Open Access | Research article
This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Posterior Approach Combined with Thoracic Intervertebral Foramen Posterior Wall Opening and Spinal Reconstruction for Complex Thoracic Intervertebral Foramen Lesions: a Single-Centre Experience
*Corresponding author: Prof. Ren-Ya Zhan
Mailing address: Department of Neurosurgery, the First Affiliated Hospital, Zhejiang University, China.
E-mail: 1196057@zju.edu.cn
Received: 20 March 2019 Accepted: 22 May 2019
DOI: 10.31491/CSRC.2019.03.030
Abstract
Background: Thoracic intervertebral foramen (TIF) lesions were really difficult to expose through posterior or transforaminal approaches. There was no effective treatment strategy, especially for complex ones.
Methods: Between 2013 and 2015, 22 patients presenting with complex TIF lesions underwent posterior approach combined with TIF posterior wall opening and spinal reconstruction were retrospectively reviewed. After ascertaining the precise location of complex TIF lesions, incisions should allow for exposure of the lesion’s adjacent vertebral pedicle screw entry point. The adjacent pair of vertebral lamina and spinous processes is typically removed in a single piece, such that the intra-spinal section can be fully exposed. The posterior wall of the TIF is subsequently opened, allowing the intra-TIF and extra-spinal sections to be sufficiently exposed. Subsequently, spinal reconstruction at the appropriate level is required. When the ventral spinal column is intact, dorsal reconstruction is typically performed using the screw and rod fixation technique (SRFT). After the dorsal surface of the spine has been burnished, the removed vertebral lamina and spinous process are rendered granular to allow reconstruction of the TIF and fusion of adjacent vertebrae.
Results: All patients presenting with complex TIF lesions were successfully treated with this approach. No patient had experienced any complications arising from SRFT use. No patient suffered intraspinal infection, incision splits, or CSF leakage in the short-term (between 1 and 3 months) or fixation loosening or spinal instability in the long-term (6–24 months). Imaging studies confirmed that the TIF and spinal reconstruction outcomes were favorable.
Conclusion: A posterior approach combined with TIF posterior wall opening and spinal reconstruction is a rapid, effective, and reliable method in the treatment of complex TIF lesions. This technique can provide total lesion resection while reconstructing spinal stability.
Keywords
posterior approach; thoracic intervertebral foramen (TIF); intervertebral articular process (IAP); spinal reconstruction; screw and rod fixation technique (SRFT)
Introduction
Pancreatic cancer (PC) is one of the most aggressive cancer with high lethality. It was estimated the 5-year survival rate of PC is 6%, and the mortality rate is almost equal to the incident rate [1]. The risk factors of PC are included in the smoking, obesity, family history, as well as the enviroDuring the treatment of thoracic intervertebral foramen (TIF) lesions, such as schwannoma and nerve sheath cysts, the ultimate goal of surgery is to achieve complete resection. However, achieving this using posterior approach combined with transforaminal or transthoracic approach is problematic [1-3]. In dumbbell-shaped schwannomas, piecemeal excision of tumor, using a combined posterior and transforaminal approach, typically results in incomplete tumor resection and destruction of the intervertebral articular process (IAP), leading to poor neurological outcome and impaired spinal stability. Consequently, the goal in modern surgical management of complex TIF lesions is to achieve total lesion resection and spinal reconstruction [4-6].
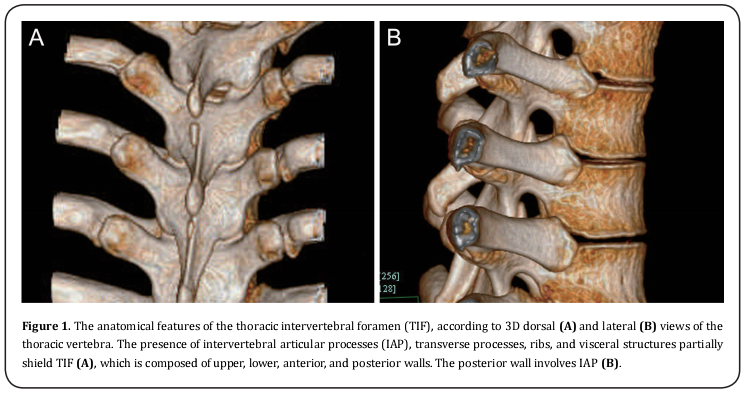
Due to the high rates of morbidity, virtually all anatomical studies have been concerned with the cervical intervertebral foramen (CIF) [7-10]and lumbar intervertebral foramen (LIF) [11-14]. Meanwhile, many authors have reported favorable outcomes when treating complex CIF or LIF lesions using anterior, posterior, or transforaminal approaches[15-17]. Although the anatomical characteristics of TIF are similar to CIF or LIF, careful attention is required for the following reasons: 1) the thoracic spinous process is imbricate; 2) the thoracic canal is very narrow; 3) the IAP is difficult to identify; and 4) the vertebral transverse process, and ribs, partially shield the foramen (Figure 1) [18]. All of these considerations preclude the use of traditional approaches aimed to identify and completely expose the TIF.
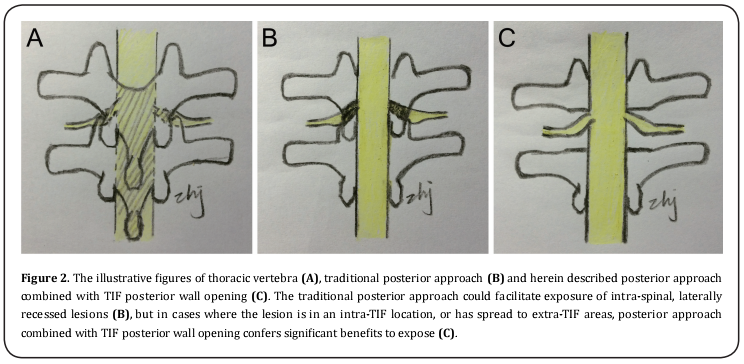
The posterior approach, combined with TIF posterior wall opening (Figure 2C), allows for complete complex TIF lesion resection in conjunction with fixation techniques and TIF reconstruction in a subsequent procedure. We herein describe the operational steps involved in treating complex TIF lesions, using a posterior approach combined with TIF posterior wall opening, to achieve favorable neurological and spinal outcomes.
Patient and Methods
Patient Selection and General Information
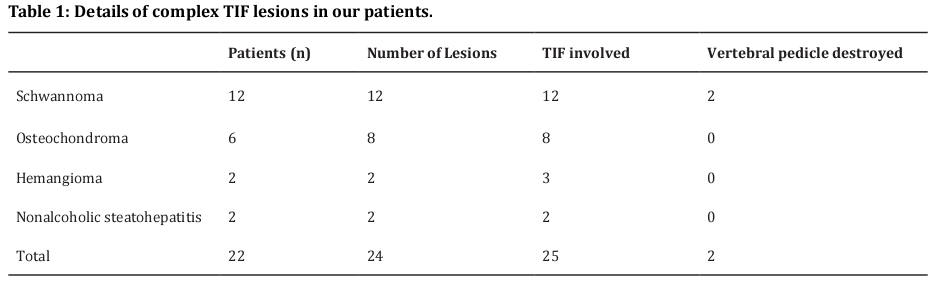
Between 2013 and 2015, 22 patients presenting with complex TIF lesions underwent total resection and spinal reconstruction at the First Affiliated Hospital, College of Medicine, Zhejiang University (Hangzhou, China). Ten of the patients were female, and twelve were male. Patients ranged between 28 and 72 years of age (mean age = 45 years). No patient had a history of spinal surgery. The details of the complex TIF lesions of our patients are provided in Table 1. In total, 22 patients with 24 lesions underwent 25 TIF posterior wall-opening procedures. All of the TIF lesions were dilated to some degree. Twelve patients were diagnosed with dumbbell-shaped schwannomas, of whom two presented with a destroyed vertebral pedicle. Six patients were diagnosed with nerve sheath cysts, of which one exhibited two nerve sheath cysts at bilateral TIF lesions of the same level (Figure 5A). One patient presented with two nerve sheath cysts at different levels of the homolateral TIF. Two patients were diagnosed with osteochondroma, one of whom had a lesion surrounding a pedicle of vertebral arch involving two adjacent TIFs. The lesion grew posteriorly to the exterior of the lamina (Figure 3A-B). Two patients were diagnosed with TIF hemangioma. The opened TIF was reconstructed in these patients using fixation techniques and bone grafting. Screws and rods were used in the spinal reconstruction of all patients. No patient developed intraspinal infection, incision splits, or cerebrospinal fluid (CSF) leakage in the short-term (between 1 and 3 m), and 16 patients had no fixation loosening or spinal instability in the long-term (between 6 and 24 m).
Anatomical Considerations and Operative Nuances
The vertebral notches of adjacent vertebrae constitute TIF (i.e., the porous channel of spinal nerve roots departing from the spinal cord). It is composed of upper, lower, anterior, and posterior walls. The upper and lower walls represent vertebral pedicle notches; the anterior wall involves the lateral vertebra, intervertebral disc, and posterior longitudinal ligament, whereas the posterior wall involves IAP (Figure 1) [19]. The corresponding nerve root is surrounded by cellular tissue and small blood vessels at the point at which it passes through the foramen; the interior section is laterally recessed [20]. The presence of IAP, transverse processes, ribs, and visceral structures nearby to the lesion, poses significant challenges to radical lesion excision in the TIF.
The posterior approach towards complex TIF lesions involves ascertaining the precise location, and subsequently confirming it with pre-operative computed tomography (CT), magnetic resonance imaging (MRI), and intraoperative mobile x-ray. Incisions should allow for exposure of the lesion’s adjacent vertebral pedicle screw entry point. Following reconfirmation of the lesion’s location, the adjacent pair of vertebral lamina and spinous processes is typically removed in a single piece, such that the intra-spinal section can be fully exposed. The posterior wall of the TIF is subsequently opened using a high-speed drill, allowing the intra-TIF and extra-spinal sections to be sufficiently exposed.
Although certain complex TIF lesions can be resected using a posterior approach combined with transforaminal
or transthoracic approach, this method is inconvenient
and often render total resection difficult (see Illustrative
Cases, Sec. 3) [1-3]. We favor a posterior approach combined with TIF posterior wall opening (Figure 2C), which
is particularly useful when the lesion is located nearby
to the TIF. The main advantage that this method offers
is complete lesion resection and spinal reconstruction
in a single incision and direction, thereby reducing the
length of the overall operation.
For complex TIF lesions, spinal reconstruction at the
appropriate level is required. When the ventral spinal column is intact, dorsal reconstruction is typically
performed using the screw and rod fixation technique
(SRFT). After the dorsal surface of the spine has been
burnished, the removed vertebral lamina and spinous
process are rendered granular to allow reconstruction
of the TIF and fusion of adjacent vertebrae.
Illustrative Cases
Patient 1
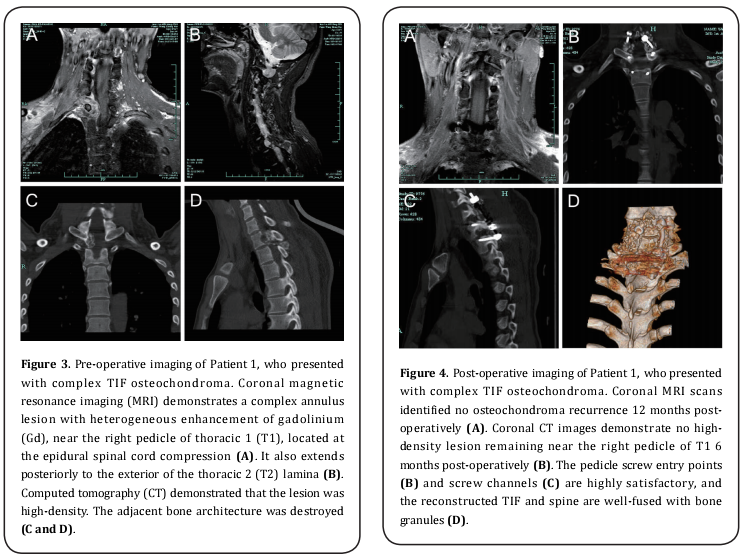
A 37-year-old man presented with numbness and weakness of the right upper extremity, for 1 week, principally in the ulnaris ring finger and little finger. CT and MRI scans of his cervical spine were obtained. CT imaging demonstrated an annulus high-density lesion near the right pedicle of thoracic 1 (T1), involving C7/ T1 and T1/T2 foramen, and leading to spinal stenosis.This lesion also extended posteriorly to the exterior of the T2 lamina (Figure 3C-D). MRI scans demonstrated a complex annulus lesion with heterogeneous enhancement of gadolinium (Gd) near the right pedicle of T1. This lesion extended outward from the right C7/T1 and T1/T2 foramen to the right posterior mediastinum, which also extended posteriorly to the exterior of the T2 lamina (Figure 3A-B). Electromyogram (EMG) revealed that the motor-evoked potential (MEP) and sensory-evoked potential (SEP) of the right ulnar nerve were impaired. Based upon these observations, multiple osteochondromas were considered, and the patient was offered a posterior approach combined with C7/T1 and T1/T2 right intervertebral foramen posterior wall opening to achieve complete resection of the lesion. Spinal reconstruction was achieved using C6/T1/T2 SRFT, and bone granules were implanted to reconstruct the TIF and fuse the adjacent vertebrae. The patient was discharged 8 days post-surgery without any neurological dysfunction. Over the subsequent 15 months, the patient’s incision remained dry, with no fixation loosening or spinal instability. A CT scan obtained 6 months post-surgery revealed that the reconstructed spine was well-fused with the bone granules (Figure 4B-D). MRI indicated no osteochondroma recurrence 12 months post-operatively (Figure 4A). The patient has remained asymptomatic.
Patient 2
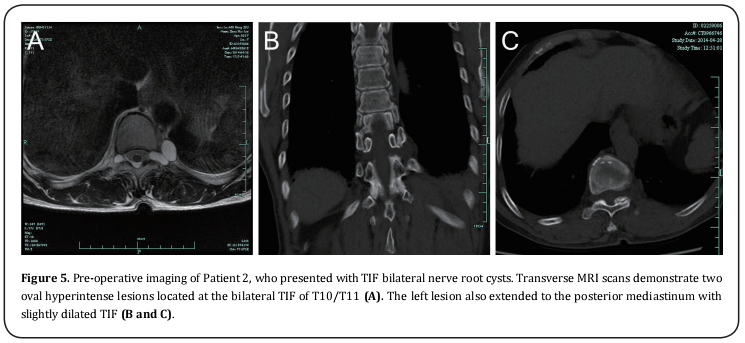
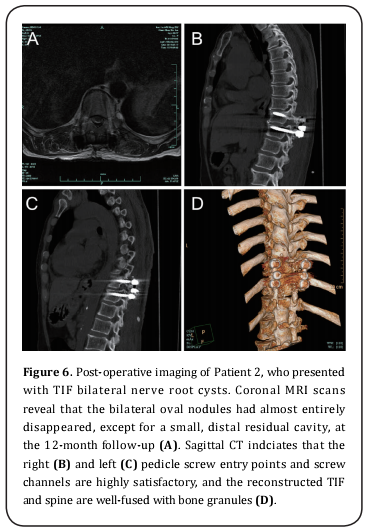
A 64-year-old woman presented with belt-like numbness and pain in the back and abdomen for 10 months. Bilateral navel levels were principally involved. CT and MRI scans of the thoracal spine were obtained. MRI scans revealed two ovals, hyperintense lesions located at the bilateral TIF of T10/T11 (Figure 5A). CT imaging revealed two ovals, iso-hypodense nodules located at the bilateral TIF of T10/T11; the bilateral TIF were slightly dilated (Figure 5B-C). Systemic workup using whole-spine MRI did not reveal any additional lesions. Based upon these observations, bilateral nerve sheath cysts were considered, and the patient was offered a posterior approach to seal the ventage of the bilateral T10 nerve in the intradural direction. The T10/T11 bilateral intervertebral foramen posterior walls were subsequently opened, and the bilateral nerve sheath cysts were completely aspirated by syringe. Spinal reconstruction was performed using T10/T11 SRFT, and bone granules were implanted to reconstruct the TIF and fuse the adjacent vertebrae. The patient was discharged 7 days post-surgery without any neurological dysfunction. During the following 12 months, the patient’s incision healed well, exhibiting ideal bone fusion and spinal stability. A CT scan obtained 6 months post-operatively indicated that the reconstructed spine was well-fused with bone granules (Figure 6B-D). MRI revealed that the bilateral oval nodules had almost disappeared, except for a small, distal residual cavity (Figure 6A). The patient remains in a healthy condition.
Results
Between 2013 and 2015, 22 patients were successfully treated using a posterior approach combined with TIF posterior wall opening, for total resection and spinal reconstruction. Diagnoses were made according to physical examination, and CT and MRI scans. At the time that this manuscript was written, no patient had experienced any complications arising from SRFT use. Furthermore, no patient suffered intraspinal infection, incision splits, or CSF leakage in the short-term (between 1 and 3 months) or fixation loosening or spinal instability in the long-term (6–24 months). Imaging studies confirmed that the TIF and spinal reconstruction outcomes were favorable (Figure 4 and 6).
Discussion
Based on the anatomical and biomechanical characteristics of thoracic vertebra, degenerative disease is extremely rare, and few researches concerning TIF has been previously conducted [18-20]. The use of a traditional posterior approach could facilitate exposure of intra-spinal, laterally recessed lesions (Figure 2B), but in cases where the lesion is in an intra-TIF location, or has spread to extra-TIF areas, this becomes problematic; we refer to such cases as complex TIF lesions. Partial intra-TIF lesions can be dragged using an angled nerve hook, but nerve root injuries and/or CSF leakage present a significant challenge. Partial, extra-TIF lesions could be exposed in conjunction with a transforaminal approach, but the presence of IAP, transverse processes, and ribs represents a significant obstacle. Certain lesions involving the posterior mediastinum should be subsequently resected in combination with a transthoracic approach [18].
However, all of these procedures are relatively inconvenient, and in certain complex cases, a satisfactory resolution is not possible. A posterior approach combined with TIF posterior wall opening, confers significant benefits in such cases. Patient 1 presented with a complex annulus lesion near the right pedicle of T1, involving the right C7/T1 and T1/T2 foramen. The lesion’s hard texture and special location, rendered transforaminal or transthoracic approaches impractical. Patient 2 presented with bilateral intra-TIF nerve sheath cysts at T10/T11. Following the sealing of the bilateral T10 nerve ventage, bilateral cysts should be aspirated to relieve nerve root compression; however, the bilateral IAP obstructs this procedure. In both cases, highly satisfactory results were obtained when the TIF posterior wall was opened. Despite certain large extra-TIF lesions growing in a forward direction, the ribs and transverse processes were amenable to additional expansion (costotransversectomy) to achieve full exposure and resection. Our method simplifies the surgical procedure, and shortens the number of hospital days. Furthermore, all 22 patients achieved a satisfactory clinical outcome.
SRFT is a common technique in spinal surgery. When complex TIF lesions are resected using our method, the IAP is destroyed and spinal instability, or spinal cord compression, will manifest at long-term follow-up. Spinal reconstruction and bone fusion has resolved this problem and therefore complements our method. Although SRFT may increase medical costs, it represents a rapid, effective, and reliable method of reconstructing the spine, and is thus clinically useful for patients with complex TIF lesions.
What’s more, many neurosurgeons, especially in China are lack of spinal anatomic knowledge and training course. Our method could on one side benefits these patients, on the other encourage more neurosurgeons to learn spinal anatomy and spinal fixation technique, so as to engage in more comprehensive spine operations.
Conclusion
We describe a posterior approach, combined with TIF posterior wall opening, to treat complex TIF lesions. SRFT is a rapid, effective, and reliable method of reconstructing the spine while preserving its physiological stability. Post-operatively, patients recover without further complications. Although SRFT is a high-cost method, it is clinically useful for patients with complex TIF lesions and good method for neurosurgeons to learn more about spine.
References
1. Shadmehr, M. B., Gaissert, H. A., Wain, J. C., Moncure, A.
C., Grillo, H. C., Borges, L. F., and Mathisen, D. J. (2003)
The surgical approach to "dumbbell tumors" of the
mediastinum. Ann Thorac Surg 76, 1650-1654
2. Grillo, H. C., Ojemann, R. G., Scannell, J. G., and Zervas, N. T.
(1983) Combined approach to "dumbbell" intrathoracic
and intraspinal neurogenic tumors. Ann Thorac Surg 36,
402-407
3. Ricci, C., Rendina, E. A., Venuta, F., Pescarmona, E. O.,
and Gagliardi, F. (1990) Diagnostic imaging and surgical
treatment of dumbbell tumors of the mediastinum. Ann
Thorac Surg 50, 586-589
4. Agrawal, A., Srivastava, S., Joharapurkar, S. R., Gharde,
P., and Ubeja, G. (2008) Single stage complete excision
of large thoracic dumbbell schwannoma by modified
posterior approach. Surg Neurol 70, 432-436
5. Kim, M. S., Eun, J. P., and Park, J. S. (2011) A dumbbellshaped meningioma mimicking a schwannoma in the
thoracic spine. J Korean Neurosurg Soc 50, 264-267
6. Rzyman, W., Skokowski, J., Wilimski, R., Kurowski, K., and
Stempniewicz, M. (2004) One step removal of dumb-bell
tumors by postero-lateral thoracotomy and extended
foraminectomy. Eur J Cardiothorac Surg 25, 509-514
7. Ebraheim, N. A., An, H. S., Xu, R., Ahmad, M., and Yeasting, R.
A. (1996) The quantitative anatomy of the cervical nerve
root groove and the intervertebral foramen. Spine (Phila
Pa 1976) 21, 1619-1623
8. Panjabi, M. M., Maak, T. G., Ivancic, P. C., and Ito, S. (2006)
Dynamic intervertebral foramen narrowing during
simulated rear impact. Spine (Phila Pa 1976) 31, E128-
134
9. Takasaki, H., Hall, T., Jull, G., Kaneko, S., Iizawa, T., and
Ikemoto, Y. (2009) The influence of cervical traction,
compression, and spurling test on cervical intervertebral
foramen size. Spine (Phila Pa 1976) 34, 1658-1662
10. Tominaga, Y., Maak, T. G., Ivancic, P. C., Panjabi, M.
M., and Cunningham, B. W. (2006) Head-turned rear
impact causing dynamic cervical intervertebral foramen
narrowing: implications for ganglion and nerve root
injury. J Neurosurg Spine 4, 380-387
11. Cinotti, G., De Santis, P., Nofroni, I., and Postacchini,
F. (2002) Stenosis of lumbar intervertebral foramen:
anatomic study on predisposing factors. Spine (Phila Pa
1976) 27, 223-229
12. Arslan, M., Comert, A., Acar, H. I., Ozdemir, M., Elhan, A.,
Tekdemir, I., Tubbs, R. S., and Ugur, H. C. (2012) Nerve root
to lumbar disc relationships at the intervertebral foramen
from a surgical viewpoint: An anatomical study. Clin Anat
25, 218-223
13. Min, J. H., Kang, S. H., Lee, J. B., Cho, T. H., and Suh, J. G.
(2005) Anatomic analysis of the transforaminal ligament
in the lumbar intervertebral foramen. Neurosurgery 57, 37-41; discussion 37-41
14. Spivak, J. M., Kummer, F. J., Chen, D., Quirno, M., and
Kamerlink, J. R. (2010) Intervertebral foramen size and
volume changes in low grade, low dysplasia isthmic
spondylolisthesis. Spine (Phila Pa 1976) 35, 1829-1835
15. Habal, M. B., McComb, J. G., Shillito, J., Jr., Eisenberg, H.
M., and Murray, J. E. (1972) Combined posteroanterior
approach to a tumor of the cervical spinal foramen.
Technical note. J Neurosurg 37, 113-116
16. Osman, S. G., Nibu, K., Panjabi, M. M., Marsolais, E. B.,
and Chaudhary, R. (1997) Transforaminal and posterior
decompressions of the lumbar spine. A comparative study
of stability and intervertebral foramen area. Spine (Phila
Pa 1976) 22, 1690-1695
17. Park, J. S., Shirachi, I., Sato, K., Ando, N., and Nagata, K.
(2005) Lipoma with dumb-bell extradural extension
through the intervertebral foramen into the spinal canal.
Case report. J Neurosurg Spine 2, 69-71
18. Pait, T. G., Elias, A. J., and Tribell, R. (2002) Thoracic,
lumbar, and sacral spine anatomy for endoscopic surgery.
Neurosurgery 51, S67-78
19. Panjabi, M. M., O'Holleran, J. D., Crisco, J. J., 3rd, and
Kothe, R. (1997) Complexity of the thoracic spine pedicle
anatomy. Eur Spine J 6, 19-24
20. Kothe, R., O'Holleran, J. D., Liu, W., and Panjabi, M. M.
(1996) Internal architecture of the thoracic pedicle. An
anatomic study. Spine (Phila Pa 1976) 21, 264-270