Open Access | Research article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
The Results of a Long-Term Follow-up of Bilateral Single Port Sympathicotomy in Primary Hyperhidrosis: Should We Perform This Surgery?
*Corresponding author: Timuçin ALAR
Mailing address: Department of Thoracic Surgery, Çanakkale Onsekiz Mart University Medical Faculty, Çanakkale Onsekiz Mart
Universitesi Tıp Fakultesi Gogus Cerrahisi Anabilim Dalı Terzioglu
Girisi, Çanakkale,17100,Turkey.
Email: tmalar@yahoo.com
Received: 24 October 2019 Accepted: 25 November 2019
DOI: 10.31491/CSRC.2019.12.041
Abstract
Background: Hyperhidrosis (HH), which refers to excessive sweating of the body in response to temperature or emotional stimuli rather than physiological stimuli, can adversely affect quality of life. In this prospective study, we investigated the long-term effects, development of complications, and patient satisfaction among those who underwent bilateral single-port endoscopic thoracic sympathecotomy (ETS) for HH.
Methods: Thirty-one patients who underwent bilateral single-port endoscopic thoracic sympathicotomy (ETS) for HH between January 200 and November 2014 were enrolled in this study. The patients wer1e followed up until July 2017. Patient satisfaction in terms of the primary complaint (PC) and complications, such as compensatory hyperhidrosis (CH), in the short and long term were recorded.
Results: The mean follow-up period was 60.6 ± 12.8 (min: 40, max: 89) mo postoperatively. When both the short- and long-term results were evaluated together, CH had no effect on patient satisfaction. However, persistence of the PC in both the short (p = 0.020) and long term (p = 0.001) had a significant effect on satisfaction.
Conclusion: The most important factor affecting patient satisfaction was PC persistence. Thus, further studies should be performed to enlighten this complication. even though it may remit with time. Whether ETS is a permanent treatment that cannot successfully treat PC, possible complications and the ability to cope with them will seem to be open to debate as the most important issues that surgeons will have to face in the near future.
Keywords
Complication; hyperhidrosis; surgery; sympathicotomy
Introduction
Hyperhidrosis (HH) can be described as excessive
sweating of the body that exceeds physiological needs
[1]. Hyperhidrosis may be primary or secondary. Primary HH is the result of to overactivity of the sympathetic
nervous system, whereas secondary HH is caused by
various factors, such as malignancies, endocrine disorders (e.g., thyrotoxicosis), and some medications [1-3].
Primary HH affects facial, palmar, axillary, and plantar
regions of the body, exhibiting regional and symmetrical
involvement patterns due to sympathetic nervous system overactivity [1,2].
Hyperhidrosis may be treated via medical or surgical approaches. Endoscopic thoracic sympathecotomy (ETS)
is the most commonly used type of surgical treatment
today. The surgery can be performed in a variety of ways,
such as dissecting the sympathetic chain in the thoracic
region, thermal damage via electrocautery, or clipping.
Among various ETS-related complications, which include a hemo-pneumothorax, Horner’s syndrome, and
bradycardia, the most important in terms of both patient
and physician satisfaction is compensatory hyperhidrosis (CH) [4,5].
In this prospective study, we investigated the rate of
complications, such as CH, and PC persistence in the
long-term postoperative period following bilateral single port ETS and the effects of these complications on
patient satisfaction.
Methods
Patients who had undergone single port ETS between
January 2010 and November 2014 at Çanakkale Onsekiz
Mart University Medical Faculty Thoracic Surgery Clinic
were prospectively followed up until July 2017. During
outpatient clinical examinations and telephone interviews, the patients were questioned about changes in
CH and their PC in the postoperative period and their
satisfaction with the operation.
In the 6 mo prior to the single port ETS, all the patients
had received medical treatment. Despite this treatment,
none of the patients experienced improvements in their
PC. Prior to surgery, informed consent was obtained
from each patient. In patients with HH affecting multiple
areas, only the area most affected was treated. The ETS
was performed using a 10-mm 0-degree thoracoscope
(Karl Storz 26034 AA) with a 6-mm working channel
under general anesthesia via a double-lumen endotracheal tube. After the patient had been positioned in the
lateral decubitus position, a single thoracoport (width:
10.5 mm) was inserted into the thorax through a single incision of 11 mm at the intersection of the fourth
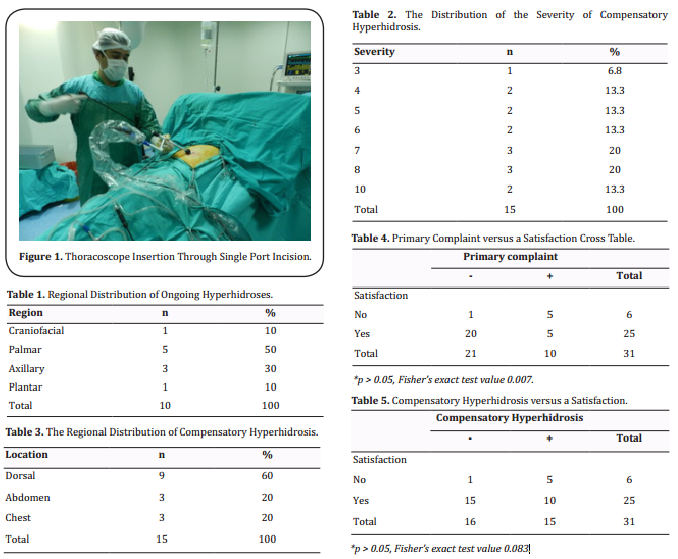
intercostal space and mid-axillary line (Figure 1). The
sympathetic chain was cauterized by endoscopic electrocautery from the T2 for fascial hyperhidrosis, T3 for
palmar hyperhidrosis, T4 for axillary hyperhidrosis,
and T5 for plantar hyperhidrosis. In addition, during
the sympathecotomy of the T2-T3, the presence of the
nerve of Kuntz was verified, and the nerve tissue was
cauterized. The rib bed was cauterized laterally for an
additional 2 cm to allow the dissection of possible bypassing nerve fibers. After hemorrhage control, the air
in the pleural cavity was evacuated via a small catheter.
The incision line was closed by subcutaneous suturing,
and the same procedure was repeated on the other side.
On the postoperative first day, the patients were evaluated by a physical examination, posterior-anterior
chest X-ray, hemogram, and blood biochemistry tests.
Patients whose physical examination and examination
results revealed no abnormalities were discharged from
the hospital on the first postoperative day. The patients
were referred to the outpatient clinic on the seventh
postoperative day and reevaluated via a physical examination and posterior-anterior chest X-ray. In the third
postoperative month and again in the third postoperative year, all the patients were interviewed by telephone.
They were questioned about their HH status, CH status,
and satisfaction with the operation. They were asked to
rate their HH at the site of the PC from 0 to 10, where 0
represented no sweating, and 10 represented the most
severe sweating.
The follow-up times were from the date of the operation to the last follow-up date (July 2017), expressed in
months. Subsequently, cutoff values at 48, 60, and 72 mo
were coded as a dichotomous variable for those below
and above the follow-up period. The following parameters were coded as dichotomous variables: CH, PC, and
patient satisfaction. In terms of the latter, on the day of
the interview, the patients were asked whether, given
the choice, they would undergo the surgery again. The CH and PC intensities were coded as continuous variables ranging from 1 to 10.
The data were then transferred to a digital medium. The
normal distribution matching of the continuous variables was examined for the frequency and distribution
of variables. The relations between the continuous variables were analyzed using appropriate correlation tests,
and the relations between the dichotomous variables
were analyzed using a chi-square test and, if necessary,
Fisher’s exact test. In all the analyses, statistical significance was accepted as a p-value of < 0 .05. The absolute
p values are given for the analysis results.
Results
Thirty-one patients who underwent bilateral single
port ETS at Çanakkale Onsekiz Mart University Medical Faculty Chest Surgery Clinic between January 2010
and November 2014 were included in the study. Sixteen
(51.6%) of the patients were males, and 15 (48.4%)
were females. The mean age of the patients was 24.13 ±
4.64 (min: 13, max: 34) y. In terms of the site of the PC,
it was craniofacial in 6.5% (n = 2) of cases, palmar-facial
in 12.9% (n = 4) of cases, palmar in 67.7% (n = 21) of
cases, axillary in 9.7% (n = 3) of cases, and palmoplantar
in 3.2% (n = 1) of cases.
The postoperative complications were a pneumothorax
in one patient and a hemopneumothorax in one patient.
Tube thoracostomy was performed in the patient who
developed a hemopneumothorax, and air evacuation via
thoracentesis was performed in the other patient. All the
other patients were discharged on the first postoperative day. Thus, the average duration of the hospital stay
was 1.13 ± 0.56 (min: 1, max: 4) d. The mean follow-up
period was 60.6 ± 12.8 (min: 40, max: 89) mo postoperatively.
When the patients were questioned about their PC status, 10 (32.3%) of the 31 patients responded that their PC was not resolved. The remaining 21 cases responded that their PC was in remission. Among patients with
a persistent PC, the most frequent site was palmar HH
(Table 1).
When the patients were asked about their CH status in
the postoperative third-month, 15 (48.4%) of the 31
patients reported that they had developed CH. When
questioned about the severity of the CH, the severity
ranged from 3–10, with the most frequent CH site being
the dorsal region (Tables 2 and 3).
At the time of the final interview in July 2017, the patients were questioned about their satisfaction with the
surgery. Six (19%) of the 31 patients were dissatisfied
with the surgery, and 81% of patients were satisfied. Five
of the six (83%) patients who were not satisfied with the
surgery had developed CH, and the PC was unresolved in
five of these six (83%) cases (Tables 4 , 5). In total, seven patients indicated that if given the choice today, they
would not have the surgery. Two of these seven patients
developed CH postsurgery, and the PC was unresolved
in the other five cases. One patient who was satisfied
with the surgery reported that he would not undergo
this surgery today. This patient had some relief from his
PC, but it was not completely resolved.
When the long-term follow-up of the cases was examined, the PC was resolved in two patients, and CH developed in three patients. In total, there were 8 (25%) cases
of PC persistence and 18 (58%) cases of CH persistence.
Persistence of the PC affected patient satisfaction in both
the short (p = 0.007) and long term (p = 0.001). In contrast, CH had no effect on patient satisfaction in either
the short (p = 0.083) or long term (p = 0.359).
Discussion
Although the precise pathophysiological mechanism in
HH is not known, excessive stimulation of thermoregulatory and emotional sweating control centers or excessive secretion of acetylcholine by the sympathetic nervous system in response to stimulation of these centers
may play a role [3]. Individuals with primary HH, which
usually begins in childhood or adolescence, generally
consult a physician because of psychosocial problems
caused by HH [6].
Medical therapy options for HH include topical or systemic antiperspirants, iontophoresis, botulinum toxin
injections, laser therapy, and microwave therapy[6]. Topical antiperspirant agents consist of a 20% solution of
aluminum hydrochloride [7]. Topical and systemic forms
of anticholinergics include glycopyrrolate and oxybutynin [7]. Iontophoresis is the treatment of choice for
palmoplantar HH. The treatment is based on the principle that the palmoplantar zone is kept in tap water
in which a low voltage electrical current is applied for
about 30 min [8,9]. Botulinum toxin A injections are used
as a treatment for both palmoplantar and axillary HH.
These provide a longer remission time than any other
medical treatment, with remission of HH for about 6 mo post-treatment [10]. In terms of laser treatment, a neodynium yttrium aluminum garnet laser is used for HH [11]. In
microwave therapy, thermolysis of eccrine sweat glands
is conducted. The main difference of this method is that
it is irreversible [12]. The main disadvantage of medical
treatments for HH as compared to surgical treatment is
that medical therapy offers only a temporary solution
to an ongoing problem, and the treatments have to be
repeated. An important advantage of medical therapy
versus surgical treatment is the absence of CH, which is
a complication of surgery. For this reason, all HH patients
are advised to receive medical treatment for at least 6
mo before considering surgery. If the medical treatment
is unsuccessful, with success defined as patient satisfaction, surgery is an option. In the present study, none of
the patients had satisfactory outcomes prior to undergoing surgery.
CH, a complication of ETS, refers to excessive sweating
affecting various parts of the bodys. The mechanism underlying the development CH is not known. Although
some authors have argued that this condition develops
because of negative feedback stimuli of the sympathetic
chain cannot reach the hypothalamus, there is no scientific evidence to support this hypothesis [13,14]. Approximately 3–98% of patients develop CH after ETS, and it
is most commonly observed in the trunk area. It is not
possible to predict who may develop CH and how severe
it may become [4,5,13,15]. Although some studies showed
that a sympathecotomy at the T2 level or a sympathectomy at multiple levels and older age increased the risk
of developing CH, other studies contradicted these findings [13,16-18]. In our study, in the short term, the rate of
CH was 48%, whereas it was 58% in the long term. CH
developed most commonly in the trunk region, similar
to the scientific literature on this subject.
Previous research reported that the development of CH
and PC persistence were the two most important factors affecting patient satisfaction after ETS operations.
In the literature, the reported rates of PC persistence
range from 0 to 21.4% [13,17,19]. The rates in the present
study were comparable to those found in the literature,
with rates of 32% in the short-term follow up and 25%
in the long-term follow up. An interesting finding in the
present study was that PC persistence was the most important factor affecting patient satisfaction in the long
term.
In previous studies on HH, the postoperative follow-up
period was less than 1 y, with most follow-ups lasting
approximately 6 mo. Thus, knowledge is limited on the
status of HH among these patients over the long term.
In the present study, the patients were followed up for
a mean of 60 mo. As shown by the results, an increase
in the rate of CH did not increase patient satisfaction. In
contrast, while a decrease in PC was observed, there was
also a decrease in the patient satisfaction. Thus, the most
important factor affecting patient satisfaction was continuation of the PC in contrast to our current knowledge.
According to a previous study, the results of intermittent
unilateral ETS for reducing CH, which affects patient satisfaction in the short term, are promising, although the
duration of the follow-up in the study was only 1 y [20].
However, the hospital costs associated with intermittent
unilateral ETS seem to be disadvantages, with the procedure requiring two surgeries, two anesthesia sessions,
and two hospitalizations. We believe that the primary
goal of surgery should be complete resolution of the PC.
Self-remission of the PC with age should also be seen as
a disadvantage for the ETS [21]. The possibility that the
PC may regress in time, combined with the fact that PC
persistence rather than CH affects patient satisfaction,
casts doubts on the feasibility of ETS for HH.
The present study has some limitations. The number
of cases (N = 31) may be considered low as compared
with that in other studies on ETS. In addition, we did
compare the ETS method with medical treatment methods in terms of patient satisfaction. Furthermore, we did
not use standardized questionnaires to assess quality
of life and patient satisfaction with ETS. Thus, the answers we obtained in our interviews may be considered
“subjective.” As with all forms of “satisfaction,” the term
“patient satisfaction” is subjective. The development of
standardized questionnaires on quality of life and patient satisfaction with ETS would improve the objectivity
of patient responses.
Conclusion
For HH, ETS is the only treatment that has been proven to be successful in the long term. The two most important factors affecting patient satisfaction after ETS are the continuation of the PC and CH. Intermittent unilateral ETS may be considered an alternative surgical approach for CH, although the likelihood of CH may increase in the long term. Furthermore, the PC of HH may regress with age. This treatment should be described as temporary (at least until the end of the adolescence period) rather than permanent. The decision whether to perform this surgery is up to the surgeon. However, the decision whether to be treated with surgery for HH should be the patients after all these data have been conveyed.
Declaration
Authors’ contributions
Made substantial contributions to conception and design of the study and performed data analysis and interpretation: Alar T and Gedik İ E.
Performed data acquisition, as well as provided administrative, technical, and material support: Alar T and Gedik İ E.
Conflicts of interest
All authors declare that there are no conflicts of interest.
References
1. Smith, F. C. T. (2013). Hyperhidrosis. Surgery, 31,251-255
2. Stefaniak, T. J., and Ćwigoń, M. (2013). Long-term results
of thoracic sympathectomy for primary hyperhidrosis.
Pol Przegl Chir, 85,247-252
3. Stashak, A-B., Brewer, J. D. (2014). Management of Hyperhidrosis. Clinical, Cosmetic and Investigational Dermatology, 7,285–299
4. Drott, C., Gothberg, G., and Claes, G. (1995). Endoscopic
transthoracic sympathectomy: an efficient and safe method for the treatment of hyperhidrosis. J Am Acad Dermatol, 33,78-78
5. Chwajol, M., Barrenechea, I. J., Chakraborty, S., Lesser, J. B.,
Connery, C. P., and Perin, N. I. (2009). Impact of compensatory hyperhidrosis on patient satisfaction after endoscopic thoracic sympathectomy. Neurosurgery, 64,511-518
6. Brown, A. L., Gordon, J., and Hill, S. (2014). Hyperhidrosis:
review of recent advances and new therapeutic options
for primary hyperhidrosis. Curr Opin Pediatr, 26,460–465
7. Wozniacki, L., and Zubilewicz, T. (2009). Primary hyperhidrosis controlled with oxybutynin after unsuccessful
surgical treatment. Clin Exp Dermatol, 34,e990-991
8. Ozcan, D., and Güleç, A. T. (2014). Compliance with tap
water iontophoresis in patients with palmoplantar hyperhidrosis. J Cutan Med Surg, 18,109-113
9. Siah, T. W., and Hampton, P. J. (2013). The effectiveness of
tap water iontophoresis for palmoplantar hyperhidrosis
using a Monday, Wednesday, and Friday treatment regime. Dermatol Online J, 19,14
10. Lecouflet, M., Leux, C., Fenot, M., Célerier, P., and Maillard,
H. (2014). Duration of efficacy increases with the repetition of botulinum toxin A injections in primary palmar
hyperhidrosis: A study of 28 patients. J Am Acad Dermatol, 70,1083-1087
11. Letada, P. R., Landers, J. T., Uebelhoer, N. S., and Shumaker,
P. R. (2012). Treatment of focal axillary hyperhidrosis using a long pulsed Nd: YAG 1064 nm laser at hair reduction
settings. J Drugs Dermatol, 11,59–63
12. Hong, H. C., Lupin, M., O’Shaughnessy, K. F. (2012). Clinical evaluation of a microwave device for treating axillary
hyperhidrosis. Dermatol Surg, 38,728-735
13. Cai, S., Huang, S., An, J., Li, Y., Weng, Y., Liao, H., Chen, H., Liu,
L., He, J., and Zhang, J. (2014). Effect of lowering or restricting sympathectomy levels on compensatory sweating. Clin
Auton Res, 24,143–149
14. Chou, S. H., Kao, E. L., Lin, C. C., Chang, Y. T., Huang, M. F.
(2006). The importance of classification in sympathetic
surgery and a proposed mechanism for compensatory
hyperhidrosis: experience with 464 cases. Surg Endosc,
20,1749–1753
15. Waseem, M, Hajjar., Sami, A, Al-Nassar., Heba, M, Al-Sharif., Dana, M. Al-Olayet., Wejdan, S, Al-Otiebi., Alanoud, A,
Al-Huqayl., Adnan, W, Hajjar. (2019). The quality of life and
satisfaction rate of patients with upper limb hyperhidrosis
before and after bilateral endoscopic thoracic sympathectomy Saudi J Anaesth, 13,16–22
16. Baumgartner, F. J., Reyes, M., Sarkisyan, G. G., Iglesias,
A., Reyes, E. (2011). Thoracoscopic sympathicotomy for
disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg,
92,2015–2019
17. Aoki, H., Sakai, T., Murata, H., Sumikawa, K. (2014). Extent
of sympathectomy affects postoperative compensatory
sweating and satisfaction in patients with palmar hyperhidrosis. J Anesth, 28,210–213
18. Licht PB, Pilegaard HK. (2004). Severity of compensatory
sweating after thoracoscopic sympathectomy. Ann Thorac
Surg, 78,427–431
19. Delaplace, M., Dumont, P., Lorette, G., Machet, L., Lagier, L.,
Maruani, A., Samimi, M. (2015). Factors associated with
long-term outcome of endoscopic thoracic sympathectomy for palmar hyperhidrosis: a questionnaire survey in
a cohort of French patients. Br J Dermatol, 172,805-807
20. Youssef, T., Soliman, M. (2015). Unilateral Sequential Endoscopic Thoracic Sympathectomy for Palmar Hyperhidrosis: A Proposed Technique to Overcome Compensatory
Hyperhidrosis and Improve Plantar Hyperhidrosis. Journal of Laparoendoscopic & Advanced Surgical Techniques
, 2,370-374
21. Callejas, M. A., Grimalt, R., Cladellas, E. (2010). Hyperhidrosis Update. Actas Dermosifiliogr, 101,110-118