of the patients had reported traumatic brachial plexopathy, and
10 (21.7%) of the patients presented with polytrauma.
Of the reviewed patients, 15 (32.6%) had a pneumothorax, hemothorax, or both at presentation (Table 2).
Regarding the diagnostic modalities utilized, 44 cases reported the use of 1 or more imaging techniques.
Conventional/digital subtracted angiography was
utilized in 13 (28.3%) of the reported cases, and doppler ultrasonography, contrast CT, and CT angiography
were used in 3 (6.5%), 10 (21.7%), and 12 (26.1%)
cases, respectively. One patient had a chest x-ray as the
sole imaging modality for diagnosis. A combination of
CT angiography and conventional angiography with
Doppler ultrasonography was conducted in 2 (4.3%)
patients.
The types of vascular injuries diagnosed using imaging modalities or with intra-operative findings were
reported in all 46 patients in this review. Pseudoaneurysm and dissection were reported in 20 (43.5%) and
8 (17.4%) of the cases, respectively. Rupture, laceration, and compression occurred in 4 (15.2%), 6 (13%),
and 3 (6.5%) of the cases, respectively. One patient
presented with a spasm of the subclavian artery.
The treatment modalities were specified in all 46 of the
reviewed cases, with open surgical repair performed
in 21 (45.7%) cases and endovascular and hybrid procedures performed in 17 (37%) and 5 (10.9%) cases,
respectively. Three patients underwent conservative/
medical therapy. Within the open surgical repair group,
11 (57%) underwent graft repair. Of the graft repair
patients, 3 (27.3%), 2 (18.1%), and 2 (18.1%) underwent a prosthetic interposition graft, a prosthetic
carotid-subclavian bypass, and a prosthetic carotid-axillary bypass graft, respectively. In addition, 3 (27.3%) patients underwent a saphenous bypass graft, 8 (42.1%
of the open repair cases) patients had direct repairs
with end-to-end anastomosis, a simple suture and ligation were performed in 2 (25%) patients, and 1 patient
underwent a patch repair.
The outcomes and complications were reported in 45
of the 46 cases, with 73.9% of patients experiencing
total resolution and 6 (13%) experiencing upper limb
complications, of which 4 were confirmed brachial
plexopathy at presentation rather than vascular injury-related complications. Repeat intervention was
needed in 2 (4.3%) patients, and 2 (4.3%) patients
died. Furthermore, 1 patient was diagnosed with a
cerebrovascular accident related to the subclavian artery injury.
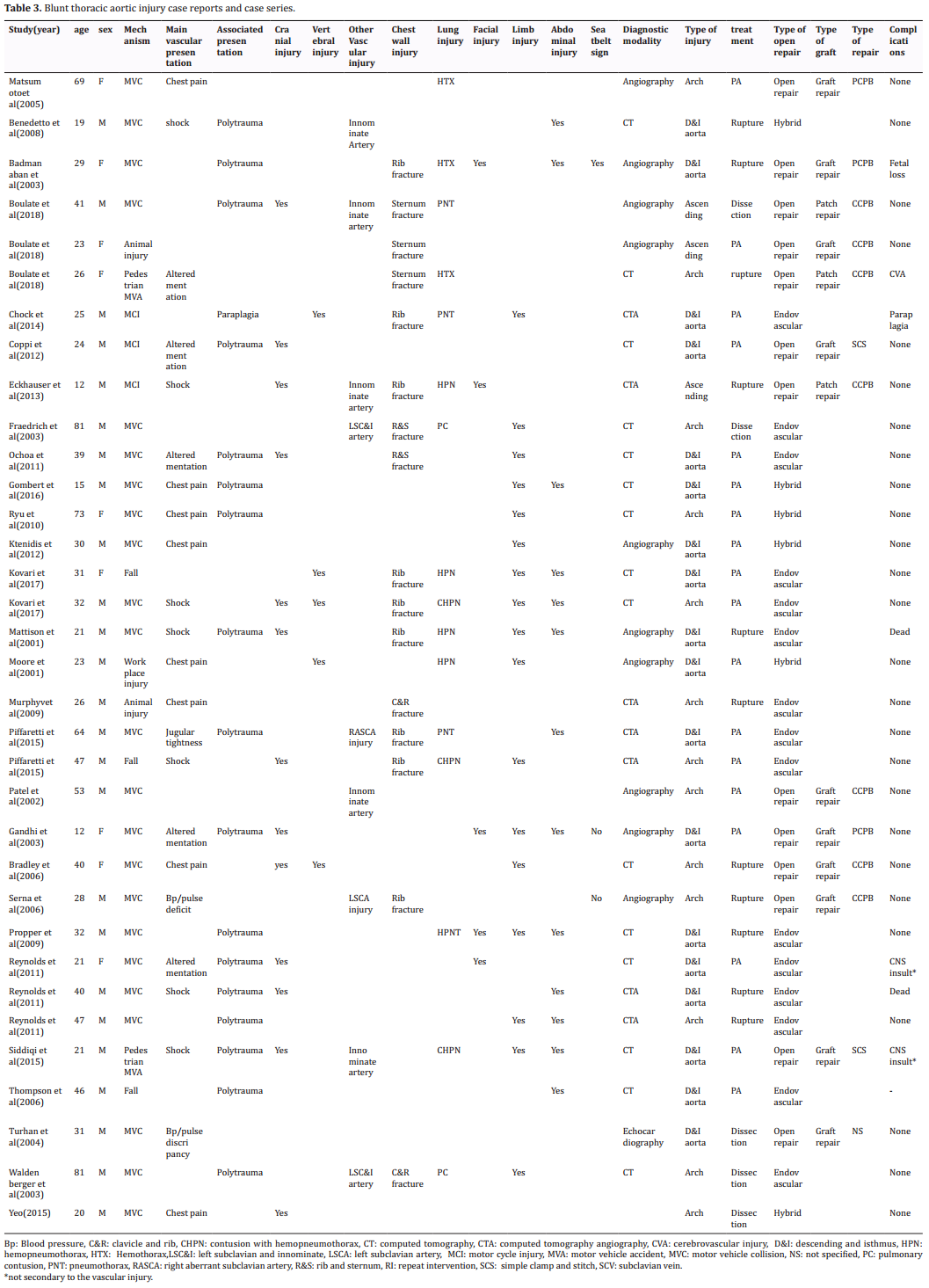
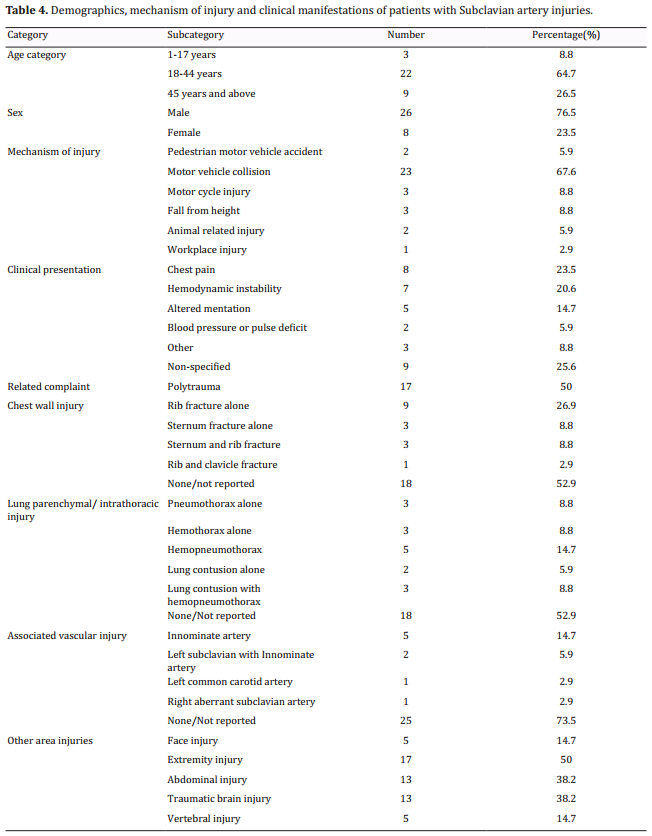
Thoracic Aorta injury
The data for a total of 34 aortic injury patients was
retrieved from the literature between 2000 and 2019
(Table 3). The mean age of the patients with aortic injuries was 35.9±18.9 years, and 26 (76.5%) of the patients were male. Of the patients examined, 23 (67.6%)
presented after a motor vehicle collision, and 28
(82.4%) had injuries related to motor vehicles (including pedestrian motor vehicle accidents and motorcycle
injuries). Hemodynamic instability (hypotension) and
chest pain were the chief clinical features in 7 (20.6%)
and 8 (23.5%) of the cases, respectively. Polytrauma
was reported in 17 (50%) of the patients. Twenty-one
(84%) of the patients aged under 45 years had motor
vehicle-related injuries, compared to 7 (77.7%) of the
patients aged 45 years or older. Female patients presented after motor vehicle accidents in 87.5% of the
cases, compared to 80.7% in male patients.
Rib fracture was the most common associated chest
wall injury, presenting in 9 (26.9%) of the cases overall
and in 3 (8.8%) and 1 (2.9%) cases with sternum and
clavicle fractures, respectively. Hemopneumothorax
alone was reported in 5 (14.7%) patients, and with
lung contusion in 3 (8.8%) patients. Five (14.7%) patients had an abdominal-associated innominate artery
injury, and 13 (38.2%) patients had an associated traumatic brain injury (Table 4).
The most common imaging modalities utilized were
contrast CT scanning and CT angiography, which were
used in 16 (47.1%) and 7 (20.6%) cases, respectively,
and conventional/digital subtracted angiography was
used in 10 (29.4%) cases. The most common sites of
injury were the isthmus and the descending aorta,
accounting for 18 (52.9%) of the examined cases. The
aortic arch and the ascending aorta were injured in 13
(38.2%) and 3 (8.8%) cases, respectively. A pseudoaneurysm was discovered in 18 (52.9%) of the patients
using an imaging modality or intraoperative findings.
Rupture was diagnosed in 11 (32.4%) cases and dissection with or without thrombosis in 5 (14.7%) cases.
Regarding treatment, 13 (38.2%) patients underwent open surgical repair, with endovascular repair
performed in 15 (44.1%) and a hybrid method in 6
(17.6%) cases. In the open repair group 10 out of 13
(76.9%) of the patients underwent a repair using a
prosthetic graft, and 3 (23.1%) underwent a patch
repair. The majority of the open procedures—7 cases
(53.8%)—were performed under a complete cardiopulmonary bypass with deep hypothermic arrest and
a centrifugal pump (3 cases, 23.1%). Two patients underwent a simple clamp and stitch procedure with no
bypass.
In terms of the outcomes and complications in the
aortic injury patients, 76.5% experienced complete
resolution, with 2 deaths out of the 34 patients reported. Three (9%) patients had chronic cerebral sequele,
with 2 of the 3 cases caused by traumatic brain injury.
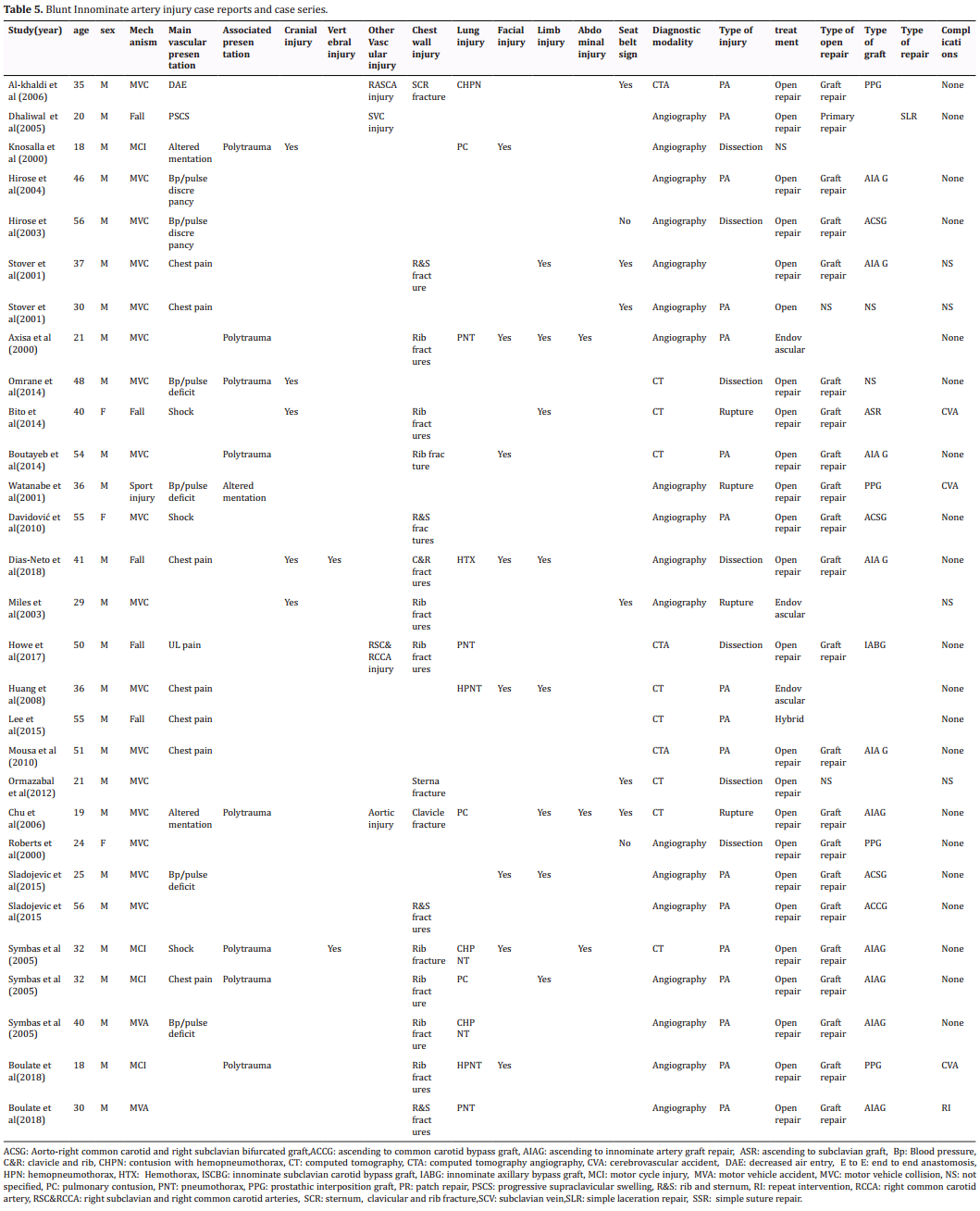
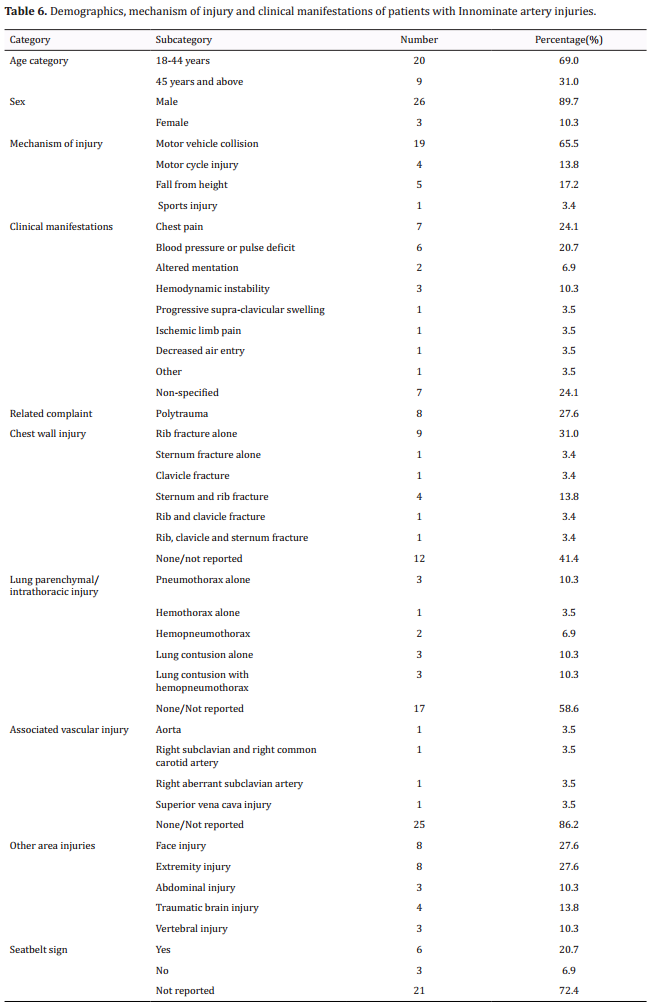
Innominate artery injury
The data of a total of 29 patients was retrieved from
reports from 2000 to 2019 (Table 5). The mean age
of the patients with innominate artery injuries was
36.4±12.8 years, and 26 (89.7%) of the patients
were male. Motor vehicle collisions contributed to 19
(65.5%) of the innominate artery injury cases, with
motor vehicle associated-injuries accounting for 79.3%
of the cases. Regarding the clinical presentations of the
innominate artery injury patients, chest pain and blood
pressure/pulse deficit were reported in 7 (24.1%) and
6 (20.7%) cases, respectively. Polytrauma was reported in 8 (27.6%) cases.
Rib fracture alone was reported in 9 (31%) patients
and with sternum fracture in 4 (13.8%) patients. Lung
contusion alone was reported in 3 (10.3%) patients
and with hemopneumothorax in another 3 (10.3%).
Eight (27.6%) of the cases included facial injuries. Extremity injuries were reported in 8 of the 29 patients
(27.6%), and 6 (20.7%) had a seatbelt sign (Table 6).
Regarding diagnostic imaging and treatment modalities, angiography (conventional/digital subtracted)
was utilized in 18 (62.1%) cases. A contrast CT scan
and CT angiography were performed in 8 (27.6%)
and 3 (10.3%) cases, respectively. A pseudoaneurysm
was identified using imaging modalities or intraoperative findings in 58.6% of the reported cases, whereas
24.1% of the cases had dissection with or without
intravascular thrombosis, and rupture was present in
13.8% of the cases.In 1 case, the type of innominate
injury was not further specified. Twenty-four (82.8%)
patients underwent open surgical repair: 3 patients
were treated with an endovascular technique, and 1
patient was treated with a hybrid method. Twenty-one
of the 24 (87.5%) patients treated with open repair underwent a graft repair, and 1 patient was treated with
a direct suture repair. Two cases did not specify the
method of open repair used. Among the patients in the
graft repair group, 10 (47.6%) had an ascending aorta
to innominate artery bypass graft, whereas 3 (14.3%)
had an aorto-right common carotid and right subclavian bifurcated bypass graft. An interposition graft was performed in 4 (19%) patients, and ascending aorta to
common carotid artery bypass, innominate to axillary
artery bypass graft, and ascending aorta to subclavian
artery bypass procedures were performed in 1 patient
each.
Among the patients with innominate artery injuries,
69% experienced complete resolution and were
symptom free at follow-up, 10.3% of the patients had
a cerebrovascular accident pertaining to the arterial
injuries, and 1 patient required a repeat intervention.
Discussion
Subclavian artery injury
Subclavian artery injuries were more common in
males, corresponding with the results of a report by
Sturm et al. in 1984, which included 80% (12 out of
15 patients) male patients [108]. The mean age of the
patients examined in this review was relatively older
than that of the report of 26.2 years by Sturmet al.but
relatively younger than a case series published in 2001
from cases treated before 1998, which reported a
mean age of 57 years [107, 108].
Motor vehicle-related injuries were reported in almost
half of the reviewed cases as a mechanism of trauma,
which is low compared to other studies [107–109]. Motor
vehicle-related injuries were found to be more common among males than females in this review, corresponding to a significantly higher rate of motor vehicle-related fatalities among males than among females
[110]. A point worth mentioning is the high proportion of
fall-related subclavian artery injuries in older patients,
which has never been previously reported in systematic reviews.
The most common clinical presenting signs and symptoms in the reviewed cases were blood pressure/pulse
deficit and hemodynamic instability. This is certainly
not an outlier in the context of blunt subclavian artery
injuries. Katras et al.reported that 7 out of the 15 patient cases they reviewed included hypotension (unstable hemodynamic status), and 7 out of 15 included
diminished or absent pulse [107]. Patients with subclavian artery injuries after a fall had a less dramatic, but
more progressive presentation of progressive supraclavicular swelling, pointing toward the necessity for a
more vigilant follow-up in these cases.
Clavicular fracture was the most common associated
fracture in patients with subclavian artery injuries,
with more than half of patients presenting with this
fracture. This finding has been replicated by multiple
reviews articles published by other authors [107–109].
Concerning imaging modalities, conventional/digital
subtracted angiography was the most commonly utilized technique, followed by CT angiography and standard contrast CT scanning. In the present review, conventional angiography was used less frequently than
in previous reviews.This is consistent with a review by
Sturm et al., in which 14 of the 15 patients underwent
conventional diagnostic angiography before operative
management was performed. In addition, Costa and
Robbs reported that conventional angiography was
performed in all 11 patients for whom operative management was provided [108, 109]. Investigative modalities
have found that most vascular lesions are pseudoaneurysms. However, this was not exhibited in a review by
Katras et al.,in which only 2 of the 7 patients had pseudoaneurysm of the subclavian artery [108].
Endovascular and hybrid methods of treatment together have contributed to managing 48% of subclavian
artery injuries, which certainly demonstrates a significant shift from the previous reports from the end of
the past century. In all 3 of the reports examined from
this period—those of Strum et al., Katras et al.,and Costa and Robbs—only open repair was reported in all of
the patients [107–109]. In the present review, the open repair group underwent more graft repairs than primary/direct sutures, which is similar to Costa and Robbs’
report [109].
Regarding patient outcomes, 6 out of the 46 patients
in this review experienced upper limb complications
due to either vascular or non-vascular causes. This
outcome was significantly rarer than in the 7 out of
15 patient cases with limb complications in Costa and
Robbs’ report [109]. This may be due to recent improvements in operative techniques and the advent of endovascular and hybrid techniques.
Subclavian artery injury
More than 3/4ths of the patients with blunt thoracic
aortic injury in this review were male, with motor
vehicle-related injuries being the most common mechanism. This corresponds to a larger study from Germany, in which 77.5% of the patients with blunt thoracic
aorta injuries were male, and high-speed motor vehicle
accidents caused 78% of the blunt thoracic aortic injuries [111].
The most common clinical manifestations in this review were chest pain and hemodynamic instability
(hypotension). Hemodynamic instability was more
common in a German study, appearing in 35.6% to
70.1% of cases depending on the vascular lesions in
question [111]. Polytrauma was reported in the present
review in half of patients, and cervical and thoracic
vertebral injuries were reported in significant number
of patients at, 14.7%, although no prior data is available for comparison.
Rib fracture is the most common chest wall trauma associated with blunt thoracic aorta injury. There is also
a high rate of associated traumatic brain injury among
blunt thoracic aorta injuries. An autopsy report by Burkhart et al.showed higher rates of rib fracture and traumatic brain injury (69% and 68%, respectively) than
this review (26.9% and 38.2%, respectively) [112]. This
may be because autopsy cases have an expected higher
severity of injury than the patient cases examined in
the present review. In addition, in the present review, nearly half of the patients had 1 or more pulmonary
injuries. This high occurrence is still lower than that
of the autopsy reports of patients with thoracic aorta
injuries [112].
Innominate artery injuries were most commonly associated with aortic injuries, and although prior studies
linking aortic and innominate artery injury are not
available, this association is logical. Similar trauma
mechanisms and anatomic proximity make both vessels vulnerable simultaneously.
CT scanning was the diagnostic modality of choice in
nearly half of the patient cases in the present review
[113]. This is consistent with the recommendation from
Mirvis et al., who argue that, given its sensitivity and
specificity of greater than 90%, the CT scan is a good
option for traumatic aortic injury diagnosis. In fact, an
additional 1/5th of patientsin the present review underwent CT angiography, further decreasing the need
for conventional/digital subtracted angiography.
In the present review, most patients (52.9%) had injuries either at the isthmus or the descending aorta.This
is slightly lower than in other studies. For instance,
Williams et al. reported that 65% of the reviewed injuries occurred at the isthmus or the descending aorta
[114]. Pseudoaneurysm was the most common vascular
lesion in this review. This is similar to other findings
in the literature, including those of Starnes et al., in
which pseudoaneurysm was reported among 71% of
the blunt aortic injury patients [115].
Endovascular repair was the most common modality
of thoracic aorta repair in the present review. In fact,
with the introduction of the hybrid method, close to
2/3rds of patients underwent a minimally invasive
corrective procedure with either total endovascular or
hybrid techniques. This data is similar to the findings
of Gombert et al.,in which 62.8% of patients underwent an endovascular procedure. However, contrary to
what Gombert et al. reported, this review did not find
patients who underwent conservative management
with no surgical intervention [111]. Graft repair was the
most common method of open repair in the present
review.
The present review revealed a 6% mortality rate,
which is significantly lower than the rates reported by
large reviews, such as that by Gombert et al.,in which
a 40.8% rate of total mortality was reported [111]. This
level of staggering difference may be attributed to the
fact that the case reports and case series in the present
review are those of living patients rather than fatalities.
Innominate artery injury
The mean ages of the thoracic aorta and innominate
artery injury patients are quite similar. The high male
predominance (89.7%) identified in this review is consistent with the results of an older review by Hirose
and Gill, which showed a male predominance of 86.3%.
Motor vehicle related-accidents were the mechanism
of injury in more than 80% of the patients in this review, which is similar to the 88.9% reported by Hirose
and Gill. Chest pain and blood pressure/pulse discrepancies were the 2 dominant manifestations, occurring
in almost half of the patients in the present review.
Hirose and Gill reported that 20 out of 132 patients
(15.15%) experienced blood pressure/pulse deficits
even though thy didn’t report on Chest pain [90].
On the subject of associated injuries, this review found
rib fractures in almost half of the reported cases, polytrauma in 1/4th of the reports, and a significant number (41.4%) of instances of at least 1 pulmonary injury.
Hirose and Gill reported a significantly lower rate of rib
fractures (16 out of 132 cases, 12.1%). Similarly, Hirose
and Gill reported only 28 out of 132 patients experiencing pulmonary complications, which is also significantly lower than the rate obtained in this review. The
reason for these discrepancies is unknown. The rate of
head injury, at 13.8% in this review, is comparable to
that in the report from Hirose and Gill, in which 15 out
of 132 patients (11.4%) experienced a traumatic brain
injury [90]. The seatbelt sign status was reported in 8 patients in the present review, of which 6 had a seatbelt
sign, which can indicate a sudden deceleration injury
that may have caused the innominate artery injuries.
Although 62% of patients in this review underwent a
diagnostic angiography, this invasive modality seems
to be decreasing in popularity. Hirose and Gill reported
that in all of their reviewed cases with a reported imaging modality, diagnostic conventional angiography
was used, which caused the authors to conclude that
angiography is the gold standard modality. This shows
a slow yet steady increase in the utilization of noninvasive diagnostic modalities such as CT with contrast and
CT angiography.
The present review found pseudoaneurysm in more
than half of the cases. This correlates well with similar
review findings on thoracic aorta and subclavian artery
injuries [90].
In the innominate artery injury cases examined in the
present review, open repair was the most common
management modality (in contrast with the for aortic
and subclavian artery repair, for which endovascular
intervention was preferred more often). Hirose and Gill
did not report any endovascular procedures in the case
reports reviewed prior to 2003. Although the progress
towards endovascular and hybrid techniques may be
slower compared to aortic and subclavian artery injury
repairs, more and more surgeons have been utilizing
endovascular interventions in recent years [90].
In the present review, complications with cerebrovascular accidents occurred in 10% of the patient cases,
and all of these complications occurred in the open
surgical repair group and none in innominate artery injury patients treated with endovascular interventions.
This could be due to selection bias because more stable
patients may have been more likely to be managed
with endovascular techniques than those undergoing open repairs.
Conclusion
In subclavian artery injuries, clavicular fracture can
point to arterial injuries, especially in older patients.
Blood pressure/pulse deficits were the most common
clinical indicators of these injuries.Investigations using
CT with contrast, CT angiography, or conventional angiography are typically performed in these cases, with
no clear preference of any one over the others. Open
repair is still the most common treatment modality,
with an increasing use of endovascular techniques.
Blunt thoracic aortic injuries are common among highspeed deceleration injuries. Chest pain in a patient
with a significant trauma mechanism is a good indicator that further investigation is needed, especially
when associated with head trauma or polytrauma. A
CT scan can be the first and even the modality of choice
for this investigation. Endovascular procedures can be
considered regardless of the type of vascular lesion.
Innominate artery injury is a predominantly motor
vehicle-related injury. Chest pain and blood pressure/
pulse deficits are the most common clinical features of
this injury. Suspected innominate artery injuries may
need conventional/digital subtracted angiography,
and the threshold for performing these tests should be
lower. Open surgical management is still the procedure
of choice, and until further knowledge is gained, there
can be no recommendation to replace this time-tested
technique.
Declaration
Conflicts of interest
All authors declare that there are no conflicts of interest.
References
1. Heron, M. P. (2019). National Vital Statistics report:
Deaths: leading causes for 2017 June 24 2019, 68(6) 1-77.
2. Moodley, N. B., Aldous, C., & Clarke, D. L. (2014). An audit
of trauma-related mortality in a provincial capital in South
Africa. South African Journal of Surgery, 52(4), 101-104.
3. Byun, C. S., Park, I. H., Oh, J. H., Bae, K. S., Lee, K. H., & Lee,
E. (2015). Epidemiology of trauma patients and analysis
of 268 mortality cases: trends of a single center in Korea. Yonsei medical journal, 56(1), 220-226.
4. World Health Organization. (2015). Global status report
on road safety 2015. World Health Organization.
5. World Health Organization. Violence, Injury Prevention, &
World Health Organization. (2013). Global status report
on road safety 2013: supporting a decade of action. World
Health Organization.
6. Baghi, I., Herfatkar, M. R., Shokrgozar, L., Poor-Rasuli, Z., &
Aghajani, F. (2015). Assessment of vascular injuries and
reconstruction. Trauma monthly, 20(4).
7. Perkins, Z. B., De'Ath, H. D., Aylwin, C., Brohi, K., Walsh, M., &
Tai, N. R. M. (2012). Epidemiology and outcome of vascular
trauma at a British Major Trauma Centre. European journal of vascular and endovascular surgery, 44(2), 203-209.
8. Mattox, K. L., Feliciano, D. V., Burch, J., Beall Jr, A. C., Jordan
Jr, G. L., & De Bakey, M. E. (1989). Five thousand seven
hundred sixty cardiovascular injuries in 4459 patients.
Epidemiologic evolution 1958 to 1987. Annals of surgery,
209(6), 698.
9. Baker, C. C., Oppenheimer, L., Stephens, B., Lewis, F. R., &
Trunkey, D. D. (1980). Epidemiology of trauma deaths. The
American Journal of Surgery, 140(1), 144-150.
10. Sobrino, J., & Shafi, S. (2013, April). Timing and causes of
death after injuries. In Baylor University Medical Center
Proceedings (Vol. 26, No. 2, pp. 120-123). Taylor & Francis.
11. O’Connor JV, Byrne C, Scalea TM, Griffith BP, Neschis DG.
(2019). Vascular injuries after blunt chest trauma: diagnosis and management. Scand J Trauma Resusc Emerg
Med, 17, 1-10.
12. Fatimi, S. H., Anees, A., Muzaffar, M., & Hanif, H. M. (2010).
Acute traumatic subclavian artery thrombosis and its successful repair via resection and end-to-end anastomosis.
Chinese Journal of Traumatology (English Edition), 13(4),
255-256.
13. Stefańczyk, L., Czeczotka, J., Elgalal, M., Sapieha, M., &
Rowiński, O. (2011). A large posttraumatic subclavian
artery aneurysm complicated by artery occlusion and arteriobronchial fistula successfully treated using a covered
stent. Cardiovascular and interventional radiology, 34(2),
146-149.
14. Günday, M., Özülkü, M., Yıldırım, E., Güven, A., & Çiftçi, Ö.
(2013). Successful endovascular treatment of subclavian
artery dissection after compression trauma. The American journal of emergency medicine, 31(2), 457-e1.
15. Sandiford, N., Tsitskaris, K., & Erritty, M. (2010). Delayed
presentation of a pseudoaneurysm of the subclavian and
axillary artery–the importance of vigilance. Journal of the
Royal Society of Medicine, 103(2), 67-69.
16. Fudurić, J., Erdeljac, Ž., Frketić, I., Miletić, M., Šoštarić Zadro, A., Bačić, I., ... & Missoni, E. (2014). Blunt Trauma of
Thorax with Subclavian and Axillary Artery Lesion-Case
Report. Collegium antropologicum, 38(3), 1055-1057.
17. Assenza, M., Centonze, L., Valesini, L., Campana, G., Corona,
M., & Modini, C. (2012). Traumatic subclavian arterial rupture: a case report and review of literature. World Journal
of Emergency Surgery, 7(1), 18.
18. Queiroz, R. M., Santana, D. B. F. D., Roque, D., Bernardes
Filho, F., Febronio, E. M., & Valentin, M. V. N. (2018). Blunt
thoracic trauma with the formation of pseudoaneurysm
with the junction of the right subclavian artery. Revista da
Associação Médica Brasileira, 64(11), 987-989.
19. Serrano, J. A., Rodriguez, P., Castro, L., Serrano, P., & Carpintero, P. (2003). Acute subclavian artery pseudoaneurysm
after closed fracture of the clavicle. Acta orthopaedica
belgica, 69(6), 555-557.
20. Derom, A., Ottenheim, S., Raat, H., & van Kleef, J. (2008).
Endovascular treatment of acute subclavian pseudo-aneurysm after fracture of the clavicle. Acta Chirurgica Belgica, 108(4), 441-443.
21. Baikoussis, N. G., Siminelakis, S. N., Matsagas, M., & Michalis, L. K. (2010). Massive haemothorax due to subclavian artery rupture: Emergency thoracotomy or primary
stent-grafting?. Heart, Lung and Circulation, 19(7), 431.
22. Weber, C. D., Kobbe, P., Herren, C., Mahnken, A. H., Hildebrand, F., & Pape, H. C. (2017). Endovascular management
of a combined subclavian and vertebral artery injury in
an unstable polytrauma patient: case report and literature
review. Bulletin of emergency and trauma, 5(1), 53-57.
23. Campfield, B., & Barzideh, O. S. (2016). Clavicular Fracture
Associated with Life-Threatening Hemorrhage: A Case Report. JBJS case connector, 6(2), e31.
24. Yonezawa, N., Nakayama, Y., Takei, T., Toh, M., Asano, M.,
Imamura, T., & Ito, T. (2017). Fatal delayed rupture of
the subclavian artery in a patient with first-rib fracture
caused by blunt trauma. Clinical case reports, 5(3), 260.
25. Cheema, M., Kirton, O. C., Lukose, B., & Gallagher, J. (2008).
Ligation of the subclavian artery after blunt trauma presenting as massive hemothorax. Journal of Trauma and
Acute Care Surgery, 64(4), 1126-1130.
26. Diaz-Gutierrez, I., Rana, M. A., Ali, B., Marek, J. M., & Langsfeld, M. (2017). Hybrid Repair of Complex Left Subclavian Artery Injury with Partial Transection and Complete
Thrombosis in an Unstable Patient following Blunt Trauma. Annals of vascular surgery, 40, 298-e11.
27. Elkbuli, A., Shaikh, S., McKenney, M., & Boneva, D. (2019).
Subclavian artery avulsion following blunt trauma: A case
report and literature review. International journal of surgery case reports, 61, 157-160.
28. Enamorado-Enamorado, J., Egea-Guerrero, J. J., Revuelto-Rey, J., Gordillo-Escobar, E., & Herrera-Melero, C.
(2011). Left subclavian artery pseudoaneurysm after a
traffic accident: a case report. Case reports in critical care,
2011.
29. Nakada, T. A., Idoguchi, K., Fukuma, H., Ono, H., Nakao, S.,
& Matsuoka, T. (2014). Case report: urgent endovascular
treatment of subclavian artery injury after blunt trauma.
F1000Research, 3.
30. Gullo, J., Singletary, E. M., & Larese, S. (2013). Emergency bedside sonographic diagnosis of subclavian artery
pseudoaneurysm with brachial plexopathy after clavicle
fracture. Annals of emergency medicine, 61(2), 204-206.
31. Hirose, H., & Temes, R. T. (2005, December). Acute subclavian artery occlusion by blunt trauma: a case report. In
HEART SURGERY FORUM (Vol. 8, No. 6, p. 360)
32. Ipaktchi, R., Dettmer, S., Vogt, P. M., & Knobloch, K. (2010).
Subclavian artery and jugular vein rupture after a blunt
thoracic trauma due to a BMX handlebar. European journal of cardio-thoracic surgery, 12(1), 235.
33. Jaiswal, L. S., Prasad, J. N., Maharjan, R., & Pandit, N. (2018).
Giant pseudoaneurysm of subclavian artery after blunt
chest trauma. Journal of vascular surgery cases and innovative techniques, 4(3), 220-222.
34. Ostovan, M. A., Kojuri, J., & Dehghani, P. (2017). Endovascular Repair of the Traumatic Dissection of the Subclavian–Axillary Artery: Report of Four Cases. The Journal of
Tehran University Heart Center, 12(2), 88.
35. Kapetanakis, E. I., Sears-Rogan, P., Young, R. S., Kanda, L. T.,
& Ellis, J. L. (2006). Traumatic partial avulsion of a single
right subclavian artery from the aortic arch and definitive
repair. The Annals of thoracic surgery, 81(1), 348-350.
36. Karkos, C. D., Mair, R., Markose, G., Fishwick, G., London,
N. J., & Naylor, A. R. (2007). Hybrid procedures combining
open and endovascular surgical techniques for the management of subclavian artery injuries. Journal of Trauma
and Acute Care Surgery, 63(5), E107-E110.
37. Noh, D., Lee, C. K., Hwang, J. J., & Cho, H. M. (2018). Concomitant avulsion injury of the subclavian vessels and
the main bronchus caused by blunt trauma. The Korean
journal of thoracic and cardiovascular surgery, 51(2), 153.
38. Kluemper, C., Koestner, T., Cowart, J., & Higgins, M. (2018).
Intercostal Entrapment of Clavicle Fracture Causing a
Pulseless, Flaccid Upper Extremity. The Journal of hand
surgery, 43(12), 1143-e1.
39. Knobloch, K., von Falck, C., Teebken, O., & Krettek, C.
(2006). Scapulothoracic dissociation with subclavian artery dissection following a severe motorbike accident. European journal of cardio-thoracic surgery, 30(4), 671-671.
40. Sabbagh, C. N., Chowdhury, M. M., Durrani, A., Van Rensburg, L., Koo, B., & Coughlin, P. A. (2016). A Novel Combined Hybrid Approach to Enable Revascularisation of a
Trauma-Induced Subclavian Artery Injury. EJVES short
reports, 32, 18-20.
41. Mirza, W. R., & Shiraev, T. P. (2018). Endovascular Management of a Left Subclavian Artery Pseudoaneurysm
Secondary to Clavicular Fracture. European Journal of
Vascular and Endovascular Surgery, 55(5), 624.
42. Wan Ismail Faisham, P. M., Juhara, H., Munirah, N. M.,
Shamsulkamaruljan, H., & Ziyadi, G. M. (2011). Clavicle
fracture and subclavian vessels disruption with massive
haemothorax mimic intrathoracic injury. The Malaysian
journal of medical sciences: MJMS, 18(2), 74.
43. Quinones-Baldrich, W. J. (2010). Right subclavian pseudoaneurysm secondary to blunt trauma in an arteriovenous malformation. Journal of vascular surgery, 51(1),
228-229.
44. Gill, I., Quayle, J., & Fox, M. (2013). A low energy paediatric clavicle fracture associated with acute brachial plexus
injury and subclavian artery compression. The Annals of
The Royal College of Surgeons of England, 95(2), e6-e9.
45. Rodriguez-Merchan, E. C., & Gomez-Cardero, P. (2010).
Delayed union of a fracture of the middle third of the clavicle presenting with a late subclavian pseudoaneurysm.
Musculoskeletal surgery, 94(2), 89-92.
46. Scheffler, P., Uder, M., Gross, J., & Pindur, G. (2003). Dissection of the proximal subclavian artery with consecutive
thrombosis and embolic occlusion of the hand arteries
after playing golf. The American journal of sports medicine, 31(1), 137-140.
47. Sodhi, K. S., Arora, J., & Khandelwal, N. (2007). Post-traumatic occlusion of subclavian artery with clavicle fracture.
Journal of Emergency Medicine, 33(4), 419-420.
48. Zaharudin, I., Azizi, Z. A., & Govindarajanthran, N. (2016).
Traumatic right proximal subclavian artery pseudoaneurysm treated with a hybrid procedure: a case report. Med
J Malaysia, 71(4), 221.
49. Tachtsi, M. D., Pitoulias, G. A., Fycatas, P., Kalogirou, T., &
Papadimitriou, D. K. (2011). Subclavian artery aneurysm
due to clavicle fracture. Annals of vascular surgery, 25(7),
984-e5.
50. Tennyson, C., Karunaratne, D., McLaughlin, K. E., Hasan, R.,
& Grant, S. W. (2018). Delayed subclavian artery rupture
secondary to a traumatic first rib fracture. Trauma case
reports, 16, 1.
51. Mandal, A. K. J., Jordaan, J., & Missouris, C. G. (2004). Fractured clavicle and vascular complications. Emergency
medicine journal, 21(5), 648-648.
52. Van Schaik, P. M., de Borst, G. J., Moll, F. L., & Toorop, R. J.
(2015). Late onset acute occlusion of the subclavian artery after clavicle fracture. Vascular, 23(6), 661-662.
53. Watanabe, K., & Matsumura, T. (2005). Late-onset brachial plexus paresis caused by subclavian pseudoaneurysm
formation after clavicular fracture. Journal of Trauma and
Acute Care Surgery, 58(5), 1073-1074.
54. Zhang, M., Yuan, Y., Hu, Y., Zhao, Y., Liu, H., & Lu, H. (2015).
Urgent endovascular treatment of proximal right subclavian artery pseudoaneurysm using kissing technique.
Annals of vascular surgery, 29(6), 1319-e1.
55. Butterworth, S. A., Ng, A. K., Janusz, M. T., & Simons, R. K.
(2001). Great vessel injury after hockey-related trauma:
two case reports and a literature review. Journal of Trauma and Acute Care Surgery, 51(4), 796-799.
56. Sladojevic, M., Markovic, M., Ilic, N., Pejkic, S., Banzic, I.,
Djoric, P., ... & Davidovic, L. (2016). Open Treatment of
Blunt Injuries of Supra-Aortic Branches: Case Series. Annals of vascular surgery, 31, 205-e5.
57. Bukhari, H. A., Saadia, R., & Hardy, B. W. (2007). Urgent
endovascular stenting of subclavian artery pseudoaneurysm caused by seatbelt injury. Canadian journal of surgery, 50(4), 303.
58. Matsumoto, M., Tanemoto, K., Inagaki, E., Hamanaka, S.,
Masaki, H., Nakata, M., ... & Tabuchi, A. (2006). Traumatic
rupture of a right aortic arch in a patient with an aberrant
left subclavian artery. The Journal of thoracic and cardiovascular surgery, 131(2), 464-465.
59. Benedetto, F., La Spada, M., Stilo, F., De Caridi, G., Cotroneo,
A., Passari, G., & Spinelli, F. (2008). Endovascular repair in
atypical traumatic rupture of thoracic aorta. Il Giornale di
chirurgia, 29(10), 427-428.
60. Badmanaban, B., Diver, A., Ali, N., Graham, A. N., McGuigan,
J., & MacGowan, S. (2003). Traumatic aortic rupture during
pregnancy. Journal of cardiac surgery, 18(6), 557-561.
61. Boulate, D., Fabre, D., Langer, N. B., & Fadel, E. (2018).
Ascending aorta, aortic arch and supra-aortic vessels rupture in blunt thoracic trauma. Interactive cardiovascular
and thoracic surgery, 27(2), 304-306.
62. Chock, M. M., Aho, J., Naik, N., Clarke, M., Heller, S., &
Oderich, G. S. (2015). Endovascular treatment of distal
thoracic aortic transection associated with severe thoracolumbar spinal fracture. Vascular, 23(5), 550-552.
63. Coppi, G., Tshomba, Y., Psacharopulo, D., Marone, E. M.,
& Chiesa, R. (2012). Aberrant right subclavian artery in
blunt aortic injury: implication for treatment and review
of the literature. Annals of vascular surgery, 26(6), 861-e1.
64. Eckhauser, A. W., Hannon, D., Molitor, M., Scaife, E., & Gruber, P. J. (2013). Repair of traumatic aortoinnominate disruption using CorMatrix. The Annals of thoracic surgery,
95(4), e99-e101.
65. Waldenberger, P., Fraedrich, G., Mallouhi, A., Jaschke, W. R.,
Perkmann, R., Jung, T., & Czermak, B. V. (2003). Emergency
endovascular treatment of traumatic aortic arch rupture
with multiple arch vessel involvement. Journal of Endovascular Therapy, 10(4), 728-732.
66. Gilani, R., Ochoa, L., Wall Jr, M. J., Tsai, P. I., & Mattox, K.
L. (2011). Endovascular repair of traumatic aortic injury using a custom fenestrated endograft to preserve the
left subclavian artery. Vascular and endovascular surgery,
45(6), 549-552.
67. Gombert, A., Barbati, M. E., Grommes, J., Jalaie, H., Schleimer,
K., Jacobs, M. J., & Kalder, J. (2016). Blunt thoracic aortic
injury in case of a 15-year-old boy: difficulties and possibilities of the endovascular approach. Annals of vascular
surgery, 33, 228-e15.
68. Ryu, Y. G., Choo, S. J., Lim, J. Y., Yoon, H. K., & Chung, C. H.
(2010). Hybrid procedure for a traumatic aortic rupture
consisting of endovascular repair and minimally invasive
arch vessel transposition without sternotomy. Journal of
Korean medical science, 25(1), 142.
69. Ktenidis, K., Lioupis, A., Giannopoulos, A., Ginis, G., & Kiskinis, D. (2012). Management of traumatic aortic isthmus
rupture in case of aberrant right subclavian artery (arteria
lusoria). Annals of vascular surgery, 26(3), 421-e1.
70. Kovari, V. Z., Pecsi, F., Janvari, M. C., & Veres, R. (2017).
Initial experience with the treatment of concomitant aortic pseudoaneurysm and thoracolumbar spinal fracture:
Case report. Trauma case reports, 12, 48-53.
71. Mattison, R., Hamilton Jr, I. N., Ciraulo, D. L., & Richart, C.
M. (2001). Stent-graft repair of acute traumatic thoracic
aortic transection with intentional occlusion of the left
subclavian artery: case report. Journal of Trauma and
Acute Care Surgery, 51(2), 326-328.
72. Moore, R. D., & Brandschwei, F. (2001). Subclavian-to-carotid transposition and supracarotid endovascular stent
graft placement for traumatic aortic disruption. Annals of
vascular surgery, 15(5), 563-566.
73. Murphy, E. H., Dimaio, J. M., Dean, W., Jessen, M. E., & Arko, F.
R. (2009). Endovascular repair of acute traumatic thoracic
aortic transection with laser-assisted in-situ fenestration
of a stent-graft covering the left subclavian artery. Journal
of Endovascular Therapy, 16(4), 457-463.
74. Piffaretti, G., Carrafiello, G., Ierardi, A. M., Mariscalco, G.,
Macchi, E., Castelli, P., ... & Franchin, M. (2015). Thoracic
endovascular aortic repair for blunt thoracic aortic injuries in complex aortic arch vessels anatomies. Annals of
vascular surgery, 29(6), 1320-e11.
75. Patel, K., Allen, K., Hinrichs, C., Jihayel, A., & Donahoo, J. S.
(2002). Traumatic aortic arch injury. The Annals of thoracic surgery, 73(2), 666.
76. Gandhi, S. K., Von Haag, D., Webber, S. A., & Pigula, F. A.
(2003). Traumatic aortic transection in a child with an anomalous right subclavian artery. The Annals of thoracic
surgery, 76(6), 2087-2089.
77. Leshnower, B. G., Litt, H. I., & Gleason, T. G. (2006). Anterior
approach to traumatic mid aortic arch transection. The
Annals of thoracic surgery, 81(1), 343-345.
78. Serna, D. L., Miller, J. S., & Chen, E. P. (2006). Aortic reconstruction after complex injury of the mid-transverse arch.
The Annals of thoracic surgery, 81(3), 1112-1114.
79. Propper, B. W., Alley, J. B., Gifford, S. M., Burkhardt, G. E.,
& Rasmussen, T. E. (2009). Endovascular treatment of a
blunt aortic injury in Iraq: extension of innovative endovascular capabilities to the modern battlefield. Annals of
vascular surgery, 23(5), 687-e19.
80. Reynolds, T. S., Donayre, C. E., Somma, C. G., Poggio, W. G.,
Kim, K. M., Nguyen, T., & White, R. (2011). Endovascular
management of blunt aortic injury with an associated
aberrant right subclavian artery: a report of three cases.
Annals of vascular surgery, 25(7), 979-e7.
81. Siddiqi, M. S., Sharma, A. K., & Sabti, H. A. (2015). Polytrauma to right diaphragm, descending thoracic aorta,
and innominate artery. Asian cardiovascular and thoracic
annals, 23(9), 1075-1078.
82. Thompson, J. K., Reed, A. B., & Giglia, J. S. (2006). Novel
endovascular treatment of blunt thoracic aortic trauma
with a self-expanding stent lined with aortic extender
cuffs. Annals of vascular surgery, 20(2), 271.
83. Turhan, H., Topaloglu, S., Cagli, K., Sasmaz, H., & Kutuk, E.
(2004). Traumatic type B aortic dissection causing near
total occlusion of aortic lumen and diagnosed by transthoracic echocardiography: A case report. Journal of the
American Society of Echocardiography, 17(1), 80-82.
84. Waldenberger, P., Fraedrich, G., Mallouhi, A., Jaschke, W. R.,
Perkmann, R., Jung, T., & Czermak, B. V. (2003). Emergency
endovascular treatment of traumatic aortic arch rupture
with multiple arch vessel involvement. Journal of Endovascular Therapy, 10(4), 728-732.
85. Yeo, D. L. T., Haider, S., & Zhen, C. A. C. (2015). Blunt traumatic aortic injury of right aortic arch in a patient with an
aberrant left subclavian artery. The Yale journal of biology
and medicine, 88(1), 93.
86. Al-khaldi, A., & Robbins, R. C. (2006). Successful repair
of blunt injury of aortic arch branches in the setting of
bovine arch. Journal of vascular surgery, 43(2), 396-398.
87. Dhaliwal, R. S., Luthra, S., Goyal, S., Behra, S., Krishna, R., &
Ba, K. (2005). Traumatic giant pseudoaneurysm of innominate artery. Asian Cardiovascular and Thoracic Annals,
13(4), 369-371.
88. Knosalla, C., Pasic, M., & Hetzer, R. (2000). Traumatic
dissection of the innominate artery. European Journal of
Cardio-Thoracic Surgery, 18(3), 370-370.
89. Hirose, H., & Gill, I. S. (2004). Blunt injury of proximal innominate artery. Annals of thoracic and cardiovascular
surgery, 10(2), 130-132.
90. Hirose, H., & Gill, I. S. (2004). Blunt injury of the innominate artery: a case report and review of literature. Annals
of thoracic and cardiovascular surgery, 10(4), 218-223.
91. Stover, S., Holtzman, R. B., Lottenberg, L., & Bass, T. L.
(2001). Blunt innominate artery injury. The American
surgeon, 67(8), 757.
92. Axisa, B. M., Loftus, I. M., Fishwick, G., Spyt, T., & Bell, P. R.
(2000). Endovascular repair of an innominate artery false
aneurysm following blunt trauma. Journal of Endovascular Therapy, 7(3), 245-250.
93. Ben, S. O., Ben, M. H., Ben, M. M., Kaouel, K., Daoued, Z., &
Khayati, A. (2014). Traumatic dissection of the innominate artery. A case report. Journal des maladies vasculaires, 39(1), 73-76.
94. Bito, Y., Hirai, H., Sasaki, Y., Hosono, M., Nakahira, A., Suehiro, Y., ... & Suehiro, S. (2014). Successful surgical treatment
of traumatic transection of the innominate artery: a case
report. Annals of vascular diseases, 7(2), 165-168.
95. Boutayeb, A., Porcu, P., Pirvu, A., & Chavanon, O. (2014).
Post-traumatic injury of the brachiocephalic artery: onpump beating heart repair. Heart, Lung and Circulation,
23(10), e226-e228.
96. Davidović, L., Ilić, N., Cvetković, S., Koncar, I., Čolić, M., &
Vjestica, M. (2011). Blunt injury of the innominate artery
and left innominate vein. Vascular, 19(4), 223-225.
97. Dias-Neto, M., Ramos, J. F., & Teixeira, J. F. (2018). Blunt
Injury of the Innominate Artery: What Surprises to Expect? A Case Report. Vascular and endovascular surgery,
52(3), 226-232.
98. Miles EJ, Blake A, Thompson W, Jones WG, Dunn EL.
(2003). Endovascular repair of acute innominate artery
injury due to blunt trauma. Am Surg, 68(2), 155-159.
99. Howea KL, Guirgisa G, Woodmana G, Chub GF, Cooperc
MJ,Rapanosa T, Szalay D. (2017). Blunt innominate artery
trauma requiring repair and carotid ligation. Trauma Case
Reports, 12, 24–27
100. Huang C, Kao H. (2008). Endovascular Management of
Post-Traumatic Innominate Artery Transection With
Pseudo-Aneurysm Formation. Catheterization and Cardiovascular Interventions, 72, 569–572
101. Lee CW, Song S, Choi SU, Kim SH, Lee HC. (2015). Hybrid
Repair for Anastomotic Pseudoaneurysm on the Innominate Artery Following Blunt Chest Trauma. J Card Surg,
30, 836–838
102. Mousa AY, Batsides GP, RV Todd. (2010). Delayed presentation of traumatic innominate artery injury. J Vasc Surg,
51, 1014
103. Ormazabal A, Muangman N, Eric J. (2012). SternManubrial Fracture with an Associated Innominate Artery Injury:
Curr Probl Diagn Radiol, 41(4), 122-123
104. Chu MWA, Myers ML. (2006). Traumatic Innominate Artery Disruption and Aortic Valve Rupture. Ann Thorac
Surg, 82:1095–7
105. Roberts CS, Sadoff JD, White DR. (2000). Innominate Arterial Rupture Distal to Anomalous Origin of Left Carotid
Artery. Ann Thorac Surg, 69, 1263-4
106. Symbas JD, Halkos ME, Symbas PN. (2005). Rupture of the
Innominate Artery from Blunt Trauma: Current Options
for Management. J Card Surg, 20, 455-459
107. Sturm JT, Dorsey JS, Oslon FR, Perry JF. (1984). The management of Subclavian artery injuries following blunt
thoracic trauma. The annals of thoracic surgery, 38(3),
188-191
108. Katras T, Baltazar U, Rush DS, Davis D, Bell TD, Browder
IW, Compton RP, Stanton PE. (2001). Subclavian arterial
injury associated with blunt trauma. Vascular surgery,
35, 43-50
109. Costa MC, Robbs JV. (1988). Non penetrating Subclavian
artery trauma. Journal of vascular surgery, 8(1): 71-75
110. Road safety annual report 2018: International transport
forum. https://www.itf-oecd.org/sites/default/diles/
docs/irtad-road-safety-annual-report-2018_2.pdf
111. Gombert A, Barbati ME, Storck M, Kotelis D, Keschenau P,
Pape H, Andruszkow H, Lefering R, Hilderbrand F, Greiner
A, Jacobs MJ, Grommes J. (2017). Treatment of blunt thoracic aortic injury in Germany-Assessment of the TraumaRegister DGU, 12(3), 1-12
112. Burkhart HM, Gomez GA, Jacobson LE, Pless JE, Broadie TA.
(2001). Fatal blunt aortic injuries: A review of 242 autopsy
cases. J Trauma, 50, 113-115
113. Mirvis SE, Shanmuganathan K, Miller BH, White CS, Turney
SZ. (1996). Traumatic aortic injury: Diagnosis with contrast-enhanced CT-Five year experience of a major trauma
center. Radiology, 200(2), 413-422
114. Williams JS, Graff JA, Uku JM, Steining JP. (1995). Aortic
injury in vehicular trauma. Ann Thorac Surg, 57, 726-730c.
115. Starnes BW, Lundgren RS, Gunn M, Quade S, Hatsukami
TS, Tran NT, Mokadam N, Aldea G. (2012). A new classification scheme for treating blunt aortic injury. J vasc surg,
55(1), 47-54